Establishing Computational Model Credibility: Standards, Applications, and Best Practices for Biomedical Research
This article provides a comprehensive guide to the standards and practices for establishing credibility in computational models, with a specific focus on applications in drug development and medical device innovation.
Establishing Computational Model Credibility: Standards, Applications, and Best Practices for Biomedical Research
Abstract
This article provides a comprehensive guide to the standards and practices for establishing credibility in computational models, with a specific focus on applications in drug development and medical device innovation. It explores the foundational principles of risk-based credibility frameworks like ASME V&V 40 and FDA guidance, detailing methodological steps for verification, validation, and uncertainty quantification. The content further addresses common implementation challenges—including data quality, model bias, and talent shortages—and offers troubleshooting strategies. Finally, it examines comparative validation approaches and the evolving role of in silico trials, equipping researchers and professionals with the knowledge to build trustworthy models for regulatory submission and high-impact decision-making.
The Bedrock of Trust: Core Principles and Regulatory Frameworks for Model Credibility
In the development of drugs and medical devices, computational modeling and simulation (CM&S) have become critical tools for evaluating safety and effectiveness. The credibility of these models is paramount, especially when they are used to inform high-stakes regulatory decisions. Model credibility is broadly defined as the trust, established through the collection of evidence, in the predictive capability of a computational model for a specific context of use [1] [2]. Establishing this trust requires a systematic, evidence-based approach.
Two primary frameworks have emerged to guide this process: the U.S. Food and Drug Administration (FDA) guidance document, "Assessing the Credibility of Computational Modeling and Simulation in Medical Device Submissions," and the American Society of Mechanical Engineers (ASME) V&V 40 standard, "Assessing Credibility of Computational Modeling through Verification and Validation: Application to Medical Devices" [3] [4]. The FDA guidance provides a risk-informed framework for regulatory submissions, while the ASME V&V 40 standard offers a detailed engineering methodology. This guide objectively compares these frameworks, detailing their applications and the experimental protocols required to demonstrate model credibility.
Comparative Analysis of Credibility Frameworks
The following table summarizes the core characteristics of the FDA and ASME frameworks, highlighting their shared principles and distinct focuses.
Table 1: Core Framework Comparison: FDA Guidance vs. ASME V&V 40 Standard
| Feature | FDA Guidance | ASME V&V 40 Standard |
|---|---|---|
| Primary Purpose | Regulatory recommendations for medical device submissions [3] [5]. | Engineering standard for establishing model credibility [4] [1]. |
| Scope of Application | Physics-based, mechanistic models for medical devices [3] [5]. | Computational models for medical devices; principles adapted for other areas like drug development [1] [6]. |
| Core Methodology | Risk-informed credibility assessment framework [3]. | Risk-informed credibility assessment framework [1]. |
| Defining Element | Context of Use (COU): A detailed statement defining the specific role and scope of the model [3] [1]. | Context of Use (COU): A detailed statement defining the specific role and scope of the model [1]. |
| Risk Assessment Basis | Combination of Model Influence (on decision) and Decision Consequence (of an error) [1]. | Combination of Model Influence (on decision) and Decision Consequence (of an error) [1] [6]. |
| Key Output | Guidance on evidence needed for a credible regulatory submission [3]. | Goals for specific Credibility Factors (e.g., code verification, validation) [1]. |
| Regulatory Status | Final guidance for industry and FDA staff (November 2023) [3]. | Consensus standard; recognized and utilized by the FDA [1]. |
The FDA guidance and ASME V&V 40 standard are highly aligned, with the ASME standard providing the foundational, technical methodology that the FDA guidance adapts for the regulatory review process [7] [1]. The core principle shared by both is that the level of evidence required to demonstrate a model's credibility should be commensurate with the model risk [1] [6]. This means that a model supporting a critical decision with significant patient impact requires more rigorous evidence than one used for exploratory purposes.
The Risk-Based Credibility Assessment Workflow
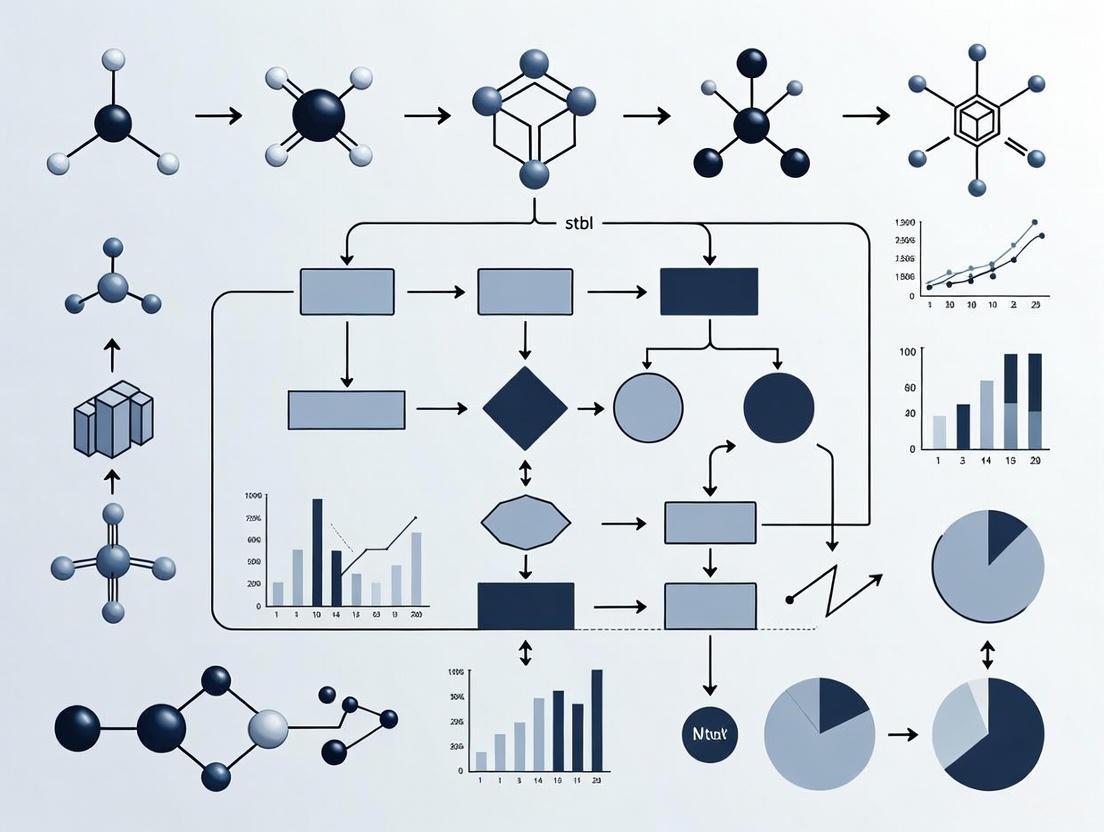
Both frameworks operationalize the risk-based approach through a structured workflow. The diagram below illustrates the key steps, from defining the model's purpose to assessing its overall credibility.
Diagram 1: Credibility Assessment Workflow
Defining Context of Use and Risk Assessment
The process begins by precisely defining the Context of Use (COU), a detailed statement of the specific role and scope of the computational model in addressing a question of interest [1] [6]. For example, a COU could be: "The PBPK model will be used to predict the effect of a moderate CYP3A4 inhibitor on the pharmacokinetics of Drug X in adult patients to inform dosing recommendations" [6].
The COU directly informs the model risk assessment, which is a function of two factors:
- Model Influence: The contribution of the computational model relative to other evidence in making a decision (e.g., supportive vs. primary evidence) [1] [6].
- Decision Consequence: The significance of an adverse outcome resulting from an incorrect decision based on the model [1] [6].
The following table illustrates how different combinations of these factors determine the overall model risk, using examples from medical devices and drug development.
Table 2: Model Risk Assessment Matrix with Application Examples
| Decision Consequence | Low Model Influence | High Model Influence |
|---|---|---|
| Low | Low Risk: Model for internal design selection, with low impact on patient safety. | Moderate Risk: Model used as primary evidence to waive in vitro bioequivalence study for a low-risk drug. |
| High | Moderate Risk: Model supports, but is not primary for, a clinical trial design for a ventricular assist device [1]. | High Risk: Model used as primary evidence to replace a clinical trial for a high-risk implant or to set pediatric dosing [1] [6]. |
Credibility Factors and Validation Activities
The model risk drives the rigor required for specific credibility factors, which are elements of the verification and validation (V&V) process [1]. The following table lists key credibility factors and examples of corresponding validation activities, with data from a centrifugal blood pump case study [1].
Table 3: Credibility Factors and Corresponding Experimental Validation Activities
| Credibility Factor | Experimental Validation Activity | Example from Blood Pump Case Study [1] |
|---|---|---|
| Model Inputs | Characterize and quantify uncertainty in input parameters. | Use validated in vitro tests to define blood viscosity and density for fluid dynamics model. |
| Test Samples | Ensure test articles are representative and well-characterized. | Use a precise, manufactured prototype of the pump for validation testing. |
| Test Conditions | Ensure experimental conditions represent the COU. | Perform experiments at operating conditions (flow rate, pressure) specified in the COU (e.g., 2.5-6 L/min, 2500-3500 RPM). |
| Output Comparison | Compare model outputs to experimental data with a defined metric. | Compare Computational Fluid Dynamics (CFD)-predicted hemolysis levels to in vitro hemolysis measurements using a pre-defined acceptance criterion. |
| Applicability | Demonstrate relevance of validation activities to the COU. | Justify that in vitro hemolysis testing is a relevant comparator for predicting in vivo hemolysis. |
Detailed Experimental Protocols for Model Validation
This section provides a detailed methodology for key experiments used to generate validation data, as referenced in the credibility factors above.
In Vitro Hemolysis Testing for Blood Pump Validation
Purpose and Principle: This test is designed to quantify the level of red blood cell damage (hemolysis) caused by a blood pump under controlled conditions. It serves as a critical comparator for validating computational fluid dynamics (CFD) models that predict hemolysis [1]. The principle involves circulating blood through the pump under specified operating conditions and measuring the release of hemoglobin.
Protocol Workflow: The experimental sequence for hemolysis validation is methodical, proceeding from system preparation to data analysis.
Diagram 2: In Vitro Hemolysis Testing Protocol
Key Reagents and Materials:
- Fresh Heparinized Blood: Typically bovine or porcine blood; provides the biological substrate for measuring shear-induced damage. The hematocrit should be adjusted to a standardized level (e.g., 30%±2%) [1].
- PBS (Phosphate Buffered Saline): Used for priming the flow loop and diluting blood samples; prevents clotting and cell lysis from osmotic shock prior to testing.
- Centrifuge: Critical for separating plasma from blood cells after sample collection, enabling accurate measurement of plasma-free hemoglobin.
- Spectrophotometer: Instrument used to measure the concentration of free hemoglobin in plasma by detecting absorbance at specific wavelengths (e.g., 540 nm).
Data Analysis: The primary output is the Normalized Index of Hemolysis (NIH), which is calculated based on the increase in plasma-free hemoglobin, the total hemoglobin content in the blood, the test flow rate, and the duration of the test [1]. This normalized value allows for comparison across different test setups and conditions.
PBPK Model Validation for Drug-Drug Interactions
Purpose and Principle: Physiologically-Based Pharmacokinetic (PBPK) models are used in drug development to predict pharmacokinetic changes, such as those caused by drug-drug interactions (DDIs). The credibility of a PBPK model is established by assessing its predictive performance against observed clinical data [6].
Protocol Workflow: The validation of a PBPK model is an iterative process of building, testing, and refining the model structure and parameters.
Diagram 3: PBPK Model Development and Validation Workflow
Key Reagents and Materials:
- In Vitro System Data: Data from experiments like human liver microsome or transfected cell assays to quantify enzyme kinetics (e.g., Km, Vmax) for the drug of interest [6].
- Clinical PK Data: Observed concentration-time data from early-phase clinical trials in humans; used for model calibration and refinement before the final validation step.
- Independent Clinical DDI Study Data: Data from a dedicated drug-drug interaction clinical study not used in model development; serves as the primary comparator for final model validation [6].
- PBPK Software Platform: A qualified and verified software tool (e.g., GastroPlus, Simcyp, PK-Sim) used to implement the mathematical model and perform simulations.
Data Analysis: Validation involves a quantitative comparison of PBPK model predictions to observed clinical data. Standard pharmacokinetic parameters like Area Under the Curve (AUC) and maximum concentration (Cmax) are compared. Predictive performance is typically assessed by calculating the fold-error of the prediction and checking if it falls within pre-specified acceptance criteria (e.g., within 1.25-fold or 2-fold of the observed data) [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key materials and their functions for conducting the experiments essential to model validation.
Table 4: Essential Research Reagents and Materials for Credibility Evidence Generation
| Item | Function in Credibility Assessment |
|---|---|
| Particle Image Velocimetry (PIV) | An optical experimental method used to measure instantaneous velocity fields in fluids. It serves as a key comparator for validating CFD-predicted flow patterns and shear stresses in medical devices like blood pumps [1]. |
| Human Liver Microsomes | Subcellular fractions containing drug-metabolizing enzymes (e.g., CYPs). Used in in vitro assays to generate kinetic parameters for drug metabolism, which are critical model inputs for PBPK models [6]. |
| Standardized Blood Analog Fluid | A solution with optical and viscous properties matching human blood. Used in in vitro flow testing (e.g., for PIV) to provide a safe, reproducible, and well-characterized fluid that represents key biological properties [1]. |
| Qualified PBPK Software Platform | Commercial or proprietary software used to build and simulate PBPK models. The platform itself must undergo code verification and software quality assurance to ensure it solves the underlying mathematics correctly [6]. |
| Clinical Bioanalytical Assay (LC-MS/MS) | A validated method (e.g., Liquid Chromatography with Tandem Mass Spectrometry) for quantifying drug concentrations in biological samples. It generates the high-quality clinical PK data used as a comparator for PBPK model validation [6]. |
The journey toward establishing model credibility is a structured, evidence-driven process guided by the complementary frameworks of the FDA guidance and the ASME V&V 40 standard. The core takeaway is that credibility is not a one-size-fits-all concept; it is a risk-informed judgment where the required evidence is proportional to the model's impact on decisions related to patient safety and product effectiveness [3] [1]. Success hinges on the precise definition of the Context of Use and the execution of targeted verification and validation activities—ranging from mesh refinement studies to in vitro hemolysis tests and clinical DDI studies—to generate the necessary evidence. As computational models take on more significant roles, including enabling In Silico Clinical Trials, the rigorous and transparent application of these credibility standards will be foundational to gaining the trust of regulators, clinicians, and patients [7].
The Centrality of Context of Use (COU) in Risk-Based Assessment
In computational science, the Context of Use (COU) is a formal statement that defines the specific role, scope, and objectives of a computational model within a decision-making process [1] [8]. This concept is foundational to modern risk-based credibility assessment frameworks, which posit that the evidence required to trust a model's predictions should be commensurate with the risk of an incorrect decision impacting patient safety or public health [1] [8] [9]. As computational models transition from supporting roles to primary evidence in regulatory submissions for medical devices and pharmaceuticals, establishing model credibility through a structured, risk-informed process has become essential [1] [10] [8].
The American Society of Mechanical Engineers (ASME) V&V 40 subcommittee developed a pioneering risk-informed framework that directly links the COU to the required level of model validation [1]. This framework has been adapted across multiple domains, including drug development and systems biology, demonstrating its utility as a standardized approach for establishing model credibility [11] [8]. The core principle is that a model's COU determines its potential influence on decisions and the consequences of those decisions, which collectively define the model risk and corresponding credibility requirements [1].
The Risk-Based Framework: From COU to Credibility
Core Components of the Assessment Framework
The risk-based credibility assessment framework involves a systematic process with clearly defined steps and components. The table below outlines the key terminology essential for understanding this approach.
Table 1: Core Terminology in Risk-Based Credibility Assessment
| Term | Definition | Role in Credibility Assessment |
|---|---|---|
| Context of Use (COU) | A detailed statement defining the specific role and scope of a computational model in addressing a question of interest [1] [8]. | Serves as the foundational document that frames all subsequent credibility activities. |
| Model Influence | The degree to which the computational model output influences a decision, ranging from informative to decisive [1]. | One of two factors determining model risk. |
| Decision Consequence | The potential severity of harm resulting from an incorrect decision made based on the model [1] [9]. | One of two factors determining model risk. |
| Model Risk | The possibility that using a computational model leads to a decision resulting in patient harm. It is the combination of model influence and decision consequence [1]. | Directly drives the level of evidence (credibility goals) required. |
| Credibility Factors | Elements of the verification and validation (V&V) process, such as conceptual model validation or operational validation [1]. | The specific V&V activities for which evidence-based goals are set. |
| Credibility Goals | The target level of evidence needed for each credibility factor to establish sufficient trust in the model for the given COU [1]. | The final output of the risk analysis, defining the evidentiary bar. |
The Sequential Assessment Workflow
The following diagram visualizes the standard workflow for applying the risk-based credibility framework, from defining the COU to the final credibility assessment.
Comparative Analysis: COU-Driven Credibility Requirements
Case Study: Computational Fluid Dynamics in a Blood Pump
The ASME V&V 40 standard illustrates the profound impact of COU using a hypothetical computational fluid dynamics (CFD) model of a generic centrifugal blood pump [1]. The model predicts flow-induced hemolysis (red blood cell damage), but the required level of validation changes dramatically based on the pump's clinical application.
Table 2: Impact of COU on Credibility Requirements for a Centrifugal Blood Pump Model [1]
| Context of Use (COU) Element | COU Scenario 1:\nCardiopulmonary Bypass (CPB) | COU Scenario 2:\nVentricular Assist Device (VAD) |
|---|---|---|
| Clinical Application | Short-term cardiopulmonary bypass surgery (hours) | Long-term ventricular assist device (years) |
| Device Classification | Class II | Class III |
| Model Influence | Informs safety assessment, but not the sole evidence | Primary evidence for hemolysis safety assessment |
| Decision Consequence | Low; temporary injury if hemolysis occurs | High; potential for severe permanent injury or death |
| Resulting Model Risk | Low | High |
| Credibility Goal for Validation | Low: Comparison with a single in-vitro hemolysis dataset may be sufficient. | High: Requires rigorous validation against multiple, high-quality experimental datasets under various operating conditions. |
This comparison demonstrates that the same computational model requires substantially different levels of validation evidence based solely on changes to its COU. For the high-risk VAD application, the consequence of an incorrect model prediction is severe, justifying the greater investment in comprehensive validation [1].
Cross-Domain Application of the Framework
The risk-informed principle pioneered by ASME V&V 40 has been successfully adapted to other fields, including drug development and systems biology.
Table 3: Application of Risk-Informed Credibility Assessment Across Domains
| Domain | Framework/Initiative | Role of COU | Key Application |
|---|---|---|---|
| Medical Devices | ASME V&V 40 [1] | Central driver of model risk and credibility goals. | CFD models for blood pump hemolysis, fatigue analysis of implants. |
| Drug Development | Model-Informed Drug Development (MIDD) [12] [8] | Defines the "fit-for-purpose" application of quantitative models. | Physiologically-Based Pharmacokinetic (PBPK) models for dose selection, trial design. |
| Systems Biology | Adapted credibility standards [11] | Informs the level of reproducibility and annotation required for a model to be trusted. | Mechanistic subcellular models used for drug target identification. |
| AI/ML Medical Devices | Alignment with MDR/ISO 14971 [9] | Determines the clinical impact of model errors (e.g., false negatives vs. false positives). | Image-based diagnosis classifiers (e.g., for cancer detection). |
In drug development, the "fit-for-purpose" paradigm mirrors the risk-based approach, where the selection and evaluation of Model-Informed Drug Development (MIDD) tools are closely aligned with the COU and the model's impact on development decisions [12]. For AI/ML-based medical devices, the COU is critical for understanding the clinical impact of different types of model errors, necessitating performance metrics that incorporate risk rather than relying solely on standard accuracy rates [9].
Experimental Protocols for Establishing Credibility
The credibility of a computational model is established through rigorous Verification and Validation (V&V) activities. The specific protocols are tailored to meet the credibility goals set by the risk analysis.
Protocol for a High-Risk CFD Model (e.g., VAD Blood Pump)
For a high-risk model, such as the CFD model for a Ventricular Assist Device, a comprehensive V&V protocol is required.
1. Verification
- Code Verification: Ensure the computational solver (e.g., ANSYS CFX) correctly implements the underlying mathematical equations. This involves solving problems with known analytical solutions [1].
- Calculation Verification: Estimate the numerical accuracy of the specific simulation (e.g., for a blood pump). This includes performing a mesh refinement study to ensure results are independent of the discretization of the geometry [1].
2. Validation
- Objective: Demonstrate that the model accurately represents the real-world physics. This is done by comparing model predictions with experimental data.
- Experimental Comparator: In-vitro hemolysis testing using a blood analog fluid in a mock circulatory loop [1].
- Key Metrics: The Modified Index of Hemolysis (MIH) is calculated from experimental measurements and compared to the hemolysis index predicted by the CFD model.
- Acceptance Criterion: The model's prediction of the MIH must fall within a pre-defined agreement margin (e.g., ±20%) of the experimental measurements across the pump's operating range. The strictness of this margin is dictated by the model risk [1].
The workflow for this protocol is detailed below.
Protocol for a Low-Risk or Informational Model
For a model with low influence and consequence, the V&V process may be substantially reduced. The focus may be on conceptual model validation, where the underlying assumptions and model structure are reviewed by subject matter experts, with limited or no quantitative validation against physical data required [1].
The following table details key resources and methodologies that support the development and credibility assessment of computational models across different domains.
Table 4: Essential Research Reagents and Solutions for Computational Modeling
| Tool/Resource | Function/Purpose | Relevance to Credibility |
|---|---|---|
| ASME V&V 40 Standard | Provides the authoritative framework for conducting risk-informed credibility assessment [1]. | The foundational methodology for linking COU and risk to V&V requirements. |
| Systems Biology Markup Language (SBML) | A standardized XML-based format for representing computational models in systems biology [11]. | Ensures model reproducibility and interoperability, a prerequisite for credibility. |
| MIRIAM Guidelines | Define minimum information for annotating biochemical models, ensuring proper metadata [11]. | Supports model reusability and understanding, key factors in long-term credibility. |
| PBPK/PD Modeling Software (e.g., GastroPlus, Simcyp) | Tools for developing mechanistic Physiologically-Based Pharmacokinetic/Pharmacodynamic models [12]. | Used in MIDD to generate evidence for regulatory submissions; credibility is assessed via a fit-for-purpose lens. |
| In-vitro Hemolysis Test Loop | A mock circulatory loop for measuring hemolysis in blood pumps under controlled conditions [1]. | Serves as the source of experimental comparator data for validating high-risk CFD models. |
| ISO 14971 Standard | The international standard for risk management of medical devices [9]. | Provides the overall risk management process into which the risk-based evaluation of an AI/ML model is integrated. |
The Context of Use is the central pillar of a modern, risk-based approach to computational model credibility. It is the critical starting point that determines the model's risk profile and, consequently, the requisite level of evidence from verification and validation activities. As demonstrated across medical devices, drug development, and AI/ML, a disciplined application of this COU-driven framework ensures that models are fit-for-purpose, resources are allocated efficiently, and regulatory decisions are based on a justified level of trust. This structured approach is essential for harnessing the full potential of computational modeling to advance public health while safeguarding patient safety.
Understanding the ASME V&V 40 Risk-Informed Credibility Framework
In the development of pharmaceuticals and medical devices, computational modeling and simulation (CM&S) has become a critical tool for accelerating design, informing decisions, and supporting regulatory submissions. The credibility of these models—the trust in their predictive capability for a specific context—is paramount, particularly when they influence high-stakes regulatory and patient-care decisions [6] [5]. Several standards have been developed to guide the credibility assessment process. The ASME V&V 40 framework, specifically tailored for medical devices, provides a risk-informed approach for determining the necessary level of model confidence [1] [4]. Other influential standards include those from NASA, which focus on broad engineering and physical science models, and various systems biology standards (like SBML and MIRIAM) that ensure the reproducibility and unambiguous annotation of biological models [2]. This guide objectively compares the ASME V&V 40 standard with these alternative approaches, detailing their applications, experimental protocols, and the evidence required to establish model credibility.
Comparative Analysis of Credibility Frameworks
The following table summarizes the core objectives, primary application domains, and key characteristics of three major approaches to computational model credibility.
Table 1: Comparison of Major Computational Model Credibility Frameworks
| Framework Characteristic | ASME V&V 40 (2018) | NASA Standards | Systems Biology Standards |
|---|---|---|---|
| Primary Scope & Objective | Risk-based credibility for medical device CM&S [1] | Quality assurance for computational models in engineering & physical science [2] | Reproducibility & reusability of biological models [2] |
| Core Application Domain | Physics-based/mechanistic medical device models [3] [5] | Aerospace, mechanical engineering [2] | Mechanistic, subcellular biological systems [2] |
| Governance & Recognition | FDA-recognized standard; developed by ASME [13] [3] | Developed by NASA for internal and partner use [2] | Community-driven (e.g., SBML, CellML, MIRIAM) [2] |
| Defining Principle | Credibility effort is commensurate with model risk [1] | Rigorous, generalized quality assurance for simulation [2] | Standardized model encoding, annotation, and dissemination [2] |
| Key Artifacts/Outputs | Credibility Assessment Plan & Report; VVUQ evidence [1] | Model quality assurance documentation [2] | Annotated model files (SBML, CellML); simulation results [2] |
Core Methodology of the ASME V&V 40 Framework
The ASME V&V 40 framework introduces a structured, risk-informed process to establish the level of evidence needed for a model to be deemed credible for its specific purpose. The workflow is not a one-size-fits-all prescription but a logical sequence for planning and executing a credibility assessment.
Figure 1: The ASME V&V 40 Credibility Assessment Workflow
Detailed Experimental Protocol for Applying the Framework
The following steps outline the protocol for executing a V&V 40-compliant credibility assessment, as demonstrated in applications ranging from heart valve analysis to centrifugal blood pumps [13] [1].
- Define the Question of Interest: Articulate the specific question, decision, or concern the study aims to address. This question may be broader than the model's immediate use.
- Define the Context of Use (COU): Create a detailed statement specifying the role, scope, and applicable boundaries of the computational model in addressing the question. This includes defining the quantities of interest the model will predict [6] [1].
- Assess Model Risk: Model risk is a combination of:
- Decision Consequence: The significance of an adverse outcome from an incorrect decision. This is often tied to patient impact [1].
- Model Influence: The contribution of the computational model relative to other evidence in the decision-making process [6] [1]. This risk assessment directly dictates the rigor of subsequent V&V activities.
- Establish Credibility Goals: For each of the 13 credibility factors (e.g., code verification, model input accuracy, output comparison), define specific, measurable goals. The stringency of these goals is determined by the model risk [1].
- Gather V&V Evidence: Execute the planned verification, validation, and uncertainty quantification activities. This involves using comparator data (e.g., from benchtop or clinical studies) to validate the model's outputs [13] [6].
- Assess Overall Credibility: A team of experts reviews the collected evidence against the pre-defined credibility goals to determine if the model is sufficiently credible for the stated COU [1].
- Document and Report: The entire process, rationale, and results are documented to provide a transparent record for internal review or regulatory submission [3].
Quantitative Comparisons and Case Study Data
The flexibility of the V&V 40 framework is best illustrated through concrete examples. The following table compares two hypothetical Contexts of Use for a computational fluid dynamics (CFD) model of a centrifugal blood pump, demonstrating how risk drives credibility requirements [1].
Table 2: Case Study Comparison: Credibility Requirements for a Centrifugal Blood Pump Model
| Credibility Factor | Context of Use 1:\nCPB Pump (Low Risk) | Context of Use 2:\nVAD Pump (High Risk) | Supporting Experimental Data & Rationale |
|---|---|---|---|
| Model Influence | Complementary evidence (Medium) | Primary evidence (High) | For the VAD COU, the model is a primary source of "clinical" information on hemolysis [1]. |
| Decision Consequence | Low impact on patient risk | High impact on patient risk | VAD use is life-sustaining; hemolysis directly impacts patient safety [1]. |
| Output Comparison | Qualitative comparison of flow fields | Quantitative comparison with strict acceptance criteria | For the VAD COU, a quantitative validation metric (e.g., using in vitro hemolysis test data) with tight tolerances is required [1]. |
| Test Samples | Single operating point tested | Multiple operating points across the design space | The high-risk VAD COU requires validation over the entire intended operating range (e.g., 2.5-6 LPM, 2500-3500 RPM) [1]. |
| Uncertainty Quantification | Not required | Required for key output quantities | The prediction of hemolysis for the VAD must include uncertainty bounds to inform safety margins [1]. |
Another case study involving a finite element analysis (FEA) model of a transcatheter aortic valve (TAV) for design verification highlights the framework's application in regulatory contexts. The model was used for structural component stress/strain analysis per ISO5840-1:2021, and its credibility was established specifically for that COU [13].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successfully implementing the V&V 40 framework requires a suite of tools and materials for model development, testing, and validation.
Table 3: Essential Research Reagents and Materials for V&V 40 Compliance
| Tool/Reagent Category | Specific Examples | Function in Credibility Assessment |
|---|---|---|
| Commercial Simulation Software | ANSYS CFX, ANSYS Mechanical [13] [1] | Provides the core computational physics solver for the model. Its built-in verification tools and quality assurance are foundational. |
| Experimental Test Rigs | In vitro hemolysis test loops [1]; Particle Image Velocimetry (PIV) systems [1] | Generate high-quality comparator data for model validation under controlled conditions that mimic the COU. |
| CAD & Meshing Tools | SolidWorks [1]; ANSYS Meshing [1] | Used to create the digital geometry and finite volume/finite element representation of the medical device. |
| Standardized Material Properties | Medical-grade PEEK for device testing [13]; Newtonian blood analog fluids [1] | Provide consistent, well-defined model inputs and ensure test conditions are representative of real-world use. |
| Code Verification Suites | Method of Manufactured Solutions (MMS) benchmarks; grid convergence study tools [7] | Used to verify that the numerical algorithms in the software are solving the mathematical equations correctly. |
| Data Analysis & Statistical Packages | Custom scripts for validation metrics; uncertainty quantification libraries | Enable quantitative output comparison and the calculation of uncertainty intervals for model predictions. |
The ASME V&V 40 standard provides a uniquely flexible and powerful framework for establishing confidence in computational models used for medical devices. Its core differentiator is the risk-informed principle, which ensures that the rigor and cost of credibility activities are proportionate to the model's impact on patient safety and regulatory decisions [1]. While standards from NASA offer robust methodologies for general engineering applications, and systems biology standards solve critical challenges in model reproducibility, V&V 40 is specifically designed and recognized for the medical device regulatory landscape [3] [2]. As the field evolves with emerging applications like In Silico Clinical Trials (ISCT), the principles of V&V 40 continue to be extended and refined, underscoring its role as a foundational element in the credible practice of computational modeling for healthcare [7].
Computational models are increasingly critical for high-impact decision-making across scientific, engineering, and medical domains. Within regulatory science, agencies including the U.S. Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the National Aeronautics and Space Administration (NASA) have established frameworks to ensure the credibility of these computational approaches. These standards are particularly relevant for pharmaceutical development and public health protection, where model predictions can influence therapeutic approval and patient safety. This guide provides a systematic comparison of credibility standards across these three organizations, contextualized within broader research on computational model validation. It is designed to assist researchers, scientists, and drug development professionals in navigating multi-jurisdictional regulatory requirements for in silico evidence submission. The comparative analysis focuses on organizational structures, specific credibility assessment criteria, and practical implementation pathways, supported by standardized experimental data presentation and visualization.
Organizational Structures and Regulatory Authority
The regulatory frameworks governing computational model credibility are fundamentally shaped by the distinct organizational structures and mandates of the FDA, EMA, and NASA.
FDA (U.S. Food and Drug Administration): The FDA operates as a centralized federal authority within the U.S. Department of Health and Human Services. Its Center for Drug Evaluation and Research (CDER) possesses direct decision-making power to approve, reject, or request additional information for new drug applications. This centralized model enables relatively swift decision-making, as review teams consist of FDA employees who facilitate consistent internal communication. Upon FDA approval, a drug is immediately authorized for marketing throughout the entire United States, providing instantaneous nationwide market access [14].
EMA (European Medicines Agency): In contrast, the EMA functions primarily as a coordinating network across European Union Member States rather than a single decision-making body. Based in Amsterdam, it coordinates the scientific evaluation of medicines through its Committee for Medicinal Products for Human Use (CHMP), which leverages experts from national competent authorities. Rapporteurs from these national agencies lead the assessment, and the CHMP issues scientific opinions. The final legal authority to grant marketing authorization, however, rests with the European Commission. This network model incorporates diverse scientific perspectives from across Europe but requires more complex coordination among multiple national agencies, potentially reflecting varied healthcare systems and medical traditions [14].
NASA (National Aeronautics and Space Administration): As a U.S. federal agency, NASA's credibility standards for computational modeling were developed to ensure reliability in high-stakes aerospace applications, including missions that are prohibitively expensive or require unique environments like microgravity. These standards have subsequently influenced regulatory science in other fields, including medicine. NASA's approach is characterized by a rigorous, evidence-based framework for establishing trust in computational models, which has served as a reference for other organizations developing their own credibility assessments [2].
Table 1: Overview of Regulatory Structures and Model Evaluation Contexts
| Organization | Organizational Structure | Primary Context for Model Evaluation | Geographical Scope |
|---|---|---|---|
| FDA | Centralized Federal Authority | Drug/Biologic Safety, Efficacy, and Quality | United States |
| EMA | Coordinating Network of National Agencies | Medicine Safety, Efficacy, and Quality | European Union |
| NASA | Centralized Federal Agency | Aerospace Engineering and Science | Primarily U.S., with international partnerships |
Comparative Analysis of Credibility Standards
While all three organizations share the common goal of ensuring model reliability, their specific approaches to credibility assessment differ in focus, application, and procedural details.
FDA Credibility Standards for Computational Modeling
The FDA defines model credibility as “the trust, established through the collection of evidence, in the predictive capability of a computational model for a context of use (COU)” [2]. The FDA's approach is adaptable, with credibility evidence requirements scaling proportionally with the model's impact on regulatory decisions. For models supporting key safety or efficacy conclusions, the FDA expects comprehensive verification and validation (V&V). Key components of the FDA's framework include:
- Context of Use Definition: A precise specification of the model's purpose and the specific regulatory question it addresses.
- Model Verification: Ensuring the computational model is implemented correctly and operates as intended.
- Model Validation: Assessing the model's accuracy in representing real-world biological or clinical systems, often through comparison with experimental or clinical data.
- Uncertainty Quantification: Characterizing the uncertainty in model inputs, parameters, and outputs to understand their impact on predictions.
The FDA has begun accepting modeling and simulation as forms of evidence for pharmaceutical and medical device approval, particularly when such models are adequately validated and their limitations are understood [2].
EMA Requirements for Model Credibility
The EMA's approach to computational model assessment is integrated within its broader regulatory evaluation process for medicines. Like the FDA, the EMA acknowledges the growing role of modeling and simulation in product development and regulatory submission. A cornerstone of the EMA's framework is the Risk Management Plan (RMP), required for all new marketing authorization applications. The RMP is a dynamic document that includes detailed safety specifications and pharmacovigilance activities, which can encompass the use of predictive models [15] [14]. While the EMA does not have a separate, publicly detailed credibility standard akin to NASA's, its scientific committees evaluate the credibility of submitted models based on principles of scientific rigor, transparency, and relevance to the clinical context. The assessment often emphasizes the clinical meaningfulness of model-based findings beyond mere statistical significance [14].
NASA Credibility Standards and Their Influence
NASA has developed a well-structured and influential framework for credibility assessment, formalized in a set of "Ten Rules" and a corresponding rubric for evaluating conformance [16]. This framework was born from the need to rely on computational models for complex, high-consequence aerospace experiments and engineering tasks. The standard is designed to be qualitative and adaptable to a wide range of models, from engineering simulations to potential biomedical applications. The core principles emphasize:
- Comprehensive Documentation: Ensuring all aspects of model development, assumptions, and implementation are thoroughly documented.
- Robust Verification and Validation: Demonstrating that the model is solved correctly (verification) and that it accurately represents the real-world system (validation).
- Uncertainty and Sensitivity Analysis: Quantifying uncertainties and determining how they affect model outcomes.
- Model Reproducibility: Enabling independent researchers to recreate the model and obtain consistent results, a significant challenge in computational science [2].
This NASA framework provides a foundational structure that has informed credibility discussions in other regulatory and scientific communities, including biomedical research [16] [2].
Table 2: Comparative Analysis of Credibility Framework Components
| Component | FDA | EMA | NASA |
|---|---|---|---|
| Primary Guidance | Context of Use-driven Evidence Collection | Integrated within RMP and Scientific Advice | "Ten Rules" Rubric |
| Core Principle | Evidence-based trust in predictive capability | Scientific rigor and clinical relevance | Comprehensive verification and validation |
| Key Document | Submission-specific evidence package | Risk Management Plan (RMP) | Conformance rubric and documentation |
| Uncertainty Handling | Uncertainty Quantification | Implicit in benefit-risk assessment | Explicit Uncertainty and Sensitivity Analysis |
| Applicability | Pharmaceutical & Medical Device Submissions | Pharmaceutical Submissions | Aerospace, Engineering, with cross-disciplinary influence |
Experimental Protocols for Credibility Assessment
Implementing a robust credibility assessment requires a systematic, multi-stage experimental workflow. The following protocol, aligned with regulatory expectations, outlines the key methodologies for establishing model credibility.
Figure 1: A generalized workflow for assessing computational model credibility, illustrating the sequence from context definition to final evidence assembly for regulatory review.
Protocol 1: Context of Use (COU) Definition
Objective: To establish a clear and unambiguous statement of the computational model's purpose, the specific regulatory question it will inform, and the boundaries of its application. This is the critical first step that determines the scope and extent of all subsequent credibility evidence [2].
Methodology:
- Problem Scoping: Formally define the clinical or biological problem the model addresses. For a drug development context, this could be predicting tumor growth inhibition or characterizing a pharmacokinetic profile.
- Model Interface Specification: Detail the model's inputs (e.g., drug dose, patient biomarkers) and outputs (e.g., survival probability, biomarker change).
- Acceptable Risk Thresholds: In consultation with regulatory guidelines, define the level of uncertainty that is acceptable for the intended decision. A model supporting a primary efficacy endpoint requires a higher evidence standard than one used for exploratory research.
Protocol 2: Model Verification and Validation (V&V)
Objective: To ensure the computational model is implemented correctly (Verification) and that it accurately represents the real-world system of interest (Validation).
Methodology:
- Verification:
- Code Verification: Use techniques like unit testing, consistency checks, and convergence analysis to ensure the software is free of coding errors and the numerical solutions are accurate.
- Model Verification: Confirm that the conceptual model has been correctly translated into computer code, often by comparing outputs to known analytical solutions or results from independent implementations.
- Validation:
- Experimental Design: Identify and procure independent datasets not used in model calibration. These can come from clinical trials, published literature, or experimental studies.
- Goodness-of-fit Testing: Quantitatively compare model predictions against the validation data using appropriate statistical measures (e.g., Mean Squared Error, R-squared, Bayesian metrics).
- Face Validation: Engage domain experts (e.g., clinicians, biologists) to qualitatively assess whether the model behavior and outputs are biologically or clinically plausible.
Protocol 3: Uncertainty and Sensitivity Analysis
Objective: To quantify the uncertainty in model predictions and identify which model inputs and parameters contribute most to this uncertainty.
Methodology:
- Uncertainty Quantification (UQ):
- Characterize uncertainty in model input parameters (e.g., as probability distributions derived from data).
- Propagate these uncertainties through the model using techniques like Monte Carlo sampling to generate a distribution of possible outputs, resulting in prediction intervals (e.g., 95% confidence intervals) rather than single point estimates.
- Sensitivity Analysis (SA):
- Perform global sensitivity analysis (e.g., using Sobol' indices or Morris method) to rank the influence of model inputs and parameters on the output variance.
- This identifies critical parameters that require more precise estimation and simplifies models by fixing non-influential parameters.
Research Reagent Solutions and Essential Materials
Successfully executing credibility assessments requires leveraging a suite of standardized tools, resources, and data formats. The table below details key "research reagents" for computational modeling in a regulatory context.
Table 3: Essential Research Reagents and Resources for Credibility Assessment
| Item Name | Type/Category | Primary Function in Credibility Assessment |
|---|---|---|
| Systems Biology Markup Language (SBML) | Model Encoding Standard | Provides a standardized, machine-readable format for exchanging and reproducing computational models of biological processes [2]. |
| CellML | Model Encoding Standard | An XML-based language for storing and sharing mathematical models, with a strong emphasis on unit consistency and modular component reuse [2]. |
| MIRIAM Guidelines | Annotation Standard | Defines the minimum information required for annotating biochemical models, ensuring model components are unambiguously linked to biological entities, which is crucial for reproducibility [2]. |
| BioModels Database | Model Repository | A curated resource of published, peer-reviewed computational models, providing access to reproducible models for validation and benchmarking [2]. |
| Risk Management Plan (RMP) | Regulatory Document Template (EMA) | The structured template required by EMA for detailing pharmacovigilance activities and risk minimization measures, which may include model-based safety analyses [15] [14]. |
| Common Technical Document (CTD) | Regulatory Submission Format | The internationally agreed-upon format for submitting regulatory applications to both FDA and EMA, organizing the information into five modules [14]. |
| NASA "Ten Rules" Rubric | Credibility Assessment Tool | A conformance checklist and guidance for establishing model credibility, adaptable from aerospace to biomedical applications [16]. |
Signaling Pathways in Regulatory Submissions
The interaction between different credibility standards and the regulatory submission pathway can be conceptualized as an integrated system. The following diagram maps the logical flow from model development through the application of agency-specific standards to a final regulatory outcome.
Figure 2: A signaling pathway illustrating how computational models and data are processed through agency-specific credibility standards (FDA, EMA, and the influential NASA framework) to inform regulatory submissions and final decisions.
The integration of in silico clinical trials into regulatory decision-making represents one of the most significant transformations in medical product development. As regulatory agencies increasingly accept computational evidence, establishing model credibility has become paramount for researchers and developers. The U.S. Food and Drug Administration (FDA) now explicitly states that verified virtual evidence can support regulatory submissions for devices and biologics, fundamentally changing the evidence requirements for market approval [17]. This paradigm shift demands rigorous validation frameworks to ensure that computational models reliably predict real-world clinical outcomes, particularly when these models aim to reduce, refine, or replace traditional human and animal testing [18] [19].
The FDA's 2023 guidance document "Assessing the Credibility of Computational Modeling and Simulation in Medical Device Submissions" provides a risk-informed framework for evaluating computational evidence, signaling a maturation of regulatory standards for in silico methodologies [3]. This guidance, coupled with recent legislative changes such as the FDA Modernization Act 2.0 which removed the mandatory animal testing requirement for drugs, has created both unprecedented opportunities and substantial validation challenges for researchers [20]. Within this evolving landscape, this article examines the concrete standards, experimental protocols, and validation methodologies that underpin credible in silico approaches to regulatory submissions.
Establishing Credibility: Frameworks and Standards
Regulatory Foundations and Validation Frameworks
Regulatory acceptance of in silico evidence hinges on systematic credibility assessment following established frameworks. The ASME V&V 40 standard provides the foundational framework for assessing computational model credibility, offering a risk-informed approach that links validation activities to a model's context of use [17] [21]. This standard has been directly referenced in FDA guidance documents and has seen practical application in developing regulatory-grade models, such as the Bologna Biomechanical Computed Tomography solution for hip fracture risk prediction [21].
The FDA's risk-informed credibility assessment framework evaluates computational modeling and simulation (CM&S) through multiple evidence dimensions [3]. This approach requires researchers to establish a clear context of use (COU) statement that precisely defines the role and scope of the computational model within the regulatory decision-making process. The level of required credibility evidence escalates with the model's risk influence factor – a measure of how substantially the computational results will impact regulatory determinations of safety and effectiveness.
Table 1: Key Regulatory Developments Enabling In Silico Submissions
| Date | Agency | Policy/Milestone | Impact on In Silico Methods |
|---|---|---|---|
| December 2022 | U.S. Congress | FDA Modernization Act 2.0 | Removed statutory animal-test mandate; recognized in silico models as valid nonclinical tests [20] |
| November 2023 | FDA | CM&S Credibility Assessment Guidance | Formalized risk-informed framework for evaluating computational evidence in medical device submissions [3] |
| April 2025 | FDA | Animal Testing Phase-Out Roadmap | Announced plan to reduce/Replace routine animal testing, prioritizing MPS data and AI-driven models [18] [20] |
| September 2024 | FDA | First Organ-Chip in ISTAND Program | Accepted Liver-Chip S1 for predicting drug-induced liver injury, setting procedural precedent [20] |
Credibility Evidence Requirements and Documentation
Building a persuasive credibility dossier requires multifaceted evidence across technical and biological domains. The FDA's framework emphasizes three interconnected evidence categories: computational verification (ensuring models are solved correctly), experimental validation (confirming models accurately represent reality), and uncertainty quantification (characterizing variability and error) [3]. For high-impact regulatory submissions, developers must provide comprehensive documentation spanning model assumptions, mathematical foundations, input parameters, and validation protocols.
Technical credibility requires demonstration of numerical verification through mesh convergence studies, time step independence analyses, and solver accuracy assessments. Meanwhile, physical validation demands comparison against high-quality experimental data, with increasing rigor required for higher-stakes applications. The emerging best practice involves creating a validation hierarchy where model components are validated against simpler systems before progressing to full organ-level or organism-level validation [3].
In Silico Trials in Regulatory Submissions: Applications and Outcomes
Therapeutic Area Implementation and Impact
In silico methodologies have demonstrated particularly strong value in therapeutic areas where traditional trials face ethical, practical, or financial constraints. Oncology represents the largest application segment, capturing 25.78% of the in silico clinical trials market in 2024, with projections reaching $1.6 billion by 2030 [17]. The complexity of multi-drug regimens and significant tumor genetic heterogeneity in oncology benefit tremendously from in silico dose optimization and the creation of large synthetic cohorts to achieve statistical power.
Neurology has emerged as the fastest-growing discipline with a 15.46% CAGR, driven by advanced applications such as Stanford's visual-cortex digital twin that enables unlimited virtual experimentation [17]. The repeated failures of Alzheimer's candidates in late-stage traditional trials have highlighted the limitations of conventional models and created urgency for more predictive computational approaches that can simulate long-term disease progression and stratify patients by digital biomarkers [19].
Table 2: In Silico Clinical Trial Applications Across Development Phases
| Development Phase | Primary Applications | Reported Impact | Example Cases |
|---|---|---|---|
| Preclinical | PBPK models, toxicity screening, animal study reduction | Flags risky compounds early; reduces animal use [22] | Roche's AI surrogate model for T-DM1 dose selection [22] |
| Phase I | First-in-human dose prediction, virtual cohort generation | Rising fastest at 13.78% CAGR; could surpass $510M by 2030 [17] | AI-designed compounds with pre-computed toxicity profiles [17] |
| Phase II | Dose optimization, synthetic control arms, efficacy assessment | Constituted 34.85% of deployments in 2024 [17] | AstraZeneca's QSP model for PCSK9 therapy (6-month acceleration) [22] |
| Phase III/Registrational | Trial design optimization, digital twin control arms | Synthetic control arms reduce enrollment by 20% [17] | Pfizer's PK/PD simulations for tofacitinib (replaced Phase 3 trials) [22] |
| Post-Approval | Long-term safety extrapolation, label expansion simulations | Enhanced surveillance with real-world data feeds [17] [22] | BMS-PathAI partnership for PD-L1 scoring in tumor slides [22] |
Regulatory Precedents and Successful Submissions
Several landmark regulatory submissions have demonstrated the viability of in silico evidence as a primary component of regulatory packages. Pfizer secured FDA acceptance for in silico PK/PD simulation data bridging efficacy between immediate- and extended-release tofacitinib for ulcerative colitis, eliminating the need for new phase 3 trials [22] [23]. This precedent confirms that properly validated computational models can substantially reduce traditional clinical trial requirements for approved molecules seeking formulation changes.
In the medical device sector, the FDA approved the restor3d Total Talus Replacement based primarily on computational design from patient CT data, demonstrating that in silico engineering approaches can meet safety thresholds for implantable devices [17]. Similarly, Medtronic utilized computational fluid dynamics (CFD) virtual trials to predict aneurysm flow reduction for its Pipeline Embolization Device, with results correlating well with subsequent clinical trial outcomes [23].
The expanding regulatory acceptance is reflected in market data: the in-silico clinical trials market size reached $3.95 billion in 2024 and is projected to grow to $6.39 billion by 2033, demonstrating increasing integration into mainstream development pathways [24].
Experimental Protocols for Model Validation
Core Validation Methodologies
Establishing model credibility requires rigorous experimental protocols that systematically evaluate predictive performance against relevant clinical data. The following standardized protocol outlines key validation steps:
Protocol 1: Comprehensive Model Validation
- Context of Use Definition: Precisely specify the model's regulatory application, including specific clinical endpoints and patient populations.
- Validation Hierarchy Establishment: Define a cascade of validation benchmarks from simple systems (cellular, tissue) to complex organ-level or population-level responses.
- Reference Data Collection: Curate high-quality clinical or experimental data for comparison, documenting sources, demographics, and measurement uncertainties.
- Model Prediction: Generate computational results for validation cases without reference to outcome data (prospective prediction preferred).
- Comparison Metrics Application: Calculate quantitative agreement metrics including mean absolute error, correlation coefficients, and confidence intervals.
- Uncertainty Quantification: Characterize uncertainty from input parameters, numerical approximations, and biological variability.
- Sensitivity Analysis: Identify influential parameters and assumptions through local (one-at-a-time) or global (variance-based) methods.
- Documentation and Reporting: Compile comprehensive validation report including all inputs, methods, results, and limitations.
This structured approach aligns with the ASME V&V 40 framework and FDA guidance recommendations, emphasizing transparency and methodological rigor [21] [3].
Technical Workflow for In Silico Trial Implementation
The implementation of regulatory-grade in silico trials requires integration of multiple computational and data modules into a cohesive workflow. The leading framework comprises six tightly integrated components that simulate different aspects of clinical trials [22]:
Figure 1: In Silico Trial Workflow illustrating the six modular components and their interactions, with feedback loops enabling iterative refinement.
This workflow creates an iterative system where outputs from later stages can refine earlier modules. For instance, operational simulations might reveal that certain protocol designs are impractical to implement, triggering protocol redesign before resimulation [22]. This iterative refinement capability represents a significant advantage over traditional static trial designs.
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Implementing credible in silico trials requires specialized computational tools and platforms validated for regulatory applications. The following table details essential solutions across key functional categories:
Table 3: Essential Research Reagent Solutions for In Silico Trials
| Tool Category | Representative Platforms | Primary Function | Regulatory Validation Status |
|---|---|---|---|
| PK/PD Modeling | Certara Phoenix, Simulations Plus | Predicts drug concentration and effect relationships; supports dose selection | Used in 75+ top pharma companies; accepted by 11 regulatory agencies [24] |
| Medical Device Simulation | ANSYS, Dassault Systèmes | Physics-based modeling of device performance and tissue interactions | FDA acceptance for implantable devices (e.g., restor3d Talus Replacement) [17] |
| Virtual Patient Generation | Insilico Medicine, InSilicoTrials | Creates synthetic patient cohorts with realistic characteristics and variability | Deployed in Phase I supplement studies; synthetic control arms [17] [23] |
| Trial Operational Simulation | The AnyLogic Company, Nova | Models recruitment, site activation, and other operational factors | Integrated into protocol optimization workflows at major CROs [22] [24] |
| QSP Platforms | Physiomics Plc, VeriSIM Life | Mechanistic modeling of drug effects across biological pathways | Used in AstraZeneca's PCSK9 accelerator program (6-month time saving) [22] [23] |
Beyond commercial platforms, successful in silico trial implementation requires robust data management infrastructures that adhere to FAIR principles (Findable, Accessible, Interoperable, Reusable). The integration of real-world data from electronic health records, wearable sensors, and patient registries provides essential training and validation datasets for refining computational models [22]. Emerging best practices also emphasize the importance of version control systems for computational models and comprehensive documentation pipelines that track all model modifications and assumptions throughout the development process.
Signaling Pathways: The Credibility Assessment Framework
The credibility assessment process for regulatory submissions follows a systematic pathway that evaluates multiple evidence dimensions. The following diagram illustrates the key decision points and validation requirements:
Figure 2: Credibility Assessment Framework depicting the systematic pathway from context definition to regulatory decision, emphasizing evidence requirements.
This assessment pathway begins with precise Context of Use (COU) specification, which determines the model's purpose and regulatory impact. The Risk Influence Factor assessment then establishes the required evidence level, with higher-risk applications demanding more extensive validation [3]. Evidence gathering encompasses three interconnected domains: Verification and Validation (V&V) confirms numerical accuracy and predictive capability; Uncertainty Quantification characterizes variability and error; and Sensitivity Analysis identifies influential parameters and assumptions. The cumulative evidence supports the final regulatory determination of model credibility for the specified context.
The integration of in silico methodologies into regulatory submissions represents a fundamental transformation in medical product development. As regulatory agencies increasingly accept computational evidence, establishing model credibility through rigorous validation frameworks has become essential. The convergence of regulatory modernization, computational advancement, and growing clinical validation has created an inflection point where in silico trials are transitioning from supplemental to central components of development pipelines.
The successful examples from industry leaders demonstrate that properly validated computational models can accelerate development timelines by 25% or more while reducing costs and ethical burdens [25]. However, realizing this potential requires meticulous attention to credibility frameworks, comprehensive validation protocols, and transparent documentation. The institutions that master these competencies will lead the next era of medical product development, where simulation informs every stage from discovery through post-market surveillance.
For researchers and developers, the imperative is clear: invest in robust validation methodologies, maintain rigorous documentation practices, and actively engage with evolving regulatory expectations. As one editorial starkly concluded, "In a decade, failing to run in silico trials may not just be seen as a missed opportunity. It may be malpractice" [19]. The standards for computational credibility are being written today through pioneering submissions that establish precedents for the entire field.
From Theory to Practice: Implementing Verification, Validation, and Uncertainty Quantification
The ASME V&V 40-2018 standard provides a risk-informed framework for establishing credibility requirements for computational models used in medical device evaluation and other high-consequence fields [7] [4]. This standard has become a key enabler for regulatory submissions, forming the basis of the U.S. Food and Drug Administration (FDA) CDRH framework for evaluating computational modeling and simulation data in medical device submissions [7] [3]. The core innovation of V&V 40 lies in its risk-based approach to verification and validation (V&V), which tailors the rigor and extent of credibility activities to the model's specific context of use and the decision-related risks involved [7].
The standard introduces credibility factors as essential attributes that determine a model's trustworthiness for its intended purpose. These factors guide the planning and execution of V&V activities, ensuring that computational models provide sufficient evidence to support high-stakes decisions in medical device development, regulatory evaluation, and increasingly in in-silico clinical trials (ISCTs) [7] [26]. The framework acknowledges that different modeling contexts require different levels of evidence, and it provides a structured methodology for determining the appropriate level of V&V activities based on the model's role in decision-making and the potential consequences of an incorrect result [3].
Core Components of the Credibility Factor Framework
Foundational Principles and Risk-Based Approach
The Credibility Factor Framework operates on several foundational principles that distinguish it from traditional V&V approaches. First, it explicitly recognizes that not all models require the same level of validation – the necessary credibility evidence is directly proportional to the model's decision consequence, meaning the impact that an incorrect model result would have on the overall decision [7]. Second, the framework emphasizes a systematic planning process that begins with clearly defining the context of use, which includes the specific question the model will answer, the relevant physical quantities of interest, and the required accuracy [3].
The risk-based approach incorporates two key dimensions: decision consequence and model influence. Decision consequence categorizes the potential impact of an incorrect model result (low, medium, or high), while model influence assesses how much the model output contributes to the overall decision (supplemental, influential, or decisive). These dimensions collectively determine the required credibility level for each credibility factor [7] [3]. This nuanced approach represents a significant advancement over one-size-fits-all validation requirements, enabling more efficient allocation of V&V resources while maintaining scientific rigor where it matters most.
Key Credibility Factors and Corresponding V&V Activities
The framework identifies specific credibility factors that must be addressed to establish model trustworthiness. For each factor, the standard outlines a continuum of potential V&V activities ranging from basic to comprehensive, with the appropriate level determined by the risk assessment [7]. The following table summarizes the core credibility factors and their corresponding V&V activities:
Table: Core Credibility Factors and Corresponding V&V Activities in ASME V&V 40
| Credibility Factor | Description | Example V&V Activities |
|---|---|---|
| Verification | Ensuring the computational model is implemented correctly and without error [7]. | Code verification, calculation verification, systematic mesh refinement [7]. |
| Validation | Determining how accurately the computational model represents the real-world system [7]. | Comparison with experimental data, historical data as comparator, validation experiments [7] [21]. |
| Uncertainty Quantification | Characterizing and quantifying uncertainties in model inputs, parameters, and predictions [27]. | Sensitivity analysis, statistical uncertainty propagation, confidence interval estimation [27]. |
| Model Form | Assessing the appropriateness of the underlying mathematical models and assumptions [7]. | Comparison with alternative model forms, evaluation of simplifying assumptions [7]. |
| Input Data | Evaluating the quality and appropriateness of data used to define model inputs and parameters [7]. | Data provenance assessment, parameter sensitivity analysis, input uncertainty characterization [7]. |
Experimental Protocols for Credibility Assessment
Verification Protocols: Code and Calculation Verification
Verification constitutes the foundational layer of credibility assessment, ensuring that the computational model is implemented correctly and solved accurately. The protocol begins with code verification, which confirms that the mathematical algorithms are implemented without programming errors. This typically involves comparing computational results against analytical solutions for simplified cases where exact solutions are known [7].
Calculation verification follows, focusing on quantifying numerical errors in specific solutions. As highlighted in recent applications, systematic mesh refinement plays a critical role in this process [7]. The experimental protocol involves:
- Generating a series of computational meshes with progressively refined element sizes
- Solving the boundary value problem on each mesh
- Quantifying solution metrics of interest for each mesh refinement level
- Analyzing the convergence behavior of these metrics as mesh size decreases
- Extrapolating to estimate the discretization error at zero mesh size
Research demonstrates that failing to apply systematic mesh refinement can produce misleading results, particularly for complex simulations like blood hemolysis modeling [7]. For unstructured meshes with nonuniform element sizes, maintaining systematic refinement requires special attention to often-overlooked aspects such as consistent element quality metrics across refinement levels [7].
Validation Protocols: Comparative Analysis and Uncertainty Quantification
Validation protocols determine how accurately a computational model represents real-world physics. The standard approach involves hierarchical testing, beginning with component-level validation and progressing to system-level validation as needed based on the risk assessment [7] [3]. The validation protocol comprises:
- Designing validation experiments that isolate specific physical phenomena relevant to the context of use
- Quantifying experimental uncertainty through repeated measurements and statistical analysis
- Comparing computational results with experimental data using predefined validation metrics
- Assessing agreement through both quantitative measures and qualitative engineering judgment
For patient-specific models, such as those used in femur fracture prediction, validation presents unique challenges. The ASME VVUQ 40 sub-committee is developing a classification framework for comparators that assesses the credibility of patient-specific computational models [7]. This framework defines, classifies, and compares different types of comparators (e.g., direct experimental measurements, clinical imaging, historical data), highlighting the strengths and weaknesses of each comparator type, and providing rationale for selection [7].
A key advancement in validation methodology is the formal uncertainty quantification process, which characterizes both computational and experimental uncertainties and propagates them through the model to determine whether differences between simulation and experiment are statistically significant [27]. This represents a shift from binary pass/fail validation to a probabilistic assessment of agreement.
Workflow Visualization: Credibility Factor Assessment Process
The following diagram illustrates the systematic workflow for planning V&V activities using the Credibility Factor Framework:
Diagram: Credibility Factor Assessment Workflow. This workflow illustrates the iterative process of establishing model credibility according to ASME V&V 40.
Comparative Analysis of V&V Implementation Scenarios
The application of the Credibility Factor Framework varies significantly based on the modeling context and application domain. The following table compares implementation approaches across different scenarios, highlighting how V&V activities are tailored to specific contexts:
Table: Comparative Analysis of V&V Implementation Across Application Domains
| Application Domain | Context of Use | Key Credibility Factors | Implementation Approach |
|---|---|---|---|
| Traditional Medical Devices | Evaluation of tibial tray durability [7] | Model verification, validation, uncertainty quantification | Comprehensive verification via mesh refinement; physical testing validation; moderate UQ |
| In-Silico Clinical Trials | Synthetic patient cohorts for trial simulation [26] | Model form validity, predictive capability, uncertainty quantification | High-fidelity validation against historical data; extensive UQ for population variability |
| Patient-Specific Modeling | Femur fracture prediction [7] [21] | Input data credibility, validation with clinical data | Classification framework for comparators; imaging data validation; specialized UQ |
| Digital Twins in Manufacturing | Real-time decision support [27] | Ongoing verification, continuous validation, UQ | Lifecycle V&V approach; real-time validation with sensor data; dynamic UQ |
The comparative analysis reveals that while the fundamental credibility factors remain consistent, their implementation varies based on the model's context of use. For traditional medical devices, the focus remains on rigorous verification and physical validation [7]. In contrast, in-silico clinical trials emphasize predictive capability and comprehensive uncertainty quantification due to their role in augmenting or replacing human clinical trials [26]. Patient-specific models require specialized approaches to validation, often relying on medical imaging data as comparators rather than traditional physical experiments [7]. For digital twins in manufacturing, the credibility assessment extends throughout the entire lifecycle, requiring continuous rather than one-time V&V activities [27].
Successful implementation of the Credibility Factor Framework requires both methodological expertise and practical tools. The following table details essential resources for researchers planning V&V activities:
Table: Research Reagent Solutions for Credibility Assessment
| Tool/Resource | Function | Application Context |
|---|---|---|
| ASME VVUQ 40.1 Technical Report | Provides detailed example applying V&V 40 to a tibial tray durability model [7] | Medical device evaluation; educational resource |
| Systematic Mesh Refinement Tools | Enables code and calculation verification through controlled mesh refinement studies [7] | Finite element analysis; computational fluid dynamics |
| Comparator Classification Framework | Guides selection of appropriate comparators for model validation, especially for patient-specific models [7] | Patient-specific modeling; clinical applications |
| Uncertainty Quantification Software | Characterizes and propagates uncertainties through computational models [27] | Risk assessment; predictive modeling |
| FDA Credibility Assessment Guidance | Provides regulatory perspective on implementing credibility factors for medical devices [3] | Regulatory submissions; medical device development |
Future Directions and Emerging Applications
The Credibility Factor Framework continues to evolve through standardization efforts and emerging applications. The ASME VVUQ 40 sub-committee is actively working on several extensions, including technical reports focused on patient-specific modeling and specialized applications [7]. These efforts aim to address unique challenges in personalized medicine and clinical decision support, where traditional V&V approaches may require adaptation [7] [21].
A significant emerging application is in the realm of in-silico clinical trials, where the credibility demands are particularly high due to the potential for these simulations to augment or replace traditional human trials [26]. As noted by regulatory science experts, "For a simulation to be used in such a high consequence application, the credibility of the model must be well-established in the eyes of the diverse set of stakeholders who are impacted by the trial's outcome" [7]. This application domain presents unique validation challenges, particularly when direct validation against human data is limited for practical or ethical reasons [7].
The integration of artificial intelligence and machine learning with traditional physics-based modeling represents another frontier for the Credibility Factor Framework [26]. These hybrid approaches introduce new credibility considerations, such as the need for explainable AI and validation of data-driven model components [26]. Ongoing standardization efforts aim to extend the framework to address these technological advancements while maintaining the rigorous risk-based approach that has made ASME V&V 40 successful in regulatory applications [7] [26].
Verification is a foundational process in computational modeling that ensures a mathematical model is implemented correctly and solves the equations accurately. Within the broader framework of model credibility, which also includes validation (assessing model accuracy against real-world data), verification specifically addresses "solving the equations right" [28]. For researchers and drug development professionals using finite element analysis (FEA), systematic mesh refinement serves as a critical verification technique to quantify numerical accuracy and build confidence in simulation results intended for regulatory submissions.
The credibility of computational modeling and simulation (CM&S) has gained significant attention from regulatory bodies like the FDA, which has issued guidance on assessing credibility for medical device submissions [3]. This guidance emphasizes a risk-informed framework where verification activities should be commensurate with a model's context of use—the role and impact the simulation has in a regulatory decision. For high-impact decisions, such as using simulations to replace certain clinical trials, rigorous verification through methods like systematic mesh refinement becomes essential.
Theoretical Foundation of Systematic Mesh Refinement
Discretization Error and Mesh Convergence
The finite element method approximates solutions to partial differential equations by dividing the computational domain into smaller subdomains (elements) connected at nodes. This discretization inevitably introduces numerical error, which systematically reduces as the mesh is refined [29]. The process of mesh refinement involves successively increasing mesh density and comparing results between these different meshes to evaluate convergence—the point at which further refinement no longer significantly improves results [30].
Mesh convergence studies form the cornerstone of calculation verification, providing evidence that discretization errors have been reduced to an acceptable level for the intended context of use. The core principle is that as element sizes decrease uniformly throughout the model, the computed solution should approach the true mathematical solution of the governing equations. Different solution metrics (displacements, stresses, strains) converge at different rates, with integral quantities like strain energy typically converging faster than local gradient quantities like stresses [29].
Mathematical Basis of Error Estimation
In practical FEA applications, the exact mathematical solution remains unknown. Engineers instead estimate discretization error by comparing solutions from systematically refined meshes. A common approach calculates the fractional change (ε) in a quantity of interest between successive mesh refinements:
[ \varepsilon = \frac{|wC - wF|}{w_F} \times 100 ]
Where (wC) and (wF) represent the outputs from coarse and fine mesh levels, respectively [31]. For medical device simulations, a fractional change of 5.0% or less between peak strain predictions is frequently used as an acceptance criterion for mesh suitability [31].
More sophisticated error estimation techniques have emerged, particularly goal-oriented error estimation that focuses on specific output quantities of interest (QoIs) rather than overall solution accuracy. This approach is especially valuable for nonlinear problems where traditional error estimation may underpredict errors in critical outputs [32].
Mesh Refinement Techniques and Methodologies
Approaches to Mesh Refinement
Table 1: Comparison of Mesh Refinement Techniques
| Technique | Mechanism | Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| Uniform Element Size Reduction | Reducing element size throughout model | Simple to implement; systematic | Computationally inefficient; no preferential refinement | Initial convergence studies; simple geometries |
| Element Order Increase | Increasing polynomial order of shape functions | No remeshing required | Computational requirements increase rapidly | When mesh cannot be altered; smooth solutions |
| Global Adaptive Refinement | Error estimation guides automatic refinement throughout domain | Automated; comprehensive error reduction | Possible excessive refinement in non-critical areas | General-purpose analysis; unknown solution characteristics |
| Local Adaptive Refinement | Error estimation focused on specific regions or outputs | Computational efficiency; targeted accuracy | Requires defined local metrics | Stress concentrations; known critical regions |
| Manual Mesh Adjustment | Analyst-controlled mesh sizing based on physics intuition | Potentially most efficient approach | Requires significant expertise and time | Well-understood problems; repetitive analyses |
Systematic mesh refinement encompasses multiple technical approaches, each with distinct advantages and limitations. Reducing element size uniformly throughout the model represents the most straightforward approach but suffers from computational inefficiency as it refines areas where high accuracy may be unnecessary [29]. Increasing element order (e.g., from linear to quadratic elements) utilizes the same mesh topology but with higher-order polynomial shape functions, potentially providing faster convergence for certain problem types [29].
Adaptive mesh refinement techniques automatically refine the mesh based on error indicators. Global adaptive refinement considers error throughout the entire domain, while local adaptive refinement focuses on specific regions or outputs of interest [29]. For specialized applications like phase-field modeling of brittle fracture, researchers have developed automated frameworks utilizing posteriori error indicators to refine meshes along anticipated crack paths without prior knowledge of crack propagation [33].
Workflow for Systematic Mesh Refinement
Systematic Mesh Refinement Workflow
The methodology for conducting systematic mesh refinement follows a structured process beginning with clearly defined analysis objectives and quantities of interest (QoIs). Engineers should start with a coarse mesh that provides a rough solution while verifying applied loads and constraints [29]. After the initial solution, systematic refinement proceeds through multiple mesh levels while tracking changes in QoIs.
The convergence assessment phase evaluates whether additional refinement would yield meaningful improvements. For stent frame analyses, this often involves estimating the exact solution with a 95% confidence interval using submodeling and multiple refined meshes [31]. Finally, the entire process—including mesh statistics, convergence data, and final error estimates—must be thoroughly documented, particularly for regulatory submissions where demonstrating mesh independence may be required [3] [31].
Experimental Protocols for Mesh Refinement Studies
Quantitative Assessment Methods
Table 2: Mesh Convergence Criteria Across Industries
| Industry/Application | Convergence Metric | Typical Acceptance Criterion | Regulatory Reference |
|---|---|---|---|
| Medical Devices (Stent Frames) | Peak strain fractional change | ≤5.0% between successive refinements | ASTM F2996, F3334 [31] |
| Computational Biomechanics | Global energy norm | ≤2-5% error estimate | ASME V&V 40 [28] |
| Drug Development (PBPK Models) | Predictive error | Context-dependent, risk-informed | FDA PBPK Guidance [34] |
| General FEA | Multiple QoIs (displacement, stress, energy) | Asymptotic behavior observed | ASME V&V 20 [28] |
Robust mesh refinement studies employ specific quantitative protocols to assess convergence. The fractional change method, widely used in medical device simulations, calculates the percentage difference in QoIs between successive mesh refinements [31]. For stent frames, a fractional change of 5.0% or less in peak strain predictions often serves as the acceptance criterion, though this threshold should be risk-informed rather than arbitrary [31].
More advanced approaches use Richardson extrapolation to estimate the discretization error by extrapolating from multiple mesh levels to estimate the "zero-mesh-size" solution [31]. For nonlinear problems, recent research introduces two-level adjoint-based error estimation that accounts for linearization errors typically neglected in conventional methods [32]. This approach solves problems on both coarse and fine meshes, then compares results to derive improved error estimates that better reflect true discrepancies in outputs.
Case Study: Cardiovascular Stent Analysis
A detailed methodology for mesh refinement in cardiovascular stent analysis demonstrates application-specific considerations. The process begins with creating a geometric representation of the stent frame, often simplifying microscopic features irrelevant to structural performance [31]. A base mesh is generated using hexahedral elements, with particular attention to regions of anticipated high stress gradients.
The analysis proceeds through multiple mesh levels, typically with refinement ratios of 1.5-2.0 between levels [31]. At each level, the model is solved under relevant loading conditions, and maximum principal strains and stresses are recorded. The study should specifically examine strains at integration points of 3D elements rather than extrapolated values, as the former more accurately represent the discretization error [31].
The final mesh selection balances discretization error, computational cost, and model risk—the potential impact of an incorrect decision on patient safety or business outcomes [31]. This risk-informed approach aligns with FDA guidance that emphasizes considering a model's context of use when determining appropriate verification activities [3].
Standards and Regulatory Framework
Credibility Assessment Framework
Regulatory bodies have established frameworks for assessing computational model credibility. The FDA guidance "Assessing the Credibility of Computational Modeling and Simulation in Medical Device Submissions" provides a risk-informed approach where verification activities should be proportionate to a model's context of use [3]. Similarly, the ASME V&V 40 standard addresses model risk by considering both the influence of simulation results on decisions and the consequences of incorrect decisions [31].
These standards emphasize that verification and validation (V&V) processes must generate evidence establishing that a computer model yields results with sufficient accuracy for its intended use [28]. Within this framework, systematic mesh refinement serves as a fundamental verification activity, providing evidence that numerical errors have been adequately controlled.
Application Across Industries
The pharmaceutical industry faces particular challenges in establishing standards for in silico models used in drug development. While specific guidance exists for traditional pharmacometric models (e.g., population PK, PBPK), emerging mechanistic models like quantitative systems pharmacology (QSP) require adaptation of existing verification frameworks [34]. The complexity of these biological models, which often incorporate multiphysics simulations, creates an unmet need for specific guidance on verification and validation [34].
Across all industries, the fundamental verification principle remains consistent: computational models must be shown to accurately represent their mathematical foundation and numerical implementation. Systematic mesh refinement provides a methodology to address the latter requirement, particularly for finite element and computational fluid dynamics applications.
Research Reagent Solutions: Essential Tools for Verification Studies
Table 3: Essential Research Reagents for Mesh Refinement Studies
| Tool Category | Specific Examples | Function in Verification | Implementation Considerations |
|---|---|---|---|
| FEA Software Platforms | Ansys Mechanical, Abaqus, COMSOL | Provides meshing capabilities and solvers for refinement studies | Varies in adaptive meshing automation and element formulations |
| Mesh Generation Tools | Native FEA meshers, Standalone meshing utilities | Creates initial and refined mesh sequences | Capabilities for batch processing and mesh quality metrics |
| Error Estimation Modules | Native error estimators, Custom algorithms | Quantifies discretization error and guides adaptation | Varies in goal-oriented vs. global error estimation |
| Programming Interfaces | Python, MATLAB, APDL | Automates refinement workflows and data extraction | Enables custom convergence criteria and reporting |
| Regulatory Guidance Documents | FDA CM&S Guidance, ASME V&V 40 | Provides framework for credibility assessment | Risk-informed approach to verification rigor |
The experimental toolkit for systematic mesh refinement studies includes both computational and methodological resources. Software platforms like Ansys Mechanical 2025 R1 offer built-in adaptive meshing capabilities that automatically refine meshes in regions of high gradient, such as around holes, notches, or sharp corners where stress concentrations occur [30]. Similarly, Abaqus provides native error estimation and mesh refinement capabilities that can be tailored for specific applications like phase-field fracture modeling through Python scripting [33].
Programming interfaces enable automation of the mesh refinement process, which is particularly valuable for complex 3D models where manual remeshing would be prohibitively time-consuming. For example, researchers have developed Python-based frameworks that integrate pre-analysis, mesh refinement, and subsequent numerical analysis in a single streamlined process [33]. Such automation ensures consistency across mesh levels and facilitates comprehensive documentation of the refinement study.
Regulatory guidance documents, particularly the FDA framework for assessing computational model credibility, serve as essential methodological resources that shape verification protocols [3]. These documents provide the conceptual framework for risk-informed approaches to mesh refinement, helping researchers determine the appropriate level of verification rigor based on a model's context of use.
Systematic mesh refinement represents a cornerstone practice in verification for computational modeling, providing a methodology to quantify and control discretization errors in finite element analyses. As regulatory agencies increasingly accept computational evidence in submissions for medical products, robust verification practices become essential for establishing model credibility.
The field continues to evolve with advanced techniques like goal-oriented error estimation that specifically target quantities of interest, particularly for nonlinear problems [32]. Future developments will likely focus on increasing automation while maintaining rigorous documentation standards required for regulatory review. For researchers and drug development professionals, implementing systematic mesh refinement protocols with risk-informed convergence criteria provides a pathway to generate trustworthy simulation results that can support critical decisions in product development and regulatory submissions.
In computational biology and medical device development, the scientific credibility of a model is not established by the model itself but through rigorous comparison against empirical, experimental data. These benchmarks, known as experimental comparators, serve as the objective ground truth against which model predictions are measured. The process is a cornerstone of the Verification and Validation (V&V) framework, which is essential for regulatory acceptance and high-impact decision-making. Regulatory bodies like the U.S. Food and Drug Administration (FDA) define model credibility as "the trust, established through the collection of evidence, in the predictive capability of a computational model for a context of use (COU)" [2]. This article explores the strategic definition and use of experimental comparators, framed within the ASME V&V 40 risk-informed credibility standard, which contends that the level of validation evidence should be commensurate with the risk of using the model to inform a decision [1].
Foundational Frameworks for Credibility Assessment
The ASME V&V 40 Risk-Informed Framework
The ASME V&V 40 standard provides a structured framework for establishing model credibility, centralizing the Context of Use (COU) and model risk. The COU is a detailed statement defining the specific role and scope of the computational model in addressing a question of interest. Model risk is the possibility that the model's use leads to a decision resulting in patient harm; it is a combination of the model's influence on the decision and the consequence of an incorrect decision [1]. The framework establishes credibility goals for various V&V activities, which are directly driven by this risk analysis. Consequently, the selection of experimental comparators and the required level of agreement between model predictions and experimental data are dictated by the model's COU and associated risk.
The FDA's Threshold-Based Validation Approach
The FDA has developed a "threshold-based" validation method as a Regulatory Science Tool (RST). This approach provides a means to determine a well-defined acceptance criterion for the comparison error—the difference between simulation results and validation experiments. It is specifically applicable when threshold values for the safety or performance of the quantity of interest are available. The inputs to this RST are the mean values and uncertainties from both the validation experiments and the model predictions, as well as the safety thresholds. The output is a measure of confidence that the model is sufficiently validated from a safety perspective [35]. This method directly links the choice of experimental comparator and the acceptable level of discrepancy to clinically or biologically relevant safety limits.
The following diagram illustrates the logical workflow of a risk-informed credibility assessment, from defining the model's purpose to determining the required level of validation evidence.
Designing a Benchmarking Study for Comparator Selection
A high-quality benchmarking study is essential for the objective comparison of computational methods. The following guidelines, synthesized from best practices in computational biology, ensure that comparators provide accurate, unbiased, and informative results [36].
Essential Guidelines for Benchmarking
- Defining Purpose and Scope: Clearly state the benchmark's purpose at the outset. A neutral benchmark (independent of method development) should be as comprehensive as possible, while a benchmark for a new method may focus on a representative subset of state-of-the-art and baseline methods. The scope dictates the comprehensiveness of method selection.
- Selection of Methods: For a neutral benchmark, strive to include all available methods for a given type of analysis, defining clear, unbiased inclusion criteria (e.g., software availability, installability). When introducing a new method, compare it against current best-performing and widely used methods, ensuring all are evaluated under fair conditions (e.g., avoiding extensive parameter tuning for the new method only).
- Selection of Datasets: The choice of reference datasets is critical. A variety of datasets, including both simulated data (with known ground truth) and real experimental data, should be used to evaluate methods under a wide range of conditions. Simulated data must be shown to accurately reflect the relevant properties of real data.
Table 1: Key Principles for Rigorous Benchmarking
| Principle | Description | Key Consideration |
|---|---|---|
| Purpose & Scope | Define the goal and breadth of the comparison. | A scope too broad is unmanageable; a scope too narrow yields misleading results. |
| Method Selection | Choose which computational methods to include. | Avoid excluding key methods; ensure the selection is representative and unbiased. |
| Dataset Selection | Choose or design reference datasets for testing. | Avoid unrepresentative datasets; use a mix of simulated and real data. |
| Evaluation Metrics | Select quantitative performance metrics. | Choose metrics that translate to real-world performance; no single metric gives a complete picture. |
A Scientist's Toolkit: Key Reagents for Validation
The following table details essential materials and their functions in establishing model credibility through experimental comparison [1] [2].
Table 2: Essential Research Reagent Solutions for Model Validation
| Category | Specific Example | Function in Validation |
|---|---|---|
| In Vitro Test Systems | FDA Generic Centrifugal Blood Pump | Provides a standardized, benchtop hydraulic platform for comparing computational fluid dynamics (CFD) predictions of hemolysis. |
| Experimental Measurement Tools | Particle Image Velocimetry (PIV) | Provides high-fidelity, quantitative velocity field measurements inside devices like blood pumps for direct comparison with CFD results. |
| Biochemical Assays | In Vitro Hemolysis Testing | Measures free hemoglobin release to quantify blood damage, serving as a critical biological comparator for CFD-based hemolysis models. |
| Data & Model Standards | Systems Biology Markup Language (SBML) | A standardized, machine-readable format for encoding models, essential for model reproducibility, exchange, and comparative evaluation. |
| Ontologies & Annotation | MIRIAM Guidelines | Provide minimum information standards for annotating biochemical models, ensuring model components are unambiguously linked to biological realities. |
Experimental Protocols and Case Studies
Case Study: CFD Validation for a Centrifugal Blood Pump
This hypothetical example, based on the ASME V&V 40 framework, demonstrates how the COU dictates the validation strategy for a computational model of a centrifugal blood pump [1].
- Question of Interest: "Are the flow-induced hemolysis levels of the centrifugal pump acceptable for its intended use?"
- Computational Model: A Computational Fluid Dynamics (CFD) model of blood flow through the pump is developed. The velocity and shear stress fields from the CFD solution are used with a hemolysis model to predict blood damage indices.
- Experimental Comparators:
- Particle Image Velocimetry (PIV): Used to obtain detailed velocity field measurements within the pump housing for comparison with the CFD-predicted flow fields.
- In Vitro Hemolysis Testing: Provides direct, physical measurements of blood damage (plasma free hemoglobin) under controlled operating conditions.
The following workflow diagram outlines the key steps in this validation protocol, from model development to the final credibility assessment.
Impact of Context of Use (COU) on Validation Rigor
The same CFD model requires different levels of validation evidence depending on the clinical application, as shown in the table below. This exemplifies the risk-informed nature of the V&V 40 framework [1].
Table 3: How Context of Use Drives Validation Requirements
| Context of Use (COU) Element | COU 1: Cardiopulmonary Bypass (CPB) | COU 2: Short-Term Ventricular Assist Device (VAD) |
|---|---|---|
| Device Classification | Class II | Class III |
| Decision Consequence | Lower (Temporary use, lower risk of severe injury) | Higher (Prolonged use, higher risk of severe injury) |
| Model Influence | Medium (Substantial contributor to decision) | High (Primary evidence for decision) |
| Overall Model Risk | Medium | High |
| Implication for Validation | Moderate validation rigor required. A defined acceptance criterion for the comparison against experimental hemolysis data must be met. | High validation rigor required. Must not only meet acceptance criteria but also demonstrate quantitative accuracy of the velocity field (vs. PIV) to build higher confidence. |
Protocol: Threshold-Based Acceptance Criterion
The FDA's threshold-based approach provides a quantitative method for setting acceptance criteria [35].
- Intended Purpose: This method is for scenarios where a well-accepted safety/performance criterion (a threshold) for the specific COU is available.
- Methodology: The approach uses the mean values and uncertainties from both the validation experiments and the model predictions, along with the known safety threshold for the quantity of interest (e.g., a maximum acceptable hemolysis level). It computes a measure of confidence that the model's prediction error is within limits that are acceptable from a safety perspective.
- Application: For example, in the blood pump case, if the safety threshold for hemolysis is known, this method can determine how closely the CFD-predicted hemolysis must match the in vitro hemolysis test results to be deemed acceptable.
Advanced Applications and Future Directions
AI and Multitask Learning in Drug Discovery
The field of drug discovery is witnessing the rise of advanced AI models that integrate predictive and generative tasks. For instance, DeepDTAGen is a multitask deep learning framework that simultaneously predicts drug-target binding affinity (DTA) and generates new target-aware drug variants [37]. The validation of such models requires sophisticated experimental comparators.
- Predictive Task Validation: DTA prediction is benchmarked on datasets like KIBA, Davis, and BindingDB. Performance is evaluated using metrics such as Mean Squared Error (MSE), Concordance Index (CI), and R-squared (r²m), which compare model predictions against experimentally measured binding affinities [37].
- Generative Task Validation: The validity, novelty, and uniqueness of generated drug molecules are assessed. Furthermore, their drug-likeness and synthesizability are computationally analyzed, providing a multi-faceted comparator for the model's generative capability [37].
The Critical Importance of Data Quality
A paramount challenge in using historical experimental data as comparators is data quality. Machine learning models are often trained on historical assay data (e.g., IC₅₀ values), but this data can be built on shaky foundations. Issues include assay drift over time due to changes in operators, machines, or software, and a lack of underlying measurement values and metadata [38]. Without statistical discipline and full traceability of experimental parameters, computational models are built on unstable ground, undermining the entire validation process.
Quantifying Uncertainty and Establishing Applicability Domains
For computational models to be deemed credible for high-impact decision-making in fields like drug development, researchers must rigorously quantify uncertainty and clearly establish applicability domains. Model credibility is defined as "the trust, established through the collection of evidence, in the predictive capability of a computational model for a context of use" [5]. This foundational concept is embraced by regulatory agencies like the U.S. Food and Drug Administration (FDA), which has issued guidance on assessing the credibility of computational modeling and simulation (CM&S) in medical device submissions [5].
Uncertainty quantification (UQ) is the science of quantitatively characterizing and reducing uncertainties in applications, serving to determine the most likely outcomes when model inputs are imperfectly known and to help designers establish confidence in predictions [39]. This process is inherently tied to the Verification and Validation (V&V) framework, where verification ensures the model is implemented correctly ("doing things right"), and validation determines its accuracy as a representation of the real world for its intended uses ("doing the right thing") [39]. Performed alongside UQ, sensitivity analysis describes the expected variability of model output with respect to variability in model parameters, allowing researchers to rank parameters by their effect on modeling output [39].
Table 1: Key Sources of Uncertainty in Computational Modeling
| Category | Source | Description |
|---|---|---|
| Input Uncertainty | Parameters & Inputs | Lack of knowledge about model parameters, initial conditions, forcings, and boundary values [40]. |
| Model Form Uncertainty | Model Discrepancy | Difference between the model and reality, even at the best-known input settings [40]. |
| Computational Uncertainty | Limited Model Evaluations | Uncertainty arising from the inability to run the computationally expensive model at all required input settings [40]. |
| Solution & Code Uncertainty | Numerical & Coding Errors | Errors in the numerical solution or the implementation/coding of the model [40]. |
The applicability domain of a model defines the boundaries within which it can be reliably applied. The concept of "nearness" of available physical observations to the predictions for the model's intended use is a critical factor in assessing prediction reliability, though rigorous mathematical definitions remain an open challenge [40]. A model used outside its applicability domain may produce results with unacceptably high uncertainty, leading to flawed conclusions.
Comparative Analysis of Uncertainty Quantification Techniques
Various methodological approaches exist for quantifying uncertainty in computational models, each with distinct strengths, weaknesses, and ideal application contexts. The choice of method often depends on the model's characteristics (e.g., computational cost, linearity) and the nature of the available data.
Table 2: Comparison of Uncertainty Quantification Techniques
| Method | Core Principle | Advantages | Limitations | Ideal Use Cases |
|---|---|---|---|---|
| Propagation of Uncertainty | Uses a truncated Taylor series to mathematically propagate input uncertainties to the output [39]. | Fast computation for closed-form models; provides analytical insight [39]. | Approximate; assumes model is well-behaved and not highly nonlinear [39]. | Closed-form, deterministic models with low nonlinearity. |
| Monte Carlo (MC) Simulation | Randomly samples from input parameter distributions to generate thousands of model runs, building an output distribution [39]. | Highly general and straightforward to implement; makes no strong assumptions about model form [39]. | Can be computationally prohibitive for models with long run times; requires many samples [39]. | Models with moderate computational cost where global sensitivity information is needed. |
| Bootstrap Ensemble Methods | Generates multiple models (an ensemble), each trained on a bootstrapped sample of the original data; uncertainty is derived from the ensemble's prediction variance [41]. | Very general and easy to parallelize; maintains features of the original model (e.g., differentiability) [41]. | The raw ensemble standard deviation often requires calibration to be an accurate UQ metric [41]. | Machine learning models (Random Forests, Neural Networks) for regression tasks. |
| Bayesian Methods | Uses Bayes' theorem to produce a posterior distribution that incorporates prior knowledge and observed data [40]. | Provides a full probabilistic description of uncertainty; naturally incorporates multiple uncertainty sources [40]. | Can be computationally intensive; requires specification of prior distributions [40]. | Complex models where fusing different information sources (simulation, physical data, expert judgment) is required. |
Performance Data and Comparative Findings
Empirical studies reveal critical insights into the practical performance of these UQ methods. A significant finding is that the raw standard deviation from a bootstrap ensemble ((\hat{\sigma}{uc})), while convenient, is often an inaccurate estimate of prediction error. However, its accuracy can be dramatically improved through a simple calibration process, yielding a calibrated estimate ((\hat{\sigma}{cal})) [41].
The accuracy of UQ methods is often evaluated using two visualization tools:
- R-Statistic Distribution: The distribution of ( r = \frac{\text{residual}}{\hat{\sigma}} ). For a perfectly accurate (\hat{\sigma}), this distribution should be a standard normal (mean=0, std=1) [41].
- Residual vs. Error (RvE) Plot: A plot of binned (\hat{\sigma}) values against the root mean square (RMS) of residuals in each bin. A perfect UQ method would follow the identity line (slope=1, intercept=0) [41].
Studies applying these evaluation methods show that calibrated bootstrap ensembles ((\hat{\sigma}_{cal})) produce r-statistic distributions much closer to the ideal standard normal and RvE plots much closer to the identity line compared to the uncalibrated approach [41]. This calibration, based on log-likelihood optimization using a validation set, has proven effective across diverse model types, including random forests, linear ridge regression ensembles, and neural networks [41].
Another underappreciated challenge in computational studies, particularly in psychology and neuroscience, is low statistical power for model selection. A power analysis framework for Bayesian model selection shows that while statistical power increases with sample size, it decreases as more candidate models are considered [42]. A review of 52 studies found that 41 had less than an 80% probability of correctly identifying the true model, often due to a failure to account for this effect of model space size [42]. Furthermore, the widespread use of fixed effects model selection (which assumes one model is "true" for all subjects) is problematic, as it has high false positive rates and is highly sensitive to outliers. The field is encouraged to adopt random effects model selection, which accounts for the possibility that different models may best describe different individuals within a population [42].
Experimental Protocols for Model Validation
A Framework for Validation and Credibility Assessment
The process of model validation is the process of assessing whether the quantity of interest (QOI) for a physical system is within a specified tolerance of the model prediction, with the tolerance determined by the model's intended use [40]. Regulatory science, as pursued by the FDA's Credibility of Computational Models Program, outlines major gaps that drive the need for rigorous experimentation, including unknown model credibility, insufficient data, and a lack of established best practices [5].
The validation process involves several key steps [40]:
- Identifying and Representing Uncertainties: Using sensitivity analysis to determine which model inputs and features significantly affect key outputs.
- Leveraging Physical Observations: Using experimental or observational data to constrain and refine the model.
- Assessing Prediction Uncertainty: Combining computational models and physical data to estimate total uncertainty.
- Assessing Prediction Reliability: A more qualitative evaluation of the model's quality, including the verification of assumptions and the concept of "nearness" to the intended use case.
Diagram 1: Model V&V and Credibility Assessment Workflow
Detailed Protocol: Calibration and Validation of a Predictive Regression Model
This protocol details the steps for using a bootstrap ensemble with calibration to quantify uncertainty, a method shown to be effective across various physical science datasets [41].
Objective: To develop a predictive model with accurate uncertainty estimates for a quantitative target property. Materials & Computational Environment:
- A dataset with features and a measured target property.
- A regression algorithm (e.g., Random Forest, Gaussian Process Regression, Neural Network).
- Computational resources for parallel processing (e.g., high-performance computing cluster).
Procedure:
- Data Partitioning: Randomly split the dataset into three parts: a training set (e.g., 70%), a validation set (e.g., 15%), and a held-out test set (e.g., 15%).
- Bootstrap Ensemble Generation:
- Generate ( B ) (e.g., 100) bootstrap samples by randomly selecting from the training set with replacement.
- Train an instance of the chosen regression model on each bootstrap sample. This creates an ensemble of ( B ) models.
- Generate Initial Predictions and Uncertainties:
- For each data point ( i ) in the validation and test sets, obtain a prediction from each of the ( B ) models.
- Calculate the final prediction ( \hat{y}i ) as the mean of the ( B ) predictions.
- Calculate the uncalibrated uncertainty ( \hat{\sigma}{uc, i} ) as the standard deviation of the ( B ) predictions.
- Calibrate the Uncertainty Estimator:
- Using the validation set, assume a linear relationship between the squared uncalibrated uncertainty and the true variance: ( \hat{\sigma}^2{cal}(x) = a \cdot \hat{\sigma}^2{uc}(x) + b ).
- Find the optimal parameters ( a ) and ( b ) by minimizing the negative log-likelihood function: ( \text{NLL} = \sum{i \in \text{validation}} \left[ \frac{(\hat{y}i - yi)^2}{a \cdot \hat{\sigma}^2{uc,i} + b} + \log(a \cdot \hat{\sigma}^2{uc,i} + b) \right] ) where ( yi ) is the measured true value.
- Apply Calibration and Validate:
- For all test set points, compute the calibrated uncertainty: ( \hat{\sigma}{cal, i} = \sqrt{a \cdot \hat{\sigma}^2{uc, i} + b} ).
- Evaluate the quality of the calibrated UQ using the RvE plot and r-statistic distribution on the test set.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The following table details key resources and tools used in computational modeling research for credibility assessment, as identified in the search results.
Table 3: Key Research Reagents and Computational Tools
| Item Name | Type | Primary Function | Relevance to Credibility |
|---|---|---|---|
| Dakota [39] | Software Tool | A general-purpose analysis toolkit for optimization, sensitivity analysis, and UQ. | Provides robust, peer-reviewed algorithms for UQ and V&V processes. |
| SBML (Systems Biology Markup Language) [2] | Model Encoding Standard | An XML-based format for representing computational models of biological processes. | Ensures model reproducibility, exchange, and reuse by providing a common, unambiguous language. |
| MIRIAM Guidelines [2] | Annotation Standard | Minimum Information Requested in the Annotation of Biochemical Models. | Enables model reproducibility and credibility by standardizing the minimal required metadata. |
| BioModels Database [2] | Model Repository | A curated database of published, peer-reviewed computational models. | Provides a source of reproducible models for validation and benchmarking against existing work. |
| ClinicalTrials.gov [43] | Data Repository | A database of privately and publicly funded clinical studies conducted around the world. | Used for retrospective clinical analysis to validate computational drug repurposing predictions. |
The rigorous quantification of uncertainty and clear demarcation of applicability domains are not standalone exercises but are fundamental pillars of modern computational model credibility standards. Frameworks from NASA and the FDA emphasize that credibility is established through the collection of evidence for a specific context of use [5] [2]. The methods and comparisons outlined here provide a scientific basis for generating that evidence.
The move towards standardized credibility assessments in fields like systems biology demonstrates the growing recognition that credible models must be reproducible, well-annotated, and accompanied by a clear understanding of their limitations [2]. As computational models increasingly inform high-stakes decisions in drug development and medical device regulation, the consistent application of these UQ and validation protocols will be paramount. The experimental data shows that techniques like calibrated bootstrap ensembles can provide accurate UQ, while statistical best practices, such as using random effects model selection and conducting power analysis, guard against overconfident and non-reproducible findings [42] [41]. By integrating these practices, researchers can provide the transparent, evidence-based justification required to build trust in their computational predictions.
Computational Fluid Dynamics (CFD) has become an indispensable tool in the design and optimization of blood-contacting medical devices such as ventricular assist devices (VADs) and extracorporeal membrane oxygenation (ECMO) pumps [44] [45]. Accurate prediction of hemolysis—the damage and destruction of red blood cells—represents a critical challenge in computational modeling, as hemolysis directly impacts patient safety and device efficacy [46] [47]. This case study examines the application of computational frameworks for hemolysis assessment within the FDA benchmark centrifugal blood pump, contextualizing methodologies and performance outcomes against the broader imperative of establishing model credibility for regulatory and clinical decision-making [7] [48].
The credibility of computational models is increasingly governed by standards such as the ASME V&V 40, which provides a risk-based framework for establishing confidence in simulation results used in medical device evaluation [7]. This analysis explores how different computational approaches to hemolysis prediction align with these emerging credibility requirements, examining both validated methodologies and innovative techniques that bridge current limitations in the field.
Comparative Performance of Turbulence Models for Hemolysis Prediction
The accuracy of CFD simulations for hemolysis prediction depends significantly on the turbulence model employed, with different models offering varying balances of computational cost, resolution of flow features, and predictive accuracy [46]. Researchers have systematically evaluated four primary turbulence modeling approaches for hemolysis prediction in the FDA benchmark centrifugal pump:
- RANS-based models (RNG k-ε and k-ω SST) provide solutions to the Reynolds-averaged Navier-Stokes equations, offering computational efficiency while modeling turbulence effects statistically [46].
- Scale-resolving models (RSM-ω and IDDES) capture a broader spectrum of turbulent scales, providing enhanced resolution of complex flow features including critical shear stress regions and vortex structures [46].
Quantitative Performance Comparison
Table 1: Performance comparison of turbulence models for hemolysis prediction in the FDA benchmark pump
| Turbulence Model | Pressure Head Prediction Error | Hemolysis Performance at 2500 RPM | Hemolysis Performance at 3500 RPM | Computational Cost |
|---|---|---|---|---|
| RNG k-ε | 1.1-4.7% | Moderate agreement | Superior agreement | Low |
| k-ω SST | 1.1-4.7% | Best performance | Moderate agreement | Low |
| RSM-ω | Higher than RANS | Best performance | Moderate agreement | Moderate |
| IDDES | Higher than RANS | Moderate agreement | Superior agreement | High |
The RANS-based models (k-ω SST and RNG k-ε) demonstrated excellent agreement in pressure head predictions, with errors of only 1.1 to 4.7% across both operating conditions [46]. For hemolysis prediction, all models produced values within the standard deviation of experimental data, though their relative accuracy varied with operating conditions [46]. The RSM-ω and k-ω SST models performed best at lower speeds (2500 RPM), while RNG k-ε and IDDES showed superior agreement at higher speeds (3500 RPM) [46].
Implications for Model Selection
The selection of an appropriate turbulence model involves balancing accuracy requirements with computational resources. While scale-resolving models (RSM-ω and IDDES) provide enhanced resolution of flow structures relevant to hemolysis, their increased computational cost may be prohibitive for design iteration cycles [46]. The strong performance of RANS-based models, particularly k-ω SST across multiple operating conditions, makes them suitable for preliminary design optimization, with scale-resolving approaches reserved for final validation of critical regions identified during development [46] [47].
Scalar Shear Stress Models and Coefficient Sets in Power-Law Hemolysis Models
Fundamentals of Power-Law Hemolysis Modeling
The power-law model remains the most widely implemented approach for computational hemolysis prediction, relating blood damage to shear stress and exposure time through the equation:
[ HI = \frac{\Delta Hb}{Hb} = C \cdot t^{\alpha} \cdot \tau^{\beta} ]
where (HI) represents the Hemolysis Index, (t) is the exposure time, (\tau) is the scalar shear stress, and (C), (\alpha), (\beta) are empirical coefficients [47] [49].
Performance of Model Combinations
Table 2: Performance of scalar shear stress models and coefficient set combinations
| Scalar Shear Stress Model | Coefficient Set | Prediction Accuracy vs. Experimental Data | Remarks |
|---|---|---|---|
| Model A | Set 1 | Within experimental error limits | Recommended combination |
| Model B | Set 2 | Overestimated hemolysis | Consistent overestimation |
| Model C | Set 3 | Overestimated hemolysis | Poor performance at high flow rates |
| Model A | Set 4 | Overestimated hemolysis | Moderate overestimation |
| Model B | Set 5 | Overestimated hemolysis | Significant overestimation |
Research indicates that the specific combination of scalar shear stress model and coefficient set significantly influences prediction accuracy [49]. Among the various combinations tested, only one specific pair of scalar-shear-stress model and coefficient set produced results within the error limits of experimental measurements, while all other combinations overestimated hemolysis [49]. This finding underscores the critical importance of model and parameter selection in achieving clinically relevant predictions.
Mesh Independence Considerations
Mesh refinement studies represent an essential component of calculation verification for hemolysis prediction [7]. Systematic mesh refinement must be applied to avoid misleading results, particularly for unstructured meshes with nonuniform element sizes [7]. The complex relationship between mesh resolution and hemolysis prediction accuracy necessitates rigorous mesh independence testing based on both hemolysis indices and pressure head to ensure result credibility [49].
Experimental Validation Frameworks
Standard Hemolysis Testing
Experimental validation of computational hemolysis predictions typically follows modified ASTM1841-19 standards, which involve running the medical device with human or animal blood for several hours followed by measurement of free plasma hemoglobin (pfHb) released by damaged red blood cells [50]. These tests have been adapted for research purposes through volume reduction to 180mL and test duration reduction to 120 minutes, enabling multiple experimental runs within a single day [50]. The FDA benchmark pump is typically evaluated at standardized operating conditions, including 3500 rpm at 2.5 L/min (flow condition #2) and 2500 rpm at 6 L/min [46] [50].
Advanced Fluorescent Hemolysis Detection
Innovative approaches to experimental hemolysis assessment include Fluorescent Hemolysis Detection (FHD), which employs a two-phase blood analog fluid composed of calcium-loaded ghost cells (hemoglobin-depleted red blood cells) suspended in phosphate-buffered saline [50]. This method utilizes a calcium-sensitive fluorescent indicator that activates upon calcium release during ghost cell hemolysis, enabling spatial localization of hemolysis within the device [50].
Diagram 1: Experimental workflow for fluorescent hemolysis detection using ghost cell-based blood analog fluid
FHD has demonstrated capability to identify localized hemolysis regions within the FDA pump, particularly at the rotor tip and bifurcation at the diffuser, with quantitative fluorescence increases of 8.85/min at 3500 rpm and 2.5 L/min flow conditions [50]. This approach bridges a critical gap between standard hemolysis tests and simulation methods by providing spatially resolved experimental data for model validation [50].
Mock Circulatory Loop Validation
Computational models are typically validated against experimental data obtained from mock circulatory loops incorporating pressure sensors, ultrasonic flowmeters, and reservoir systems [47]. These systems utilize blood-mimicking fluids with density and viscosity matching human blood (typically 1.055 kg/m³ density and 3.5×10⁻³ Pa·s dynamic viscosity) [47]. Validation involves comparison of normalized flow-rate pressure-rise characteristic curves between experimental and CFD results, with studies reporting maximum pressure rise deviations of approximately 1% when using appropriate modeling approaches [47].
Advanced Applications and Framework Implementation
System-Level Optimization Framework
Recent advances in computational hemolysis assessment have introduced system-level optimization frameworks that couple lumped parameter models of cardiovascular physiology with parametric turbomachinery design packages [44] [48]. This approach incorporates the full Euler turbomachinery equation for pump modeling rather than relying on empirical characteristic curves, enabling more comprehensive geometric optimization [48]. The framework allows specification of both physiology-related and device-related objective functions to generate optimized blood pump configurations across large parameter spaces [48].
Application of this optimization framework to the FDA benchmark pump as a baseline design has demonstrated remarkable improvements, with the optimized design achieving approximately 32% reduction in blade tip velocity and 88% reduction in hemolysis while maintaining equivalent cardiac output and aortic pressure [44] [48]. Alternative designs generated through this process have achieved 40% reduction in blood-wetted area while preserving baseline pressure and flow characteristics [48].
Speed Modulation Strategies
Beyond constant-speed operation, computational studies have investigated hemolysis under various speed modulation patterns (sinusoidal, pulsatile) that better replicate physiological conditions and are implemented in commercial devices like HVAD and HeartMate 3 [47]. Research indicates that counter-phase modulation reduces hemolysis index fluctuations compared to in-phase conditions, while higher baseline speeds increase time-averaged hemolysis due to prolonged exposure to non-physiological shear stress [47]. These findings demonstrate that phase synchronization critically balances pulsatility and hemocompatibility, providing actionable insights for adaptive speed control strategies in clinical practice [47].
In Silico Clinical Trials
An emerging application of validated computational hemolysis models is their incorporation into in silico clinical trials—computational frameworks that could potentially replace human subjects in clinical trials for new medical devices [51] [7]. These approaches require particularly high model credibility, as they directly impact regulatory decisions and patient safety [51] [7]. Researchers have developed specific frameworks for performing in silico clinical trials and validating results, with ongoing work focused on application to cardiovascular medical devices [51]. The potential payoff includes reduced patient exposure to experimental therapies and decreased costs of expensive trials, though significant validation challenges remain [51].
Research Reagent and Computational Toolkit
Table 3: Essential research reagents and computational tools for hemolysis assessment
| Tool/Reagent | Type | Function | Example Implementation |
|---|---|---|---|
| SST-ω Turbulence Model | Computational | Resolves near-wall flow characteristics critical for shear stress prediction | ANSYS CFX 2020R1 [47] |
| Power-Law Hemolysis Model | Computational | Predicts hemolysis index based on shear stress and exposure time | HI = C·tα·τβ [47] [49] |
| Ghost Cell Blood Analog | Experimental Fluid | Enables optical measurement of localized hemolysis via fluorescence | Calcium-loaded hemoglobin-depleted RBCs [50] |
| Cal590 Potassium Salt | Fluorescent Indicator | Activates upon calcium release during hemolysis | 530 nm excitation, 590 nm emission [50] |
| Mock Circulatory Loop | Experimental Setup | Provides hydraulic performance validation under clinically relevant conditions | Pressure sensors, flowmeters, reservoir [47] |
| Euler Turbomachinery Model | Computational | Enables system-level pump optimization without empirical curves | ΔPpump = ρω²r₂² - ρω²r₁² - Qpump(···) - ΔPloss [48] |
Credibility Assessment Framework
ASME V&V 40 Standard Implementation
The credibility of computational models for hemolysis assessment is increasingly evaluated against standards such as ASME V&V 40, which provides a risk-based framework for establishing model credibility [7]. This standard has become a key enabler of the FDA CDRH framework for using computational modeling and simulation data in regulatory submissions [7]. The risk-informed approach focuses verification and validation activities on model aspects most critical to the context of use, efficiently allocating resources while establishing sufficient credibility for decision-making [7].
Model Credibility for In Silico Trials
When computational models progress toward use in in silico clinical trials, credibility requirements escalate significantly [7]. For simulations to replace human patients in trial environments, model credibility must be established to the satisfaction of diverse stakeholders, including clinicians, regulators, and patients [7]. Unique challenges emerge in validation, as direct comparison against human data is rarely possible for practical and ethical reasons [51] [7]. The ASME V&V 40 framework provides guidance for addressing these challenges through comprehensive verification, validation, and uncertainty quantification activities [7].
Diagram 2: Risk-based credibility assessment process for computational hemolysis models
This case study demonstrates that assessing hemolysis in computational blood pump models requires a multifaceted approach integrating advanced turbulence modeling, experimental validation, and systematic credibility assessment. The performance comparison reveals that while multiple modeling approaches can provide reasonable hemolysis predictions, careful selection of turbulence models, scalar stress formulations, and coefficient sets is essential for achieving results within experimental error margins [46] [49].
The emergence of comprehensive optimization frameworks coupling cardiovascular physiology with turbomachinery design represents a significant advance over traditional trial-and-error approaches, enabling dramatic reductions in predicted hemolysis through systematic geometric optimization [44] [48]. These computational advances, combined with innovative experimental techniques like fluorescent hemolysis detection, provide increasingly robust tools for evaluating blood trauma in medical devices [50].
As computational models progress toward potential use in in silico clinical trials, adherence to credibility frameworks such as ASME V&V 40 becomes increasingly critical [7]. The standardized methodologies, quantitative performance comparisons, and validation frameworks presented in this case study provide researchers with actionable guidance for implementing credible hemolysis assessment in computational blood pump models, ultimately contributing to safer and more effective blood-contacting medical devices.
Navigating Implementation Hurdles: Data, Bias, and Integration Challenges
The increasing reliance on artificial intelligence (AI) and machine learning (ML) models in high-stakes fields, including scientific research and drug development, has brought the issue of model opacity to the forefront. Often described as "black boxes," complex models like deep neural networks can deliver high-performance predictions but fail to provide insights into their internal decision-making processes [52]. This lack of transparency is a significant barrier to model credibility, as it prevents researchers from validating the underlying reasoning, identifying potential biases, or trusting the output for critical decisions [53].
Explainable AI (XAI) emerges as a critical solution to this challenge. XAI is a set of techniques and methodologies designed to make the outputs and internal workings of AI systems understandable to human users [54]. For researchers and scientists, the goal of XAI is not merely to explain but to provide a level of transparency that allows for the scrutiny, validation, and ultimate trust required for integrating computational models into the scientific process [55]. This is especially pertinent in drug development, where understanding the "why" behind a model's prediction can be as important as the prediction itself, influencing everything from target identification to patient stratification.
Foundational Concepts: Transparency, Interpretability, and Explainability
Within the discourse on trustworthy AI, the terms transparency, interpretability, and explainability are often used. For computational researchers, it is essential to distinguish them:
- AI Transparency focuses on the overarching understanding of how an AI system was created. It involves disclosure of the training data, model architecture, and the overall logic behind its decision-making processes [53]. In a research context, transparency is akin to providing the materials and methods section for an AI model.
- AI Interpretability refers to the ability to comprehend the mechanics of how a model makes decisions. It involves understanding the causal relationships between inputs and outputs and the model's internal structure [56] [53]. An interpretable model allows a scientist to predict how it will behave given a specific set of inputs.
- AI Explainability (XAI), often used interchangeably with interpretability, typically provides post-hoc justifications for specific decisions or predictions [53]. It answers the question, "Why did the model arrive at this particular result for this specific instance?" [56]
The relationship between model performance and explainability is often a trade-off. Highly complex "black box" models like ensemble methods or deep learning networks may offer superior accuracy, while simpler "glass box" models like linear regression or decision trees are inherently more interpretable but may be less powerful [52]. The field of XAI aims to bridge this gap by developing techniques that provide insight into complex models without necessarily sacrificing their performance [55].
A Taxonomy of XAI Techniques
Explainable AI techniques can be broadly categorized based on their scope and applicability. The table below summarizes the primary classes of methods relevant to scientific inquiry.
Table 1: Taxonomy of Explainable AI (XAI) Techniques
| Category | Description | Key Methods | Ideal Use Cases |
|---|---|---|---|
| Model-Specific | Explanations are intrinsic to the model's architecture. | Decision Trees, Generalized Linear Models (GLMs) | When transparency is a primary design requirement and model accuracy requirements are moderate. |
| Model-Agnostic | Methods applied after a model has been trained (post-hoc), allowing them to explain any model. | LIME, SHAP, Counterfactual Explanations | Explaining complex "black box" models (e.g., deep neural networks, random forests) in a flexible manner. |
| Local Explanations | Explain the rationale behind an individual prediction. | LIME, SHAP (local), Counterfactuals | Understanding why a specific compound was predicted to be active or why a particular patient sample was classified a certain way. |
| Global Explanations | Explain the overall behavior and logic of the model as a whole. | Partial Dependence Plots (PDP), Feature Importance, SHAP (global) | Identifying the most important features a model relies on, validating overall model behavior, and debugging the model. |
Key XAI Methods in Detail
- SHAP (SHapley Additive exPlanations): Based on cooperative game theory, SHAP assigns each feature an importance value for a particular prediction [57] [58]. It provides a unified measure of feature influence that is consistent and locally accurate, making it suitable for both local and global explanations [58]. In a research context, SHAP can quantify the contribution of each molecular descriptor in a drug response prediction.
- LIME (Local Interpretable Model-agnostic Explanations): LIME explains individual predictions by perturbing the input data and observing changes in the output [57] [58]. It creates a local, interpretable surrogate model (e.g., linear regression) that approximates the complex model's behavior around a specific instance. This is valuable for understanding anomalous or high-stakes predictions on a case-by-case basis.
- Counterfactual Explanations: This technique explains a model's decision by showing the minimal changes required to the input to alter the outcome [52] [58]. For example, it can illustrate how a molecular structure would need to be modified to change its predicted toxicity from "toxic" to "non-toxic," providing actionable insights for researchers.
The following diagram illustrates the logical workflow for selecting an appropriate XAI strategy based on research needs.
Quantitative Comparison of XAI Method Performance
Evaluating XAI systems requires specific metrics beyond standard performance indicators like accuracy. The following metrics help assess the quality and reliability of the explanations provided by XAI methods [58].
Table 2: Key Metrics for Evaluating Explainable AI Systems
| Metric | Definition | Interpretation in a Research Context |
|---|---|---|
| Faithfulness | Measures the correlation between the importance assigned to a feature by the explanation and its actual contribution to the model's prediction [58]. | A high faithfulness score ensures that the explanation accurately reflects the model's true reasoning, which is critical for validating a model's scientific findings. |
| Monotonicity | Assesses whether changes in a feature's input value consistently result in expected changes in the model's output [58]. | In a dose-response model, a high monotonicity score would indicate that an increase in concentration consistently leads to an increase in predicted effect, aligning with biological plausibility. |
| Incompleteness | Evaluates the degree to which an explanation fails to capture essential aspects of the model's decision-making process [58]. | A low incompleteness score is desired, indicating that the explanation covers the key factors behind a prediction, leaving no critical information hidden. |
The table below provides a comparative overview of popular XAI tools available to researchers, highlighting their primary functions and supported platforms.
Table 3: Comparison of AI Transparency and XAI Tools (2025 Landscape)
| Tool Name | Primary Function | Supported Platforms/Frameworks | Key Strengths |
|---|---|---|---|
| SHAP | Explain individual predictions using Shapley values from game theory. | Model-agnostic; works with TensorFlow, PyTorch, scikit-learn. | Solid theoretical foundation; consistent explanations; local and global interpretations [57] [58]. |
| LIME | Create local surrogate models to explain individual predictions. | Model-agnostic. | Intuitive concept; useful for explaining classifiers on text, images, and tabular data [57] [58]. |
| IBM AI Explainability 360 | A comprehensive open-source toolkit offering a wide range of XAI algorithms. | Includes multiple explanation methods beyond LIME and SHAP. | Offers a unified library for experimenting with different XAI techniques [57]. |
| TransparentAI | A commercial tool for tracking, auditing, and reporting on AI models. | TensorFlow, PyTorch. | Comprehensive model audit reports and bias identification features [59]. |
Experimental Protocols for XAI Evaluation
To ensure the credibility of computational models, the evaluation of their explainability should be as rigorous as the evaluation of their predictive performance. The following protocol outlines a standard methodology for benchmarking XAI techniques.
Protocol: Benchmarking XAI Methods for Feature Importance
1. Objective: To evaluate and compare the faithfulness and robustness of different XAI methods (e.g., SHAP, LIME) in identifying feature importance for a given predictive model.
2. Materials & Dataset:
- A benchmark dataset with known ground-truth relationships (e.g., a synthetic dataset where feature contributions are pre-defined, or a well-studied public dataset like MoleculeNet for cheminformatics).
- A trained predictive model (e.g., a Random Forest or a Deep Neural Network).
- XAI libraries (e.g.,
shap,lime). - Computing environment with necessary Python/R packages.
3. Procedure:
- Step 1: Model Training. Train the predictive model on the selected dataset and record its performance (e.g., AUC-ROC, R²) on a held-out test set.
- Step 2: Explanation Generation. Apply each XAI method (SHAP, LIME) to the test set to generate feature importance scores for each prediction.
- Step 3: Faithfulness Evaluation.
- For a given instance, systematically remove or perturb the top-k features identified as most important by the XAI method.
- Observe the change in the model's prediction output.
- A sharp drop in model accuracy or a significant change in the prediction score indicates high faithfulness, as the explanation correctly identified the most critical features.
- Step 4: Robustness Evaluation.
- Slightly perturb the input data (e.g., add small Gaussian noise) and re-run the XAI method.
- Measure the stability of the resulting feature importance rankings (e.g., using Rank-Biased Overlap). Stable rankings indicate a robust explanation method.
- Step 5: Analysis. Compare the results across XAI methods, focusing on their computational efficiency, stability, and alignment with domain knowledge.
The workflow for this experimental protocol is visualized below.
The Scientist's Toolkit: Essential Research Reagents for XAI
Implementing and researching XAI requires a combination of software tools, libraries, and theoretical frameworks. The following table details key "reagents" for a computational scientist's toolkit.
Table 4: Essential Research Reagents for Explainable AI
| Tool/Reagent | Type | Primary Function | Research Application |
|---|---|---|---|
| SHAP Library | Software Library | Computes Shapley values for any model. | Quantifying the marginal contribution of each input feature to a model's prediction for both local and global analysis [57] [58]. |
| LIME Package | Software Library | Generates local surrogate models for individual predictions. | Interpreting specific, high-stakes predictions from complex models by creating a simple, trustworthy local approximation [57] [58]. |
| Partial Dependence Plots (PDP) | Analytical Method | Visualizes the relationship between a feature and the predicted outcome. | Understanding the global average effect of a feature on the model's predictions, useful for validating biological monotonicity [58]. |
| Counterfactual Generators | Software Algorithm | Creates instances with minimal changes that lead to a different prediction. | Hypothesis generation by exploring the decision boundaries of a model (e.g., "What structural change would make this compound non-toxic?") [52] [58]. |
| AI Fairness 360 (AIF360) | Software Toolkit | Detects and mitigates bias in ML models. | Auditing models for unintended bias related to protected attributes, ensuring equitable and ethical AI in healthcare applications [57]. |
The journey toward widespread and credible adoption of AI in scientific research and drug development is inextricably linked to solving the "black box" problem. Strategies for model transparency and Explainable AI are not merely supplementary but foundational to this effort. By leveraging a growing toolkit of rigorous methods—from SHAP and LIME to counterfactual analysis—and adopting standardized evaluation protocols, researchers can move beyond blind trust to evidence-based confidence in their computational models. The integration of robust XAI practices ensures that models are not just predictive but are also interpretable, accountable, and ultimately, more valuable partners in the scientific discovery process. As regulatory frameworks like the EU AI Act continue to evolve, emphasizing transparency and accountability, the principles of XAI will undoubtedly become a standard component of computational model credibility research [54] [53].
Mitigating Bias in AI Models and Ensuring Data Quality for Representative Training
The integration of Artificial Intelligence (AI) and Machine Learning (ML) into drug development promises to revolutionize how therapies are discovered, developed, and delivered. However, the credibility of these computational models hinges on addressing a fundamental challenge: the mitigation of bias and the assurance of high-quality, representative training data [60]. Biased AI systems can produce systematically prejudiced results that perpetuate historical inequities and compromise scientific integrity [61]. For researchers and scientists, this is not merely a technical obstacle but a core component of establishing model credibility, as defined by emerging regulatory frameworks from the FDA and EMA [62] [63]. This guide objectively compares methodologies for bias mitigation, providing experimental protocols and data to support the development of credible, fair, and effective AI models in biomedical research.
Understanding AI Bias: Typology and Impact on Model Credibility
Algorithmic bias in AI systems occurs when automated decision-making processes systematically favor or discriminate against particular groups, creating reproducible patterns of unfairness that can scale across millions of decisions [61]. In the high-stakes context of drug development, such biases can directly impact patient safety and the generalizability of research findings, thereby undermining model credibility [60].
A Taxonomy of AI Bias in Biomedical Research
Bias can infiltrate AI systems through multiple pathways. Understanding these typologies is the first step toward mitigation.
- Sampling Bias: Occurs when training datasets do not represent the population the AI system will serve [61]. For instance, if a model for diagnosing skin cancer is trained predominantly on images of lighter-skinned individuals, its accuracy will be lower for patients with darker skin tones [61].
- Historical Bias: Results from training AI on data that reflects past societal or institutional discrimination. An AI recruitment tool trained on historical hiring data that favored male candidates may subsequently discriminate against qualified female applicants [61].
- Measurement Bias: Emerges from inconsistent or culturally biased data measurement methods, potentially skewing data collection across different clinical sites or patient groups [61].
- Confirmation Bias: Happens when algorithm designers unconsciously build their own assumptions into the model's design, potentially overlooking critical variables or relationships [61].
The High Stakes: Real-World Impacts of AI Bias
The consequences of unchecked bias extend beyond technical performance metrics to tangible business, regulatory, and patient risks.
- Patient Harm and Healthcare Disparities: AI bias in healthcare can lead to diagnostic errors for underrepresented groups. A 2019 study revealed that skin cancer detection algorithms showed significantly lower accuracy for darker skin tones, risking missed diagnoses [61]. During the COVID-19 pandemic, pulse oximeter algorithms overestimated blood oxygen levels in Black patients, leading to delayed treatment [61].
- Regulatory and Reputational Damage: Regulatory agencies are increasingly focusing on bias and fairness. The EMA's framework mandates explicit assessment of data representativeness and strategies to address potential discrimination [60]. Companies face legal liabilities and reputational harm if biased AI systems lead to unfair outcomes, as seen with Amazon's hiring algorithm [61].
- Compromised Model Credibility and Drug Development Failures: A model whose predictions are not generalizable across diverse populations lacks credibility and is of limited use in regulatory decision-making [64] [62]. This can lead to costly late-stage failures in clinical trials if drug efficacy or safety profiles are not accurately predicted for the entire target population.
Comparative Analysis of Bias Mitigation Strategies and Data Quality Frameworks
A multi-faceted approach is required to tackle bias, spanning the entire AI lifecycle from data collection to model deployment and monitoring. The following section provides a structured comparison of these strategies.
Data-Centric Mitigation Protocols
The principle of "garbage in, garbage out" is paramount. Mitigating bias begins with the data itself [65] [66].
Table 1: Comparative Analysis of Data-Centric Bias Mitigation Techniques
| Technique | Experimental Protocol & Methodology | Key Performance Metrics | Impact on Model Fairness |
|---|---|---|---|
| Comprehensive Data Analysis & Profiling [65] [66] | Conduct statistical analysis to quantify representation across demographic groups. Profile data across transformation layers (e.g., bronze, silver, gold in a medallion architecture) to trace bias origins. | Percentage of incomplete records; Rate of representation disparity; Number of duplicate records. | Establishes a baseline for data representativeness; identifies systemic gaps in data collection. |
| Data Augmentation & Resampling [66] | Oversampling: Increase representation of underrepresented groups by duplicating or generating synthetic samples. Undersampling: Reduce over-represented groups to balance the dataset. | Performance accuracy parity across groups; Change in F1-score for minority classes; Reduction in disparity of error rates. | Directly improves model performance on underrepresented subgroups, enhancing equity. |
| Fairness-Aware Data Splitting [66] | Ensure training, validation, and test sets are stratified to maintain proportional representation of all key subgroups. | Consistency of model performance metrics between training and test sets across all subgroups. | Prevents overfitting to majority groups and provides a realistic assessment of model generalizability. |
| Data Anonymization [66] | Implement techniques like pseudonymization or differential privacy to protect individual privacy and reduce the risk of bias linked to sensitive attributes. | Re-identification risk score; Utility loss (drop in model accuracy post-anonymization). | Helps prevent proxy discrimination by removing or masking direct identifiers, though may not eliminate all bias. |
Algorithmic and Model-Level Fairness Strategies
Once data is curated, the focus shifts to the algorithms that learn from it.
Table 2: Comparison of Algorithmic Fairness and Governance Approaches
| Strategy | Methodology & Implementation | Experimental Evaluation | Regulatory Alignment |
|---|---|---|---|
| Fairness-Aware Machine Learning [66] | Implement algorithms that explicitly incorporate fairness constraints or objectives during training (e.g., reducing demographic parity differences). | Audit model outputs for disparate impact using metrics like Equalized Odds or Statistical Parity Difference. | Aligns with EMA and FDA emphasis on quantifying and mitigating bias, supporting credibility assessments [62]. |
| Fairness Constraints & Regularization [66] | Apply mathematical constraints or add penalty terms to the model's loss function to punish biased outcomes during the optimization process. | Measure the trade-off between overall model accuracy and fairness metrics; evaluate convergence behavior. | Demonstrates a proactive, quantitative approach to bias mitigation, which is valued in regulatory submissions. |
| Explainability & Interpretability Methods [60] [66] | Use tools like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to decipher "black-box" model decisions. | Qualitative assessment by domain experts to validate if model reasoning aligns with biological knowledge. | The EMA expresses a preference for interpretable models and requires explainability metrics for "black-box" models [60]. |
| Continuous Monitoring & Auditing [65] [66] | Deploy automated systems to track model performance and fairness metrics in production, detecting concept drift or performance decay. | Set up dashboards with alerts triggered when fairness metrics dip below pre-defined thresholds. | Mirrors FDA and EMA requirements for ongoing performance monitoring and post-market surveillance of AI tools [62] [63]. |
The following workflow diagram synthesizes the core steps for implementing a robust bias mitigation strategy, integrating both data-centric and algorithmic approaches.
Regulatory Perspectives on Bias and Credibility
Regulatory bodies have made the management of bias and data quality a central pillar of their evolving frameworks for AI in drug development, directly linking it to model credibility.
- FDA's Risk-Based Credibility Framework: The FDA's 2025 draft guidance outlines a risk-based approach for evaluating AI models, where "credibility" is defined as the measure of trust in an AI model’s performance for a given "Context of Use" (COU) [62]. A key factor in establishing this credibility is addressing challenges like "Data Variability" and the "potential for bias and unreliability introduced by variations in training data quality, volume, and representativeness" [62].
- EMA's Structured, Risk-Tiered Approach: The EMA's 2024 Reflection Paper establishes a regulatory architecture that mandates "explicit assessment of data representativeness, and strategies to address class imbalances and potential discrimination" [60]. It holds sponsors accountable for ensuring AI systems are "fit for purpose" and align with legal and ethical standards, particularly for "high patient risk" applications [60].
- Convergence on Core Principles: Both agencies emphasize transparency, robust documentation, and the need for ongoing monitoring. The EMA explicitly prohibits incremental learning during clinical trials to ensure evidence integrity, while the FDA's "Learn and Confirm" paradigm encourages iterative model refinement within a controlled framework [60] [64] [62].
Experimental Data and Case Studies in Model Validation
Theoretical frameworks are validated through practical application. The following case studies and experimental data highlight both the challenges of bias and the methodologies for ensuring model credibility.
Case Study: Facial Recognition in Medical Imaging
A landmark study, the "Gender Shades" project, audited commercial gender classification systems and found dramatic disparities. These systems showed error rates of up to 34.7% for darker-skinned females compared to 0.8% for lighter-skinned males [61]. This case study is a powerful example of how sampling and representation bias can lead to highly inequitable outcomes.
- Experimental Protocol: The methodology involved testing the APIs of major tech companies (IBM, Microsoft, Face++) using a diverse dataset of faces (Parliament members from three African and three European countries). Performance was evaluated by intersecting gender and skin tone categories [61].
- Implication for Drug Development: This underscores the critical need for diverse, representative datasets in medical AI. A diagnostic algorithm trained on non-representative data will inevitably perform worse for underrepresented patient groups, directly impacting care quality and model credibility.
Case Study: Credibility in Systems Biology Modeling
Eggertsen et al. (2025) demonstrated how a complex, logic-based model of cardiomyocyte signaling (comprising 167 nodes and 398 reactions) could be used to predict and validate drug mechanisms [67]. This study highlights the balance between complexity and credibility.
- Experimental Workflow: The researchers combined computational modeling with a multi-stage experimental validation process. Predictions from the in silico model were rigorously tested through in vitro experiments, in vivo animal studies, and analysis of retrospective clinical data [67].
- Credibility Assessment: The model's credibility was established not by perfect accuracy, but by its transparent validation against empirical data and its ability to resolve contradictions in the existing literature. The study transparently reported that the original model replicated 77% of experiments from 450 studies, a realistic accuracy given the known reproducibility rates in biological science [67].
The following diagram maps this iterative "Learn and Confirm" paradigm, which is central to building credible computational models.
Building credible, bias-aware AI models requires a suite of methodological, computational, and governance tools. This toolkit details essential resources for researchers.
Table 3: Research Reagent Solutions for Bias-Aware AI Model Development
| Tool Category | Specific Tool/Technique | Function & Application in Drug Development |
|---|---|---|
| Data Quality & Profiling [65] | Data Quality Metrics (Completeness, Uniqueness, Timeliness); Data Catalogs with Lineage | Quantifies fitness-for-purpose of datasets used in, e.g., patient stratification for clinical trials. Lineage traces error origins. |
| Bias Detection & Fairness Metrics [61] [66] | Statistical Parity; Equalized Odds; Disparate Impact Ratio; Bias Detection Algorithms | Algorithmically audits datasets and model outputs for unfair disparities across protected classes (race, sex, age). |
| Fairness-Aware ML Libraries [66] | AIF360 (IBM); Fairlearn (Microsoft) | Provides pre-implemented algorithms for mitigating bias during model training and for evaluating model fairness. |
| Explainability (XAI) Tools [60] [66] | SHAP; LIME; Partial Dependence Plots | Interprets "black-box" models like deep neural networks, providing insights into feature importance for model predictions. |
| Model Governance & Monitoring [65] [63] | ML Model Registries; Continuous Monitoring Dashboards; FDA's "QMM" and "Credibility Assessment" Frameworks | Tracks model versions, performance, and fairness metrics over time. Aligns development with regulatory expectations for credibility. |
Mitigating bias and ensuring data quality are not standalone technical tasks but foundational to the credibility of computational models in drug development. As regulatory frameworks from the FDA and EMA mature, a systematic approach—encompassing comprehensive data management, algorithmic fairness, and continuous monitoring—becomes a scientific and regulatory imperative [60] [62] [63]. The experimental protocols and comparative data presented herein provide a roadmap for researchers and scientists to build AI models that are not only powerful but also equitable, reliable, and worthy of trust in the critical mission of bringing safe and effective therapies to patients.
The AI Talent Crisis in Pharma and Biotech
The pharmaceutical and biotechnology industries are in the midst of a profound transformation driven by artificial intelligence (AI). From drug discovery and clinical trials to manufacturing and commercial operations, AI promises to unlock billions of dollars in value while accelerating the development of new therapies [68]. According to industry analysis, AI is projected to generate between $350 billion and $410 billion annually for the pharmaceutical sector by 2025 [68]. This technological revolution hinges on having a workforce capable of building, deploying, and governing AI systems—a requirement that has created a critical talent shortage.
The AI talent gap represents a significant mismatch between the AI-related competencies pharmaceutical companies need and the capabilities their existing workforces possess [69]. In a recent survey of industry professionals, 49% of respondents reported that a shortage of specific skills and talent is the top hindrance to their company's digital transformation [69]. Similarly, a Pistoia Alliance survey found that 44% of life-science R&D organizations cited a lack of skills as a major barrier to AI and machine learning adoption [69]. This shortage encompasses both technical expertise in machine learning and data science, as well as domain knowledge specific to pharmaceutical sciences and regulatory requirements.
The shortage is not merely a human resources challenge—it has tangible impacts on innovation and patient care. Companies lacking skilled AI professionals struggle to implement technologies promptly, resulting in missed opportunities and project delays [70]. More than a third of technology specialists have experienced AI project delays lasting up to six months, primarily due to AI skills shortages and budget constraints [70]. This slowdown threatens to impede the industry's ability to deliver novel treatments to patients efficiently.
Table 1: Global AI Talent Supply-Demand Imbalance (2025)
| Region | Open AI Positions | Available Talent Pool | Supply-Demand Ratio | Average Time to Fill |
|---|---|---|---|---|
| North America | 487,000 | 156,000 | 1:3.1 | 4.8 months |
| Europe | 312,000 | 118,000 | 1:2.6 | 5.2 months |
| Asia-Pacific | 678,000 | 189,000 | 1:3.6 | 4.1 months |
| Global Total | 1,633,000 | 518,000 | 1:3.2 | 4.7 months |
Quantifying the Talent Gap: A Data-Driven Analysis
Scope and Impact of the Shortage
The AI talent shortage extends beyond a simple headcount deficit. It represents a multifaceted challenge involving technical skills deficits, domain knowledge shortfalls, and insufficient data literacy across organizations. The situation is particularly acute for roles that require both technical AI expertise and pharmaceutical domain knowledge. Approximately 70% of pharma hiring managers report difficulty finding candidates who possess both deep pharmaceutical knowledge and AI skills [69]. These "AI translators"—professionals who can bridge the gap between technical and domain expertise—are in critically short supply.
The financial implications of this talent gap are substantial. AI roles command significant salary premiums, with professionals possessing AI skills earning 56% more on average than their peers in similar roles without AI expertise [71]. This wage inflation is particularly pronounced for specialized positions. For machine learning engineers at senior levels, total compensation can reach $450,000, while AI research scientists can command packages up to $550,000 [72]. This compensation environment creates intense competition for talent, with large pharmaceutical companies often outbidding smaller firms and startups for the limited pool of qualified candidates.
The talent shortage also varies significantly by specialization and technical skill set. The most severe shortages exist in emerging and highly specialized areas such as Large Language Model (LLM) development, AI ethics and governance, and MLOps (Machine Learning Operations). These areas have demand scores exceeding 85 out of 100 but supply scores below 35, creating critical gaps that hinder organizational ability to implement and scale AI solutions responsibly [72].
Table 2: Most Critical AI Roles and Shortage Levels in Pharma
| Role Category | Open Positions | Qualified Candidates | Shortage Level | YoY Demand Growth |
|---|---|---|---|---|
| AI Research Scientists | 89,000 | 23,000 | Critical (1:3.9) | +134% |
| AI Ethics & Governance Specialists | 34,000 | 8,900 | Critical (1:3.8) | +289% |
| Machine Learning Engineers | 234,000 | 67,000 | Severe (1:3.5) | +89% |
| NLP/LLM Specialists | 45,000 | 14,000 | Critical (1:3.2) | +198% |
| Data Scientists (AI/ML Focus) | 198,000 | 78,000 | High (1:2.5) | +67% |
| AI Product Managers | 67,000 | 31,000 | Moderate (1:2.2) | +156% |
Regulatory Context and Model Credibility
The talent shortage takes on added significance within the framework of regulatory requirements for AI in drug development. The U.S. Food and Drug Administration (FDA) has issued draft guidance providing recommendations on the use of AI intended to support regulatory decisions about drug and biological products [73]. This guidance emphasizes ensuring model credibility—defined as trust in the performance of an AI model for a particular context of use [73]. The FDA recommends a risk-based framework for sponsors to assess and establish AI model credibility and determine the activities needed to demonstrate that model output is trustworthy for its intended use [73].
This regulatory framework has direct implications for talent requirements. Organizations must now possess or develop expertise in AI governance, model validation, and documentation practices that align with regulatory expectations. The FDA's approach requires defining the context of use—how an AI model addresses a specific question of interest—which demands personnel who understand both the technical aspects of AI and the scientific and regulatory context of pharmaceutical development [73]. This intersection of skills represents perhaps the most challenging aspect of the talent shortage, as it requires professionals who can navigate both technical and regulatory landscapes.
Strategic Approach 1: Upskilling and Reskilling Internal Talent
Building Internal AI Capability
Upskilling existing employees represents one of the most effective strategies for addressing the AI talent shortage in pharmaceuticals. Reskilling internal teams is not only cost-effective—approximately half the cost of hiring new talent—but also offers significant secondary benefits, including improved employee retention and organizational knowledge preservation [69]. Companies that have implemented structured upskilling programs report a 25% boost in retention and 15% efficiency gains [69]. These programs allow organizations to develop talent with both AI expertise and valuable institutional knowledge of company-specific processes, systems, and culture.
Leading pharmaceutical companies have launched substantial upskilling initiatives. Johnson & Johnson, for instance, has trained 56,000 employees in AI skills, embedding AI literacy across the organization [69]. Similarly, Bayer partnered with IMD Business School to upskill over 12,000 managers globally, achieving an 83% completion rate [69]. These programs recognize that different roles require different AI competencies—while data scientists may need deep technical skills, research scientists and clinical development professionals may require greater emphasis on AI application and interpretation within their domains.
Successful upskilling initiatives typically incorporate multiple learning modalities, including instructor-led training, online courses, hands-on workshops, and mentorship programs. They also recognize the importance of coupling technical training with education on regulatory considerations and ethical implications of AI use in drug development. This comprehensive approach ensures that upskilled talent can not only implement AI solutions but do so in a manner that aligns with regulatory expectations and organizational values.
Experimental Protocol for Evaluating Upskilling Effectiveness
Objective: To assess the impact of a structured AI upskilling program on model development efficiency and model credibility in a pharmaceutical R&D context.
Methodology:
- Participant Selection: Recruit 50 employees with life sciences backgrounds but limited AI experience. Randomly assign them to experimental (structured upskilling) and control (no formal training) groups.
- Training Intervention: Implement a 12-week structured program covering:
- Foundations of machine learning and deep learning
- Data preprocessing and feature engineering
- Model validation and interpretation techniques
- Regulatory considerations for AI in drug development (including FDA guidance on AI credibility)
- Hands-on exercises with pharmaceutical datasets
- Assessment Framework:
- Pre-/Post-Testing: Evaluate technical knowledge through standardized assessments
- Practical Challenge: Task both groups with developing predictive models for compound toxicity using identical datasets
- Model Evaluation: Blind assessment of resulting models by independent experts based on:
- Predictive accuracy (AUC-ROC, precision-recall)
- Model documentation completeness
- Adherence to regulatory standards for model credibility
- Computational efficiency
- Longitudinal Tracking: Monitor career progression and project contributions for 12 months post-training
Evaluation Metrics:
- Technical knowledge assessment scores
- Model performance metrics
- Model credibility assessment scores
- Time to model development
- Participant confidence surveys
- Career advancement rates
Diagram 1: Upskilling Effectiveness Evaluation Protocol
Strategic Approach 2: Leveraging AI-as-a-Service
Accessing External Expertise
AI-as-a-Service (AIaaS) provides an alternative approach to addressing talent shortages by allowing pharmaceutical companies to access specialized AI capabilities without developing them in-house. This model encompasses a range of services, from cloud-based AI platforms and pre-built models to fully managed AI solutions tailored to specific drug development applications. AIaaS is particularly valuable for organizations that lack the resources or time to build comprehensive AI teams, enabling them to leverage external expertise while focusing internal resources on core competencies.
The AIaaS model offers several distinct advantages for pharmaceutical companies facing talent constraints. It provides immediate access to cutting-edge AI capabilities without the lengthy recruitment process required for specialized roles [70]. It reduces the need for large upfront investments in AI infrastructure and talent acquisition, converting fixed costs into variable expenses aligned with project needs. Perhaps most importantly, it allows pharmaceutical companies to leverage domain-agnostic AI expertise from technology partners while providing the necessary pharmaceutical context internally [68].
The market for AIaaS in pharma has grown substantially, with numerous partnerships and collaborations forming between pharmaceutical companies and AI technology providers. Alliances focused on AI-driven drug discovery have skyrocketed—from just 10 collaborations in 2015 to 105 by 2021 [68]. These partnerships demonstrate the industry's recognition that external collaboration is essential to compensate for internal talent gaps and accelerate AI adoption.
Experimental Protocol for Evaluating AI-as-a-Service Solutions
Objective: To compare the efficiency, cost-effectiveness, and model credibility of internally developed AI solutions versus AI-as-a-Service platforms for drug target identification.
Methodology:
- Problem Formulation: Define a standardized drug target identification challenge using a publicly available dataset (e.g., LINCS L1000 gene expression data).
- Participant Groups:
- Internal Team: 5 company data scientists with biological domain knowledge
- AIaaS Group: 3 leading AI-as-a-Service platforms specialized in drug discovery
- Hybrid Approach: Internal team using AIaaS tools
- Implementation Phase:
- Each group addresses the same target identification problem
- Internal team uses company infrastructure and standard workflows
- AIaaS groups utilize their respective platforms with minimal customization
- Hybrid group integrates AIaaS tools into company workflows
- Evaluation Framework:
- Performance Metrics: Prediction accuracy, precision, recall, F1-score
- Efficiency Metrics: Project timeline, personnel hours, computational costs
- Credibility Assessment: Alignment with FDA guidance on AI credibility, documentation completeness, reproducibility
- Business Impact: Potential therapeutic value of identified targets
Controls and Validation:
- All groups use identical training and validation datasets
- Independent panel of therapeutic area experts evaluates biological plausibility of predictions
- Standardized documentation template for model transparency
- Computational cost tracking across all approaches
Diagram 2: AI-as-a-Service Evaluation Framework
Comparative Analysis: Upskilling vs. AI-as-a-Service
When evaluating strategies to address AI talent shortages, pharmaceutical companies must consider multiple dimensions, including implementation timeline, cost structure, regulatory alignment, and long-term capability building. The following comparative analysis outlines the relative strengths and considerations of each approach across key parameters relevant to drug development.
Table 3: Strategic Comparison: Upskilling vs. AI-as-a-Service
| Parameter | Upskilling Internal Talent | AI-as-a-Service |
|---|---|---|
| Implementation Timeline | 6-18 months for comprehensive program | 1-3 months for initial deployment |
| Cost Structure | High upfront investment, long-term ROI | Subscription/pay-per-use, operational expense |
| Regulatory Alignment | Easier to maintain control over model credibility documentation | Requires careful vendor management and audit trails |
| Domain Specificity | Can be tailored to specific therapeutic areas and internal data | May require customization to address specific use cases |
| Model Transparency | Higher visibility into model development and assumptions | Varies by provider; potential "black box" challenges |
| Long-term Capability | Builds sustainable internal expertise | Limited knowledge retention if partnership ends |
| Flexibility | Can adapt to evolving organizational needs | Dependent on vendor roadmap and capabilities |
| Risk Profile | Execution risk in program effectiveness | Vendor lock-in, data security, and business continuity |
The comparative analysis reveals that upskilling and AI-as-a-Service are not mutually exclusive strategies but can function as complementary approaches. Upskilling programs build foundational knowledge that enhances an organization's ability to effectively evaluate, select, and implement AIaaS solutions. Conversely, AIaaS platforms can provide immediate capabilities while upskilling programs develop long-term internal expertise.
The optimal balance between these approaches depends on organizational factors including strategic priorities, available resources, and timeline requirements. Companies with sufficient lead time and strategic focus on AI as a core competency may prioritize upskilling, while organizations needing rapid capability deployment may lean more heavily on AIaaS solutions. Many successful pharmaceutical companies employ a hybrid strategy, using AIaaS for specific applications while simultaneously building internal capabilities through targeted upskilling.
The Scientist's Toolkit: Essential Research Reagents for AI Credibility
Establishing model credibility requires both technical resources and methodological rigor. The following toolkit outlines essential components for developing and validating AI models in pharmaceutical research, aligned with regulatory standards for computational model credibility.
Table 4: Research Reagent Solutions for AI Model Credibility
| Research Reagent | Function | Implementation Example |
|---|---|---|
| Standardized Benchmark Datasets | Provides consistent basis for model validation and comparison | TCGA (The Cancer Genome Atlas) for oncology models, LINCS L1000 for drug response prediction |
| Model Interpretability Libraries | Enables explanation of model predictions and feature importance | SHAP (SHapley Additive exPlanations), LIME (Local Interpretable Model-agnostic Explanations) |
| MLOps Platforms | Supports version control, reproducibility, and lifecycle management | MLflow, Kubeflow for experiment tracking and model deployment |
| Fairness Assessment Tools | Identifies potential biases in model predictions | AI Fairness 360, Fairlearn for demographic parity and equality of opportunity metrics |
| Model Documentation Frameworks | Standardizes documentation for regulatory review | Model cards, datasheets for datasets following FDA guidance |
| Adversarial Validation Tools | Tests model robustness against manipulated inputs | ART (Adversarial Robustness Toolbox) for vulnerability assessment |
| Cross-validation Frameworks | Ensures model performance generalizability | Nested cross-validation, group-wise splitting for temporal or clustered data |
| Uncertainty Quantification Methods | Characterizes confidence in model predictions | Bayesian neural networks, conformal prediction, Monte Carlo dropout |
The AI talent shortage in pharmaceuticals represents a significant challenge but also an opportunity to rethink traditional approaches to workforce development and technology adoption. The most successful organizations will likely embrace a hybrid strategy that combines strategic upskilling of internal talent with selective use of AI-as-a-Service solutions. This approach balances the need for immediate capability access with long-term capacity building, creating organizations that are both agile in the short term and sustainable in the long term.
Critical to this hybrid approach is the development of "AI translator" roles—professionals who can bridge technical and domain expertise [69]. These individuals play a crucial role in ensuring that AI solutions address meaningful pharmaceutical problems while maintaining alignment with regulatory standards for model credibility. Investing in these boundary-spanning capabilities may yield greater returns than focusing exclusively on deep technical expertise.
As the FDA and other regulatory agencies continue to refine their approach to AI evaluation, pharmaceutical companies must prioritize talent strategies that emphasize not just technical capability but also regulatory literacy and ethical considerations [73] [74]. The organizations that will thrive in this evolving landscape are those that recognize AI talent as a multidimensional challenge requiring equally multidimensional solutions combining internal development, external partnerships, and continuous adaptation to regulatory expectations.
Integrating Credibility Practices with Legacy Systems and Workflows
For researchers and drug development professionals, computational modeling and simulation (CM&S) has become an indispensable tool for evaluating medical device safety and effectiveness. The U.S. Food and Drug Administration (FDA) has issued specific guidance for assessing the credibility of CM&S in regulatory submissions, providing a risk-informed framework for evaluation [3]. This guidance applies specifically to physics-based, mechanistic, or other first-principles-based models, while explicitly excluding standalone machine learning or artificial intelligence-based models [5].
The FDA defines credibility as the trust, based on all available evidence, in the predictive capability of a computational model [5]. This concept is particularly challenging when implementing within established legacy systems and workflows, where outdated architectures and documentation gaps complicate adherence to modern credibility standards. The Credibility of Computational Models Program at the FDA's Center for Devices and Radiological Health (CDRH) actively researches these challenges to help ensure computational models used in medical device development meet rigorous standards [5].
Integrating these credibility practices requires a strategic approach that respects the value of existing legacy systems while implementing necessary enhancements to meet credibility standards. This integration enables organizations to leverage existing investments while adopting new technologies that drive innovation and maintain regulatory compliance [75].
Foundational Credibility Standards and Frameworks
Regulatory Foundations for Credibility Assessment
The FDA's framework for assessing credibility provides manufacturers with a structured approach to demonstrate that CM&S models used in regulatory submissions are credible [5]. This guidance aims to improve consistency and transparency in the review of CM&S evidence, increase confidence in its use, and facilitate better interpretation of submitted evidence [3]. The framework is designed to be risk-informed, meaning the level of rigor required in credibility assessment should be appropriate to the context of use and the role the simulation plays in the regulatory decision-making process.
The American Society of Mechanical Engineers (ASME) has complemented this regulatory framework with the VV 40 - 2018 standard, which provides detailed technical requirements for verification and validation processes specifically applied to medical devices [4]. This standard establishes methodologies for demonstrating that computational models are solved correctly (verification) and that they accurately represent reality (validation).
Core Credibility Challenges in Legacy Environments
Several significant challenges emerge when implementing credibility standards within legacy computational environments:
- Unknown or low credibility of existing models: Many established models have never been rigorously evaluated or suffer from known deficiencies that limit model credibility [5]
- Insufficient data: Quality experimental or clinical data for model development and validation, especially human physiological data under in vivo conditions, is often scarce in legacy environments [5]
- Insufficient analytic methods: Legacy systems often lack modern methods for code verification, appropriate validation metrics, and evaluation of virtual cohort acceptability [5]
- Knowledge and documentation gaps: Original system documentation may be incomplete or missing entirely, complicating credibility assessment [75]
- Technical integration barriers: Legacy systems frequently use outdated data formats or proprietary standards that create compatibility issues with modern credibility assessment tools [75]
These challenges necessitate a strategic approach to integration that balances regulatory requirements with practical technical constraints.
Legacy System Integration Approaches
Integration Architecture Strategies
Connecting legacy computational systems with modern credibility assessment frameworks typically employs three primary architectural approaches:
Table 1: Legacy System Integration Approaches for Credibility Practices
| Integration Approach | Technical Implementation | Advantages for Credibility Workflows | Implementation Considerations |
|---|---|---|---|
| Service Layers | Adds transformation layer atop legacy system to convert data formats between old and new systems [76] | Maintains legacy system integrity while enabling modern data consumption | Can introduce latency; requires understanding of legacy data structures |
| Data Access Layers (DAL) | Implements new database architecture that replicates legacy data in modern format [76] | Enables complex credibility analyses without legacy system constraints | Requires significant data migration; potential data synchronization issues |
| APIs (Application Programming Interfaces) | Creates standardized interfaces that make legacy system functions available to modern services [76] | Provides flexibility for future integrations; supports incremental adoption of credibility practices | Development complexity; requires comprehensive security testing |
The API-based approach has gained particular traction for credibility workflow integration due to its flexibility and compatibility with modern computational assessment tools. Advanced solutions can connect seamlessly with existing systems through cloud-based architectures and APIs, acting as an enhancement layer rather than requiring full system replacement [77].
Layered Monitoring for Progressive Integration
A particularly effective integration strategy for credibility assessment is layered monitoring, which adds a detection or assessment layer over existing systems. This approach allows institutions to progressively enhance their credibility assessment capabilities without disrupting day-to-day operations [77]. For computational modeling workflows, this might involve implementing a validation layer that operates alongside legacy modeling systems, gradually assuming more responsibility as confidence in the new processes grows.
The incremental nature of this approach makes it especially valuable for research organizations with established computational workflows. It allows for gradual adoption of credibility standards without requiring immediate, wholesale changes to legacy systems that may contain critical business logic or historical data [76].
Workflow Optimization for Credibility Compliance
Strategic Workflow Enhancement
Successfully integrating credibility practices requires deliberate optimization of existing computational workflows. This involves analyzing and refining workflows to ensure they efficiently incorporate credibility assessment steps without creating unnecessary bottlenecks [78]. Effective optimization follows several key practices:
- Engage stakeholders from multiple departments (IT, modeling teams, regulatory affairs) to gather insights throughout the project lifecycle [78]
- Set clear objectives for what the integration should accomplish, whether reducing bottlenecks, eliminating redundancy, or making processes more user-friendly [78]
- Define Key Performance Indicators (KPIs) to measure integration success, such as task completion time, error rates, or model validation throughput [78]
- Eliminate unnecessary steps in existing workflows before adding new credibility assessment requirements [78]
- Standardize processes to ensure consistent application of credibility standards regardless of who executes the task [78]
Continuous Monitoring and Improvement
Workflow optimization for credibility compliance is not a one-time event but an ongoing process. Continuous assessment means regularly checking compliance status and building assessment into regular operations [79]. This is particularly important for computational modeling, where model credibility must be maintained as underlying systems evolve.
Implementation should include risk-based assessment scheduling, where high-risk model components receive more frequent review than lower-risk elements [79]. Automated controls testing and real-time policy compliance checks can provide constant feedback without adding manual work to research teams.
Diagram 1: Computational Model Credibility Workflow Integration
Experimental Protocols for Credibility Assessment
Verification and Validation Methodologies
Rigorous experimental protocols form the foundation of computational model credibility assessment. The FDA-endorsed framework emphasizes two complementary processes:
Verification addresses whether the computational model is solved correctly by answering the question: "Is the model solving the equations correctly?" This involves:
- Code verification: Assessing whether the mathematical model and its solution are correctly implemented in the computational code
- Calculation verification: Evaluating the numerical accuracy of the solution to the computational model
Validation determines how well the computational model represents reality by answering: "Is the right model being solved?" This process involves:
- Establishing model accuracy by comparing computational results with experimental data
- Quantifying uncertainty in both computational and experimental results
- Assessing predictive capability for the model's intended context of use
The VV 40 - 2018 standard provides detailed methodologies for applying these processes specifically to medical devices, including techniques for validation experiments, uncertainty quantification, and credibility metric establishment [4].
Many-Analyst Study Approaches
Recent methodological advances in credibility assessment include many-analyst studies, where multiple research teams analyze the same research question using the same data. This approach helps quantify modeling uncertainty by abstracting from sampling error and identifying variation beyond that source [80]. When properly designed, these studies leverage the "wisdom of the crowd" to define appropriate data preparation and identification strategies, overcoming limitations of single reanalyses that may suffer from cherry-picked results [80].
However, these studies must address three critical issues to provide valid credibility assessments:
- Clearly define meta-estimands to separate problematic uncertainty from substantively meaningful variation
- Ensure external validity through incentive structures similar to standard research
- Maintain internal validity through appropriate meta-analytic tools [80]
Table 2: Key Credibility Assessment Metrics and Experimental Data
| Credibility Dimension | Experimental Protocol | Acceptance Threshold | Implementation Challenge in Legacy Systems |
|---|---|---|---|
| Code Verification | Comparison with analytical solutions or method of manufactured solutions [4] | Numerical error < 1% of output range | Limited access to source code; outdated compiler compatibility |
| Model Validation | Comparison with physical experiments across validation domain [4] | Prediction error within experimental uncertainty | Legacy data format incompatibility; insufficient experimental data |
| Uncertainty Quantification | Sensitivity analysis; statistical uncertainty propagation [5] | All significant uncertainties identified and quantified | Computational intensity exceeds legacy system capabilities |
| Predictive Capability | Assessment against independent data sets not used in calibration [5] | Consistent accuracy across context of use | Data access limitations; security restrictions in legacy environments |
Research Reagent Solutions for Credibility Integration
Implementing credibility practices in legacy environments requires both technical tools and methodological approaches. The following essential resources facilitate effective integration:
Table 3: Research Reagent Solutions for Credibility Integration
| Tool Category | Specific Solutions | Function in Credibility Integration | Compatibility Considerations |
|---|---|---|---|
| Integration Platforms | Integration Platform-as-a-Service (IPaaS); Custom APIs [76] | Connect legacy systems with modern credibility assessment tools | Support for legacy protocols; authentication with legacy security |
| Message Queuing Systems | IBM MQ, TIBCO EMS, RabbitMQ [75] | Facilitate reliable communication between legacy and modern systems | Compatibility with legacy message formats; transaction support |
| Data Transformation Tools | Custom service layers; Data access layers [76] | Convert legacy data formats to modern standards for credibility assessment | Handling of proprietary data formats; performance optimization |
| Verification & Validation Tools | ASME VV 40-compliant assessment tools [4] | Standardized credibility assessment following regulatory frameworks | Computational requirements; interface with legacy simulation codes |
| Workflow Automation | Workflow automation software [78] | Streamline credibility assessment processes and reduce manual intervention | Integration with legacy scheduling systems; user permission mapping |
These tools collectively enable research organizations to bridge the gap between legacy computational environments and modern credibility requirements. The layered approach to integration allows institutions to select tools that address their specific credibility gaps without requiring complete system overhaul [77].
Comparative Analysis of Integration Performance
Quantitative Integration Metrics
Different integration approaches yield varying performance characteristics when implementing credibility assessment workflows. The following experimental data illustrates these differences:
Table 4: Performance Comparison of Credibility Integration Approaches
| Integration Method | Implementation Timeline | Error Rate Reduction | Computational Overhead | Model Credibility Improvement |
|---|---|---|---|---|
| API-Based Integration | 3-6 months (typical) [76] | 25-40% reduction in manual data transfer errors [78] | 5-15% performance impact | High (enables comprehensive verification) |
| Service Layer Approach | 2-4 months [76] | 15-30% error reduction [78] | 10-20% performance impact | Medium (enables key validation steps) |
| Layered Monitoring | 3 weeks (proof-of-concept) to 3 months (full) [77] | 30-50% reduction in false positives [77] | <5% performance impact | Progressive (incremental improvement) |
| Full System Modernization | 12-24 months [76] | 40-60% error reduction | Minimal (after migration) | Maximum (complete standards compliance) |
Experimental data from financial institutions with complex legacy infrastructure demonstrates that API-based integration can achieve proof-of-concept implementation in as little as three days, with full deployment within three weeks [77]. This represents a significant acceleration compared to traditional integration timelines of twelve months or more.
Operational Efficiency Outcomes
Integration of credibility practices typically yields substantial operational improvements despite initial implementation challenges:
- Task completion time for model credibility assessment can decrease by 30-60% through workflow automation [78]
- Model validation throughput increases by 40-70% with standardized credibility workflows [78]
- False positive rates in model quality assessment can be reduced by 30-50% through AI-enhanced layered monitoring [77]
- Compliance assessment costs decrease by 25-45% through centralized compliance management and automated monitoring [79]
These metrics demonstrate that despite the challenges of integrating credibility practices with legacy systems, the operational benefits justify the implementation effort. The scalable workflow design ensures that these benefits increase as organizational needs grow [79].
Integrating credibility practices with legacy systems and workflows represents a significant but manageable challenge for research organizations. The regulatory framework provided by the FDA, coupled with technical standards like ASME VV 40, establishes clear requirements for computational model credibility [3] [4]. Multiple integration approaches—from API-based connectivity to layered monitoring—provide viable pathways to implementation without requiring complete system modernization [76] [77].
The experimental data demonstrates that progressive integration strategies yield substantial improvements in model credibility assessment efficiency and effectiveness while minimizing disruption to established research workflows. By adopting a strategic approach that combines appropriate integration technologies with optimized workflows, research organizations can successfully bridge the gap between legacy computational environments and modern credibility requirements, ultimately enhancing both regulatory compliance and research quality.
Managing Data Privacy and Ethical Concerns in Model Development
In computational model development, particularly for high-stakes applications in healthcare and drug development, establishing model credibility is intrinsically linked to addressing data privacy and ethical concerns. The power of computational modeling and simulation (M&S) is realized when results are credible, and the workflow generates evidence that supports credibility for the specific context of use [81]. As regulatory frameworks evolve globally, researchers and drug development professionals must navigate an increasingly complex landscape where technical validation intersects with stringent data protection requirements and ethical imperatives.
The transformative potential of artificial intelligence (AI) in medical product development is substantial, with the FDA noting its exponential increase in regulatory submissions since 2016 [73]. However, this potential depends on appropriate safeguards. A key aspect is ensuring model credibility—defined as trust in the performance of an AI model for a particular context of use [73]. This article examines the frameworks, standards, and methodologies that guide credible practice while addressing the critical data privacy and ethical dimensions that underpin responsible model development.
Comparative Analysis of Credibility and Privacy Frameworks
Established Credibility Frameworks
Several structured frameworks have emerged to establish standards for credible model development and deployment across healthcare and biomedical research:
Table 1: Key Frameworks for Model Credibility and Ethical AI
| Framework/Standard | Primary Focus | Risk-Based Approach | Key Credibility Components | Privacy & Ethics Integration |
|---|---|---|---|---|
| ASME V&V 40 [7] | Computational model credibility for medical devices | Yes | Verification, Validation, Uncertainty Quantification | Foundation for FDA review, indirectly addresses ethics via credibility |
| Ten Rules for Credible M&S in Healthcare [81] | Healthcare modeling & simulation | Not explicitly graded | Comprehensive rubric covering model development, evaluation, and application | Embedded ethical considerations throughout assessment criteria |
| FDA AI Guidance [73] | AI in drug & biological products | Yes | Context of use definition, credibility assessment | Explicit focus on ethical AI with robust scientific standards |
| EU AI Act [82] | AI systems governance | Yes (prohibited, high-risk categories) | Transparency, bias detection, human oversight | Comprehensive privacy and fundamental rights protection |
Quantitative AI Performance Benchmarks
Understanding current AI capabilities contextualizes the importance of robust governance. The 2025 AI Index Report reveals remarkable progress alongside persistent challenges in critical reasoning areas [83]:
Table 2: AI Performance Benchmarks Relevant to Drug Development (2024-2025)
| Benchmark Category | Benchmark Name | 2023 Performance | 2024 Performance | Significance for Drug Development |
|---|---|---|---|---|
| Scientific Reasoning | GPQA | Baseline | +48.9 percentage points | Potential for scientific discovery acceleration |
| Coding Capability | SWE-bench | 4.4% problems solved | 71.7% problems solved | Automated research pipeline development |
| Complex Reasoning | FrontierMath | ~2% problems solved | ~2% problems solved | Limits in novel molecular design applications |
| Model Efficiency | MMLU (60% threshold) | 540B parameters (2022) | 3.8B parameters | Democratization of research tools; 142x parameter reduction |
The performance convergence between open-weight and closed-weight models (gap narrowed from 8.04% to 1.70% within a year) demonstrates rapidly increasing accessibility of high-quality AI systems [83]. However, complex reasoning remains a significant challenge, with systems still unable to reliably solve problems requiring logical reasoning beyond their training data [83]. This has direct implications for trustworthiness and suitability in high-risk drug development applications.
Experimental Protocols for Credibility Assessment
Risk-Based Credibility Assessment (ASME V&V 40 Framework)
The ASME V&V 40 standard provides a risk-informed framework for establishing credibility requirements for computational models, particularly in medical device applications [7]. The methodology follows a structured protocol:
Define Context of Use (COU): Clearly specify how the model will be used to address a specific question, including all relevant assumptions and operating conditions [7] [73].
Assess Model Risk: Evaluate the model's risk based on the COU, considering the decision context and the consequences of an incorrect model prediction [7].
Identify Credibility Factors: Determine which quality measures (validation, verification, etc.) are most critical for the specific COU [7].
Set Credibility Goals: Establish specific acceptability criteria for each credibility factor based on the risk assessment [7].
Execute Credibility Activities: Perform verification, validation, and uncertainty quantification activities to meet the established goals [7].
Evaluate Credibility: Assess whether the completed activities sufficiently demonstrate credibility for the COU [7].
The ASME VVUQ 40.1 technical report provides a practical example applying this framework to a tibial tray component for fatigue testing, demonstrating the complete planning and execution of credibility activities [7].
Ten Rules Rubric Assessment Methodology
The "Ten Rules for Credible Practice of Modeling & Simulation in Healthcare" provides a complementary framework with a pragmatic rubric for assessing conformance [81]. The assessment methodology employs:
Ordinal Scaling: Each rule is evaluated on a scale from Insufficient (0) to Comprehensive (4), providing uniform comparison across reviewers and studies [81].
Multi-dimensional Assessment: The rubric evaluates model purpose, scope, design, implementation, evaluation, and application [81].
Contextual Application: Assessment is tailored to the specific modeling context and intended use [81].
Evidence Documentation: Requires systematic documentation of evidence supporting each credibility determination [81].
The framework has been empirically validated through application to diverse computational modeling activities, including COVID-19 propagation models and hepatic glycogenolysis models with neural innervation and calcium signaling [81].
Data Privacy Integration in Model Development
Regulatory Landscape for AI and Privacy
The global regulatory environment for data privacy as it relates to AI has undergone profound transformation, creating both challenges and opportunities for drug development researchers:
EU AI Act: Imposes a risk-based framework with strict requirements for high-risk AI systems, including transparency, bias detection, and human oversight [82]. Prohibited AI practices and AI literacy requirements became enforceable in February 2025 [84].
US Regulatory Patchwork: Multiple state-level privacy laws (CCPA, TDPSA, FDBR, OCPA) create a complex compliance landscape without comprehensive federal legislation [85] [82].
APAC Variations: India's DPDPA imposes robust consent requirements, China's PIPL enforces strict data localization, while Singapore's Model AI Governance Framework focuses on ethical AI practices [82].
Privacy-Enhancing Technologies (PETs) for Model Development
Privacy-Enhancing Technologies (PETs) enable researchers to access, share, and analyze sensitive data without exposing personal information, addressing both compliance and ethical concerns [86]. Key PETs for computational modeling include:
Table 3: Privacy-Enhancing Technologies for Medical Research
| Technology | Mechanism | Research Application | Limitations |
|---|---|---|---|
| Federated Learning | Model training across decentralized data without data sharing | Multi-institutional model development without transferring patient data | Computational overhead, communication bottlenecks |
| Differential Privacy | Mathematical framework limiting influence of any single record | Publishing aggregate research findings with privacy guarantees | Trade-off between privacy guarantee and data utility |
| Homomorphic Encryption | Computation on encrypted data without decryption | Secure analysis of sensitive genomic and health data | Significant computational requirements, implementation complexity |
| Secure Multi-Party Computation | Joint computation with inputs remaining private | Collaborative analysis across competitive research institutions | Communication complexity, specialized expertise required |
Research indicates that appropriate PET implementation can mitigate the negative impacts of strict data protection regulations on biopharmaceutical R&D, which has been shown to decline by approximately 39% four years after implementation of regulations like GDPR [86].
Essential Research Reagent Solutions
Credibility and Privacy Toolkits
Table 4: Essential Research Reagents for Credible, Privacy-Preserving Model Development
| Reagent Category | Specific Tools/Frameworks | Function | Application Context |
|---|---|---|---|
| Model Credibility Assessment | ASME V&V 40 Framework, Ten Rules Rubric [7] [81] | Structured approach to establish model trustworthiness | Regulatory submissions, high-consequence modeling |
| Privacy-Enhancing Technologies | Differential Privacy, Federated Learning, Homomorphic Encryption [86] | Enable analysis without exposing raw data | Multi-site studies, sensitive health data analysis |
| Regulatory Compliance | ISO/IEC 42001, NIST AI RMF, GDPR/CCPA compliance tools [82] | Ensure adherence to evolving regulatory requirements | Global research collaborations, regulatory submissions |
| Benchmarking & Validation | MMMU, GPQA, SWE-bench, specialized domain benchmarks [83] | Standardized performance assessment | Model selection, capability evaluation, progress tracking |
Implementation Workflow: Integrating Credibility and Privacy
Successful implementation requires systematic integration of credibility and privacy considerations throughout the model development lifecycle:
This integrated workflow emphasizes several critical principles:
Privacy by Design: Incorporating privacy considerations into every development stage, not as an afterthought [87] [84].
Context-Driven Credibility Activities: The level of validation and verification should match the model risk and context of use [7] [73].
Continuous Monitoring: Both model performance and privacy compliance require ongoing assessment post-deployment [87] [85].
Comprehensive Documentation: Maintaining detailed records of both credibility activities and privacy protections for regulatory review [73] [81].
The evolving landscape of computational model development demands rigorous attention to both technical credibility and ethical implementation. As AI systems become more capable—with open-weight models nearly matching closed-weight performance and demonstrating remarkable gains on challenging benchmarks [83]—the frameworks governing their development must similarly advance.
The most successful research organizations will be those that treat privacy and ethics not as compliance obstacles but as fundamental components of model credibility. By integrating standards like ASME V&V 40 [7] with emerging AI governance frameworks [73] [82] and implementing appropriate PETs [86], researchers can advance drug development while maintaining the trust of patients, regulators, and the public.
The future of computational modeling in healthcare depends on this balanced approach—where technical excellence and ethical responsibility progress together, enabling innovation that is both powerful and trustworthy.
Assessing and Comparing Credibility Across Modeling Paradigms and Domains
Computational models have become indispensable tools in fields ranging from medical device development to systems biology. The predictive power of these models directly influences high-stakes decisions in drug development, regulatory approvals, and therapeutic interventions. However, this reliance creates an fundamental requirement: establishing model credibility. Without standardized methods to assess and communicate credibility, researchers cannot confidently reuse, integrate, or trust computational results. This comparison guide examines two distinct but complementary approaches to this challenge: the ASME V&V 40 standard, which provides a risk-informed credibility assessment framework, and technical interoperability standards like SBML (Systems Biology Markup Language) and CellML, which enable reproducibility and reuse through standardized model encoding [88] [89] [90].
The broader thesis of credibility research recognizes that trust in computational models is built through a multi-stage process. Research indicates the workflow progresses from reproducibility (the ability to recreate model results), to credibility (confidence in model predictions), to reusability (adapting models to new contexts), and finally to integration (combining models into more complex systems) [88]. The standards examined here address different stages of this workflow. ASME V&V 40 focuses primarily on establishing credibility through verification and validation activities, while SBML and CellML provide the foundation for reproducibility and reusability that enables credible integration of model components.
ASME V&V 40: A Risk-Informed Credibility Assessment Framework
The ASME V&V 40-2018 standard, titled "Assessing Credibility of Computational Modeling through Verification and Validation: Application to Medical Devices," provides a structured framework for evaluating computational models, with particular emphasis on medical device applications [4]. This standard has gained recognition from regulatory bodies like the U.S. Food and Drug Administration (FDA), making it particularly relevant for submissions requiring regulatory approval [13].
The core philosophy of V&V 40 is risk-informed credibility assessment. The standard does not prescribe specific technical methods but instead provides a process for determining the necessary level of confidence in a model based on the Context of Use (COU) and the risk associated with the decision the model informs [13] [21]. A model's COU explicitly defines how the model predictions will be used to inform specific decisions. The credibility requirements are then scaled to match the model risk—higher-risk applications require more extensive verification, validation, and uncertainty quantification (VVUQ) activities [13].
SBML and CellML: Interoperability Standards for Reproducibility and Reuse
SBML (Systems Biology Markup Language) is a free, open, XML-based format for representing computational models of biological processes [89] [91]. Its primary purpose is to enable model exchange between different software tools, facilitate model sharing and publication, and ensure model survival beyond the lifetime of specific software platforms [91]. SBML can represent various biological phenomena, including metabolic networks, cell signaling pathways, regulatory networks, and infectious disease models [91].
CellML is similarly an open, XML-based language but is specifically focused on describing and exchanging models of cellular and subcellular processes [92] [90]. A key feature of CellML is its use of MathML to define the underlying mathematics of models and its component-based architecture that supports model reuse and increasing complexity through model importation [90].
The core philosophy of both SBML and CellML centers on enabling reproducibility, reuse, and integration through standardized machine-readable model representation. These standards focus on the technical encoding of models to facilitate sharing and interoperability across the research community [89] [92] [90].
Table 1: Fundamental Characteristics of the Standards
| Characteristic | ASME V&V 40 | SBML | CellML |
|---|---|---|---|
| Primary Focus | Credibility assessment process | Model representation and exchange | Model representation and exchange |
| Domain Origin | Engineering/Medical Devices | Systems Biology | Cellular Physiology |
| Core Philosophy | Risk-informed confidence evaluation | Interoperability and sharability | Component reuse and mathematical clarity |
| Technical Basis | Process framework | XML-based language with modular packages | XML-based language with MathML mathematics |
| Regulatory Recognition | FDA-recognized standard [13] | Community adoption in bioinformatics | Community adoption in cellular modeling |
Comparative Analysis of Methodologies and Approaches
Credibility Establishment: Process vs. Technical Foundation
ASME V&V 40 and the systems biology standards approach credibility from fundamentally different angles. ASME V&V 40 provides a process framework for determining what evidence is needed to establish credibility for a specific Context of Use [13]. It guides users through identifying relevant model risks, determining necessary credibility evidence, and selecting appropriate VVUQ activities. The framework is flexible and adaptable to various modeling approaches but does not specify technical implementation details.
In contrast, SBML and CellML establish credibility through technical reproducibility and reuse. By providing standardized, unambiguous model descriptions, these languages enable independent researchers to reproduce and verify model implementations [89] [91]. The ability to successfully execute a model across different simulation environments and to reuse model components in new contexts provides foundational credibility evidence. As noted in discussions about multiscale modeling, reproducibility is the essential first step toward credibility, without which researchers cannot confidently build upon existing work [88].
Scope and Applicability
The scope of these standards differs significantly, reflecting their origins in different scientific communities:
ASME V&V 40 is domain-agnostic in principle but has been primarily applied to medical devices, including computational models of heart valves, orthopedic implants, and spinal devices [13]. The standard can be adapted to any computational model where a Context of Use can be defined and model risk assessed.
SBML is specifically designed for biological system models, with capabilities oriented toward representing biochemical reaction networks, signaling pathways, and other biological processes [91]. Its modular Level 3 architecture includes specialized packages for flux balance analysis (fbc), spatial processes (spatial), and qualitative models (qual) [93].
CellML focuses specifically on cellular and subcellular processes, with strong capabilities for representing the underlying mathematics of electrophysiological, metabolic, and signaling models [90]. Its component-based architecture supports building complex cellular models from simpler components.
Table 2: Methodological Comparison for Establishing Model Credibility
| Credibility Aspect | ASME V&V 40 Approach | SBML/CellML Approach |
|---|---|---|
| Reproducibility | Addressed through verification activities (code and calculation verification) | Enabled through standardized, executable model encoding |
| Validation | Explicit process for comparing model predictions to experimental data | Facilitated by enabling model exchange and comparison across tools |
| Uncertainty Quantification | Required activity scaled to model risk | Supported through model annotation and parameter variation |
| Reusability | Indirectly addressed through documentation of credibility evidence | Directly enabled through component-based model architecture |
| Integration | Considered in context of multi-scale models and their specific challenges | Core feature through model composition and submodel referencing |
Implementation Requirements and Workflows
The following diagram illustrates the contrasting workflows for implementing these standards:
Diagram 1: Contrasting Workflows of Credibility Standards
Experimental Protocols and Implementation Case Studies
ASME V&V 40 Implementation in Medical Device Modeling
The application of ASME V&V 40 follows a structured protocol centered on the model's Context of Use (COU). A representative case study involves computational modeling of a transcatheter aortic valve (TAV) for design verification activities [13].
Experimental Protocol:
- Context of Use Definition: The COU is explicitly defined as "structural component stress/strain (metal fatigue) analysis for a TAV device in accordance with ISO5840-1:2021" [13].
- Risk Assessment: The risk associated with model predictions is categorized based on the potential impact of an incorrect prediction on device safety and performance.
- Credibility Plan Development: Specific verification, validation, and uncertainty quantification activities are selected, with rigor commensurate to the assessed risk.
- Verification Activities: Code verification confirms the finite element analysis (FEA) software correctly solves the underlying equations. Calculation verification establishes appropriate mesh density and time-step parameters.
- Validation Activities: Model predictions of component stresses are compared against physical bench testing data from manufactured prototypes using standardized mechanical testing protocols (e.g., ASTM F2077) [13].
- Uncertainty Quantification: Key uncertain parameters (e.g., material properties, contact friction, boundary conditions) are identified and their impact on model predictions quantified.
- Credibility Documentation: Evidence from all activities is compiled to demonstrate the model's predictive capability for its specific COU.
In the TAV case study, researchers demonstrated that varying contact stiffness and friction parameters significantly affected both global force-displacement predictions and local surface strain measurements, highlighting the importance of uncertainty quantification in model credibility [13].
SBML/CellML Implementation in Systems Biology
The implementation of SBML and CellML follows protocols focused on model encoding, sharing, and reuse. A typical experimental protocol for model development and exchange would include:
Model Encoding Protocol:
- Model Conceptualization: Biological processes are represented as a network of entities (species in SBML) and processes (reactions in SBML) or as mathematical equations describing cellular physiology (in CellML).
- Standardized Encoding: The model is encoded using the appropriate SBML Level 3 Core specification or CellML 1.1 specification, potentially incorporating specialized packages for additional functionality [93] [90].
- Annotation: Model elements are annotated with references to external data resources using machine-readable metadata, typically in RDF format.
- Software Implementation: The model is implemented across multiple simulation tools (e.g., COPASI, Virtual Cell, OpenCOR) to verify consistent interpretation.
- Repository Submission: The validated model is submitted to a public repository such as BioModels Database for community access.
- Model Reuse and Composition: Existing models are imported as submodels to create more complex multi-scale systems using the Hierarchical Model Composition package in SBML Level 3 [93].
The hierarchical model composition capability in SBML Level 3 deserves particular emphasis. This feature enables researchers to manage model complexity by decomposing large models into smaller submodels, incorporate multiple instances of a given model within enclosing models, and create libraries of reusable, tested model components [91]. This directly addresses the integration challenges noted in multiscale modeling discussions [88].
Table 3: Essential Research Reagents and Resources
| Resource | Function | Relevance |
|---|---|---|
| libSBML/JSBML | Programming libraries for reading, writing, and manipulating SBML models [89] | Essential for software developers implementing SBML support in applications |
| BioModels Database | Curated repository of published models encoded in SBML [89] | Provides reference models for testing and model components for reuse |
| CellML Model Repository | Public repository of CellML models [92] | Source of reusable cellular model components |
| ASME V&V 40 Standard Document | Definitive specification of the credibility assessment framework [4] | Essential reference for proper implementation of the V&V 40 process |
| Computational Modeling Software | Tools like ANSYS, COMSOL, Simulia for physics-based modeling [13] | Platforms for implementing computational models requiring V&V 40 assessment |
| Systems Biology Software | Tools like COPASI, Virtual Cell, OpenCOR for biological simulation [91] | Platforms supporting SBML/CellML for model simulation and analysis |
Integration Potential and Complementary Applications
While these standards originate from different domains, they exhibit significant integration potential for multi-scale models that span from cellular to organ and system levels. The following diagram illustrates how these standards can be combined in a comprehensive modeling workflow:
Diagram 2: Integration of Standards Across Biological Scales
This integrated approach is particularly valuable for pharmaceutical development and regulatory submissions. For example, a QSP (Quantitative Systems Pharmacology) model might use SBML to encode cellular signaling pathways affected by a drug candidate, while employing ASME V&V 40 principles to establish credibility for predictions of clinical efficacy [94]. The integration of within-host models (encoded in SBML/CellML) with between-host epidemiological models represents another promising application area that could enhance pandemic preparedness [88].
This comparative analysis reveals that ASME V&V 40 and systems biology standards (SBML, CellML) address complementary aspects of computational model credibility. The appropriate selection depends fundamentally on the research context and objectives:
ASME V&V 40 is the strategic choice for researchers developing computational models to support regulatory submissions, particularly for medical devices, or any application where establishing defendable credibility for specific decision-making contexts is paramount [13] [21].
SBML and CellML are essential for research programs focused on biological systems modeling, particularly those emphasizing model sharing, community validation, component reuse, and building upon existing models to accelerate discovery [89] [91] [90].
For organizations addressing complex multi-scale challenges, such as pharmaceutical companies developing integrated pharmacological-to-clinical models or research consortia building virtual physiological human platforms, the combined implementation of these standards offers a comprehensive approach. SBML and CellML provide the technical foundation for reproducible, reusable model components, while ASME V&V 40 offers the process framework for establishing credibility of integrated model predictions for specific contexts of use. This synergistic application represents the most robust approach to computational model credibility for high-impact research and development.
Benchmarking and Credibility Assessment for Patient-Specific Computational Models
The adoption of patient-specific computational models in biomedical research and clinical decision-making is accelerating, spanning applications from medical device design to personalized treatment planning. Trust in these in silico tools, however, hinges on rigorous and standardized assessment of their credibility. This involves demonstrating that a model is both correctly implemented (verification) and that it accurately represents reality (validation), while also quantifying its uncertainties. Frameworks like the American Society of Mechanical Engineers (ASME) V&V 40 standard provide a risk-based methodology for establishing this credibility, defining requirements based on a model's potential influence on decision-making and the consequence of an incorrect result [7] [95]. Concurrently, the rise of data-driven models, including large language models (LLMs) for medical applications, has necessitated the development of new benchmarking approaches to evaluate their performance, safety, and utility. This guide compares the prevailing methodologies for benchmarking and credibility assessment, providing researchers and developers with a structured comparison of approaches, experimental data, and the essential tools needed to navigate this critical field.
Comparative Analysis of Benchmarking and Credibility Frameworks
The landscape of model assessment can be divided into two primary, complementary strands: one focused on traditional physics-based computational models and the other on emerging artificial intelligence (AI) and data-driven models. The table below summarizes the core characteristics of the prominent frameworks and studies in this domain.
Table 1: Comparison of Credibility Assessment and Benchmarking Frameworks
| Framework/Study | Primary Model Type | Core Assessment Methodology | Key Metrics | Application Context |
|---|---|---|---|---|
| ASME V&V 40 Standard [96] [7] [95] | Physics-based Computational Models | Risk-based Verification, Validation, and Uncertainty Quantification (VVUQ) | Model Risk, Credibility Goal, Area Metric, Acceptance Threshold (e.g., 5%) | Medical devices, Patient-specific biomechanics, In silico clinical trials |
| TAVI Model Validation [96] [97] | Patient-Specific Fluid-Structure Interaction | Validation against clinical post-op data using empirical cumulative distribution function (ECDF) | Device Diameter, Effective Orifice Area (EOA), Transmural Pressure Gradient (TPG) | Transcatheter Aortic Valve Implantation (TAVI) planning |
| ATAA Model Credibility [95] | Patient-Specific Finite Element Analysis | Comprehensive VVUQ following ASME V&V 40; Surrogate modeling for UQ | Aneurysm Diameter, Wall Stress; Sensitivity analysis on input parameters | Aneurysmal Thoracic Ascending Aorta (ATAA) biomechanics |
| BioChatter LLM Benchmark [98] | Large Language Models (LLMs) | LLM-as-a-Judge evaluation with clinician-validated ground truths | Comprehensiveness, Correctness, Usefulness, Explainability, Safety | Personalized longevity intervention recommendations |
| LLM Confidence Benchmark [99] | Large Language Models (LLMs) | Correlation analysis between model confidence and accuracy on medical exams | Accuracy, Confidence Score for correct/incorrect answers | Clinical knowledge (multiple-choice questions across specialties) |
The comparative data reveals a fundamental alignment in purpose but a divergence in technique. The ASME V&V 40 framework establishes a principled, risk-informed foundation for physics-based models, where credibility is built upon a chain of evidence from code verification to validation against experimental or clinical data [7] [95]. For instance, in patient-specific modeling of the aorta, a high severity level (e.g., 5) mandates a validation acceptance threshold of ≤5% for the aneurysm diameter when compared to clinical imaging [95]. Similarly, a TAVI model validation demonstrated that device diameter predictions met this rigorous 5% threshold, while hemodynamic parameters like Effective Orifice Area showed slightly greater discrepancies [96].
In contrast, benchmarks for Large Language Models must evaluate different facets of performance. A benchmark for LLMs generating personalized health advice found that while proprietary models like GPT-4o outperformed open-source ones in comprehensiveness, all models exhibited limitations in addressing key medical validation requirements, even with Retrieval-Augmented Generation (RAG) [98]. Furthermore, a critical finding in LLM confidence benchmarking is that lower-performing models often display paradoxically higher confidence in their incorrect answers, highlighting a significant calibration issue for safe clinical deployment [99].
Detailed Experimental Protocols for Credibility Assessment
Protocol 1: Population-Based Validation of a TAVI Model via ASME V&V 40
This protocol details the validation of a patient-specific computational model for Transcatheter Aortic Valve Implantation (TAVI), as exemplified by Scuoppo et al. [96].
- Objective: To validate the structural and hemodynamic predictions of a SAPIEN 3 Ultra device deployment model against quantitative post-TAVI clinical data.
- Context of Use (CoU): Supporting clinical decision-making in TAVI procedural planning by predicting device deployment and post-operative hemodynamics.
- Question of Interest (QoI): How well does the computational model predict the deployed device geometry and post-TAVI blood flow parameters?
- Model Risk: High, as model outputs could influence treatment planning; thus, a high level of rigor is required.
Methodology:
- Model Development: Develop patient-specific finite-element models (n=20) from medical imaging. Simulate S3 device deployment and subsequent hemodynamics using a Fluid-Structure Interaction (FSI) approach.
- Data Extraction: From the simulations, extract scalar values for:
- Structural Parameters: Device diameters at the inflow, mid-flow, and outflow cross-sectional levels.
- Hemodynamic Indices: Effective Orifice Area (EOA) and transmural pressure gradient (TPG).
- Clinical Comparator: Obtain corresponding measurements from post-TAVI computed tomography (CT) imaging (for device diameters) and echocardiographic data (for EOA and TPG).
- Probabilistic Validation Analysis:
- Calculate the Empirical Cumulative Distribution Function (ECDF) for both the in silico predictions and the clinical measurements for each parameter.
- Compute the "area metric" (the area between the ECDF curves) to quantitatively evaluate the agreement.
- Compare the area metric against a pre-defined acceptance threshold of 5% to determine model credibility for each QoI.
Outcomes: The study reported an area metric of ≤5% for device diameters, establishing high credibility for structural predictions. Hemodynamic parameters showed slightly larger discrepancies (EOA: 6.3%, TPG: 9.6%), potentially due to clinical measurement variability [96].
Protocol 2: Benchmarking LLMs for Personalized Health Interventions
This protocol outlines the methodology for benchmarking LLMs in a specialized medical domain, as implemented using the BioChatter framework [98].
- Objective: To benchmark the ability of LLMs to generate personalized, biomarker-based longevity intervention recommendations.
- Context of Use (CoU): Evaluating the potential for LLMs to provide unsupervised medical intervention advice.
- Question of Interest (QoI): How comprehensively, correctly, usefully, explainably, and safely do different LLMs respond to synthetic patient queries?
Methodology:
- Benchmark Dataset:
- Create 25 synthetic medical profiles, reviewed and approved by physicians.
- Profiles are modular, allowing combination to generate 1000 diverse test cases. Variations include age groups and types of interventions (e.g., caloric restriction, fasting).
- Model Inference:
- Test both proprietary (e.g., GPT-4o, GPT-4o mini) and open-source models (e.g., Llama 3.2 3B, Qwen 2.5 14B).
- Run models with system prompts of varying complexity and with/without Retrieval-Augmented Generation (RAG) to provide domain-specific context.
- Evaluation via LLM-as-a-Judge:
- Use a powerful LLM (GPT-4o mini) as an automated judge to evaluate 56,000 model responses.
- The judge model is provided with expert-authored, test-item-specific ground truths.
- Each response is scored on five validation requirements:
- Comprehensiveness (Comprh)
- Correctness (Correct)
- Usefulness (Useful)
- Interpretability/Explainability (Explnb)
- Consideration of Toxicity/Safety (Safe)
- Statistical Analysis: Calculate balanced accuracy for each model and requirement. Perform ablation studies to test vulnerability to prompt variations.
Outcomes: The benchmark found that proprietary models generally outperformed open-source ones, particularly in comprehensiveness. However, no model reliably addressed all validation requirements, indicating limited suitability for unsupervised use. RAG had an inconsistent effect, sometimes helping open-source models but degrading the performance of proprietary ones [98].
Workflow Visualization of Credibility Assessment
The following diagram illustrates the overarching workflow for establishing model credibility, integrating principles from the ASME V&V 40 standard and contemporary benchmarking practices.
The Scientist's Toolkit: Essential Reagents and Materials
Successful credibility assessment and benchmarking require a suite of methodological tools and data resources. The following table catalogs key solutions used in the featured experiments and the broader field.
Table 2: Essential Research Reagent Solutions for Credibility Assessment
| Item Name | Function/Benefit | Example Use Case |
|---|---|---|
| ASME V&V 40 Standard | Provides a risk-based framework for planning and reporting VVUQ activities. | Guiding the credibility assessment for patient-specific models of TAVI [96] and aortic aneurysms [95]. |
| Clinical Imaging Data (CT, CTA) | Serves as the foundation for reconstructing patient-specific anatomy and as a primary comparator for validation. | Segmenting the lumen of an aneurysmal aorta [95]; measuring post-TAVI device dimensions [96]. |
| Finite Element Analysis Software | Solves complex biomechanical problems by simulating physical phenomena like stress and fluid flow. | Simulating stent deployment in TAVI [96] and wall stress in aortic aneurysms [95]. |
| Synthetic Test Profiles | Enables controlled, scalable, and reproducible benchmarking without using real patient data, mitigating privacy concerns. | Generating 25 synthetic medical profiles to test LLMs on longevity advice [98]. |
| Retrieval-Augmented Generation | Grounds LLM responses in external, verified knowledge sources to reduce hallucinations and improve accuracy. | Augmenting LLM prompts with domain-specific context in longevity medicine benchmarks [98]. |
| LLM-as-a-Judge Paradigm | Enables automated, high-throughput evaluation of a large number of free-text model responses against expert ground truths. | Evaluating 56,000 LLM responses across five validation requirements [98]. |
| Empirical CDF (ECDF) & Area Metric | Provides a probabilistic method for comparing the entire distribution of model predictions against clinical data, going beyond single-value comparisons. | Quantifying the agreement between simulated and clinical TAVI parameters across a patient cohort [96]. |
| Uncertainty Quantification (UQ) & Sensitivity Analysis | Identifies and quantifies how uncertainties in model inputs (e.g., material properties) propagate to uncertainties in outputs. | Determining that aneurysm wall thickness is the most sensitive parameter in an ATAA model [95]. |
The rigorous benchmarking and credibility assessment of patient-specific computational models are non-negotiable prerequisites for their confident application in research and clinical settings. The ASME V&V 40 standard offers a robust, generalizable framework for physics-based models, emphasizing a risk-based approach to VVUQ. In parallel, emerging benchmarks for AI and LLMs are developing sophisticated metrics to evaluate not just accuracy, but also comprehensiveness, safety, and explainability. The experimental data consistently shows that while modern models are powerful, they have distinct limitations—whether in predicting certain hemodynamic parameters or in calibrating confidence for medical advice. A thorough understanding of these frameworks, methodologies, and tools, as detailed in this guide, empowers researchers and developers to build more credible models and paves the way for their responsible integration into healthcare.
The Role of Historical Evidence and Model Reuse in Credibility Building
In the high-stakes domains of drug development and medical device regulation, computational models are indispensable for accelerating innovation and ensuring patient safety. The credibility of these models is not established in a vacuum; it is built upon a foundation of historical evidence and the strategic reuse of established models. This practice is central to modern regulatory frameworks and international standards, which provide a structured approach for assessing whether a model is fit for its intended purpose. The Model-Informed Drug Development (MIDD) framework, for instance, relies on this principle, using a "fit-for-purpose" strategy where the selection of modeling tools is closely aligned with specific questions of interest and contexts of use throughout the drug development lifecycle [12].
Similarly, regulatory guidance from the FDA and standards from organizations like ASME (VV-40) formalize this approach, offering a risk-informed framework for credibility assessment. These guidelines emphasize that the evidence required to justify a model's use is proportional to the model's influence on regulatory and business decisions [3] [4]. This article explores the critical role of historical evidence and model reuse within these established paradigms, providing a comparative analysis of methodologies and the experimental protocols that underpin credible computational modeling.
Foundational Standards for Credibility Assessment
The credibility of computational models is evaluated against rigorous standards that emphasize verification, validation, and the justification of a model's context of use. These standards provide the bedrock for regulatory acceptance.
Regulatory Guidance (FDA): The FDA's guidance document, "Assessing the Credibility of Computational Modeling and Simulation in Medical Device Submissions," outlines a risk-informed framework for evaluating credibility. Its primary goal is to promote consistency and facilitate efficient review, thereby increasing confidence in the use of CM&S in regulatory submissions. The guidance is applicable to physics-based, mechanistic, and other first-principles-based models, and it provides recommendations on the evidence needed to demonstrate that a model is sufficiently credible for its specific regulatory purpose [3].
Technical Standard (ASME V&V 40): The ASME V&V 40 standard offers a more detailed technical framework, establishing terminology and processes for assessing credibility through verification and validation activities. It introduces the crucial concept of a "Context of Use" (COU), defined as the specific role and scope of a model within a decision-making process. The standard stipulates that the level of effort and evidence required for credibility is directly tied to the "Risk associated with the Model Influence" within that COU. This means a model supporting a high-impact decision, such as a primary efficacy endpoint in a clinical trial, demands a more extensive credibility assessment than one used for exploratory analysis [4].
Industry Framework (MIDD): In the pharmaceutical sector, the MIDD framework operates on a similar "fit-for-purpose" philosophy. A model is considered "fit-for-purpose" when it is well-aligned with the "Question of Interest," "Content of Use," and the potential influence and risk of the model in presenting the totality of evidence. Conversely, a model fails to be fit-for-purpose if it lacks a defined COU, suffers from poor data quality, or is inadequately verified or validated. Oversimplification or unjustified complexity can also render a model unsuitable for its intended task [12].
Table 1: Core Concepts in Model Credibility Frameworks
| Concept | FDA Guidance [3] | ASME V&V 40 Standard [4] | MIDD Framework [12] |
|---|---|---|---|
| Primary Focus | Regulatory consistency and efficient review for medical devices | Technical methodology for verification & validation (V&V) | Optimizing drug development and regulatory decision-making |
| Key Principle | Risk-informed credibility assessment | Credibility based on Context of Use (COU) and Model Influence Risk | "Fit-for-Purpose" (FFP) model selection and application |
| Role of Evidence | Evidence proportional to model's role in submission | Evidence from V&V activities to support specific COU | Historical data and model outputs to support development decisions |
| Model Reuse Implication | Promotes reusable or dynamic model frameworks | Establishes baseline credibility for models in new, similar COUs | Enables reuse of QSAR, PBPK, etc., across development stages |
The Role of Historical Evidence and Model Reuse
Historical evidence and model reuse are powerful tools for enhancing scientific rigor, improving efficiency, and building a compelling case for a model's credibility. This practice aligns directly with the "fit-for-purpose" and risk-informed principles enshrined in regulatory standards.
Leveraging Historical Evidence
Historical evidence provides a benchmark for model performance and a foundation of prior knowledge. In drug development, Model-Informed Drug Development (MIDD) increases the success rates of new drug approvals by offering a structured, data-driven framework for evaluating safety and efficacy. This approach uses quantitative predictions to accelerate hypothesis testing and reduce costly late-stage failures, relying heavily on historical data and models [12]. The credibility of this historical evidence itself is paramount. As noted in analyses of clinical data, high-quality data must be complete, granular, traceable, timely, consistent, and contextually rich to be reliable for decision-making [100].
Strategies for Model Reuse
Model reuse avoids redundant work and leverages established, validated work. The following strategies are prevalent in the industry:
- Reusable/Dynamic Models: The FDA's "fit-for-purpose" initiative explicitly includes a regulatory pathway for "reusable" or "dynamic" models. Successful applications have included dose-finding and modeling patient drop-out across multiple disease areas, demonstrating how a single validated model framework can be adapted for new but related contexts [12].
- Foundational Model Types in MIDD: Certain computational methodologies are routinely reused across the drug development lifecycle. For example:
- Quantitative Structure-Activity Relationship (QSAR): Used early in discovery to predict compound activity [12].
- Physiologically Based Pharmacokinetic (PBPK) Modeling: Provides a mechanistic understanding of drug disposition [12].
- Population PK (PPK) and Exposure-Response (ER) Models: Critical in clinical stages to understand variability and efficacy [12].
- Model-Based Meta-Analysis (MBMA): This technique integrates historical evidence from multiple clinical trials to inform the design of new studies and development programs, providing a quantitative basis for forecasting outcomes [12].
Diagram 1: This workflow illustrates how a model, once developed and validated for a specific Context of Use (COU), creates a dossier of historical evidence. This evidence facilitates reuse for new, similar COUs, reducing the verification and validation (V&V) burden and creating a virtuous cycle of enhanced credibility.
Comparative Analysis of Model Reuse Applications
The application and benefits of model reuse vary across different stages of product development and types of models.
Table 2: Comparative Analysis of Model Reuse in Different Contexts
| Application Area | Primary Model Types | Role of Historical Evidence | Impact on Credibility Building |
|---|---|---|---|
| Drug Development (MIDD) [12] | PBPK, PPK/ER, QSP | Prior knowledge integrated via Bayesian methods; data from earlier trials. | Shortens development timelines, reduces cost, increases success rates of new drug approvals. |
| Medical Device Regulation [3] | Physics-based, Mechanistic | Evidence from prior validation studies for similar device physics or anatomy. | Promotes regulatory consistency; facilitates efficient review of submissions. |
| AI Model Evaluation [101] | Large Language Models (LLMs) | Performance on standardized benchmarks (e.g., MMLU, GAIA, WebArena). | Enables objective comparison of capabilities; tracks progress over time; identifies failure modes. |
Experimental Protocols for Credibility Assessment
A standardized protocol is essential for generating the evidence required to build credibility. The following methodology, synthesized from regulatory and standards documents, outlines key steps for evaluating a computational model, particularly when historical evidence is a factor.
Protocol for a Credibility Assessment Experiment
Objective: To determine if a computational model is credible for a specified Context of Use (COU) by assessing its predictive accuracy against historical or new experimental data.
Materials and Reagents:
- Computational Model: The software and mathematical formulation to be evaluated.
- Validation Dataset: A high-quality dataset, independent from the model's training/development data, serving as the ground truth [100].
- Verification Tools: Software and scripts to confirm the model solves equations correctly (e.g., code verification, mesh convergence tests).
- Uncertainty Quantification Framework: Methods to characterize numerical, parametric, and model-form uncertainties.
- Reference Standards: Relevant regulatory guidelines (e.g., FDA, ICH M15) and technical standards (e.g., ASME VV 40) [12] [3].
Experimental Workflow:
- Define Context of Use (COU): Precisely specify the question the model will answer, the inputs it will use, and the outputs it will produce to inform a decision. This is the foundational step per ASME VV 40 and MIDD guidance [12] [4].
- Conduct Model Verification: Ensure the computational model is implemented correctly and without numerical errors. This involves checking code and solving equations accurately.
- Perform Model Validation: Execute a structured comparison of model predictions against the validation dataset. This is the core experimental step.
- Select validation points that critically challenge the model within its COU.
- Run the model for the conditions of the validation data.
- Quantify the disagreement between predictions and data using pre-defined validation metrics (e.g., mean squared error, confidence interval coverage).
- Assess Validation Evidence: Compare the observed validation results against pre-defined acceptability criteria (e.g., all predictions within a 2-fold margin of experimental data). These criteria should be justified based on the COU and the Risk associated with the Model Influence [4].
- Document and Report: Compile a comprehensive dossier including the COU definition, verification and validation results, uncertainty analysis, and a clear statement on the model's credibility for its intended use [3].
Diagram 2: This workflow outlines the key experimental steps for assessing model credibility, from defining the Context of Use to the final documentation of evidence. The process is gated by pre-defined acceptability criteria.
Key Research Reagents and Materials
The following tools and resources are essential for conducting a rigorous credibility assessment.
Table 3: Essential Research Reagents and Solutions for Credibility Experiments
| Reagent / Resource | Function in Credibility Assessment | Critical Parameters |
|---|---|---|
| High-Quality Validation Dataset [100] | Serves as the objective ground truth for evaluating model predictive accuracy. | Completeness, Granularity, Traceability, Timeliness, Consistency, Contextual Richness. |
| Model Verification Suite | Checks for correct numerical implementation of the computational model. | Code coverage, convergence tolerance, unit test pass/fail rates. |
| Uncertainty Quantification (UQ) Tools | Characterizes the confidence and reliability of model predictions. | Parameter distributions, numerical error estimates, model form uncertainty. |
| Credibility Assessment Framework [3] [4] | Provides the structured methodology and acceptance criteria for the evaluation. | Defined Context of Use, Risk Level, Pre-defined acceptability criteria. |
The path to credible computational models in regulated industries is systematic and evidence-driven. Frameworks like the FDA's risk-informed guidance, ASME's V&V 40, and the "fit-for-purpose" principles of MIDD collectively establish that historical evidence and strategic model reuse are central to credible and efficient modeling. By leveraging existing models and their associated evidence dossiers for new, similar contexts of use, organizations can significantly reduce the burden of verification and validation while strengthening the regulatory case for their simulations. This practice creates a virtuous cycle: each successful application of a model enriches its historical evidence base, making subsequent reuse more justifiable and the model itself more deeply credentialed. As computational modeling continues to expand its role in product development, a mastery of these principles will be indispensable for researchers, scientists, and developers aiming to bring safe and effective innovations to market.
The ASME VVUQ 40.1 technical report represents a significant advancement in the standardization of computational model credibility. Titled "An Example of Assessing Model Credibility Using the ASME V&V 40 Risk-Based Framework: Tibial Tray Component Worst-Case Size Identification for Fatigue Testing," this document provides a critical practical illustration of the risk-based credibility framework established in the parent ASME V&V 40-2018 standard [102] [7]. For researchers and drug development professionals, this technical report offers an exhaustive, end-to-end exemplar that moves beyond theoretical guidance to demonstrate concrete verification and validation activities tailored to a specific Context of Use (COU) [7].
This emerging technical report arrives at a pivotal moment, as regulatory agencies increasingly accept computational modeling and simulation (CM&S) as substantial evidence in submissions. The U.S. Food and Drug Administration (FDA) has incorporated the risk-based framework from V&V 40 into its evaluation of computational models for both medical devices and, more recently, drug and biological products [6] [73] [103]. The draft FDA guidance on artificial intelligence explicitly endorses a nearly identical risk-based approach to establishing model credibility, highlighting the regulatory convergence around these principles [73] [103]. Within this context, VVUQ 40.1 serves as an essential template for constructing comprehensive model credibility packages that can withstand rigorous regulatory scrutiny.
Comparative Analysis of VVUQ Standards and Technical Reports
The ASME VVUQ suite comprises multiple standards and technical reports, each targeting different applications and specificity levels. Understanding how VVUQ 40.1 fits within this ecosystem is crucial for proper implementation.
Table 1: Comparison of Key ASME VVUQ Standards and Technical Reports
| Document Name | Document Type | Primary Focus | Status (as of 2025) |
|---|---|---|---|
| V&V 40-2018 | Standard | Assessing Credibility of Computational Modeling through Verification and Validation: Application to Medical Devices [102] | Published |
| VVUQ 40.1 | Technical Report | An Example of Assessing Model Credibility Using the ASME V&V 40 Risk-Based Framework: Tibial Tray Component Worst-Case Size Identification for Fatigue Testing [7] | Expected Q1-Q2 2025 [7] |
| V&V 10-2019 | Standard | Standard for Verification and Validation in Computational Solid Mechanics [102] | Published |
| V&V 20-2009 | Standard | Standard for Verification and Validation in Computational Fluid Dynamics and Heat Transfer [102] | Published |
| VVUQ 60.1-2024 | Guideline | Considerations and Questionnaire for Selecting Computational Physics Simulation Software [102] | Published |
The distinct value of VVUQ 40.1 lies in its detailed, practical application. While the parent V&V 40 standard provides the risk-based framework, it contains only limited examples. VVUQ 40.1 expands this by walking through "the planning and execution of every activity" for a specific fictional tibial tray model [7]. Furthermore, it introduces a forward-looking element by discussing "proposed work that could be done if greater credibility is needed," providing researchers with a continuum of V&V activities [7].
Experimental Protocol and Methodology for Credibility Assessment
The methodology demonstrated in VVUQ 40.1 follows the rigorous, multi-stage risk-informed credibility assessment framework established by V&V 40. This process systematically links the model's intended use to the specific verification and validation activities required to establish sufficient credibility [6].
Risk-Based Credibility Assessment Workflow
The following diagram illustrates the comprehensive workflow for applying the risk-based credibility assessment framework as exemplified in VVUQ 40.1:
Core Methodology and Key Definitions
The experimental protocol for establishing model credibility, as detailed in frameworks like VVUQ 40.1, relies on several foundational concepts and their relationships. The following diagram clarifies these core components and their interactions:
Define Context of Use (COU): The COU is a detailed statement that explicitly defines the specific role, scope, and boundaries of the computational model used to address the question of interest [6]. In the VVUQ 40.1 tibial tray example, the COU involves identifying the worst-case size of a tibial tray component for subsequent physical fatigue testing [7].
Assess Model Risk: Model risk is a composite evaluation of Model Influence (the contribution of the model relative to other evidence in decision-making) and Decision Consequence (the significance of an adverse outcome from an incorrect decision) [6]. This risk assessment directly determines the rigor and extent of required credibility activities [6] [103].
Establish Model Credibility: This phase involves executing specific Verification and Validation activities. Verification answers "Was the model built correctly?" by ensuring the computational model accurately represents the underlying mathematical model [104] [105]. Validation answers "Was the right model built?" by determining the degree to which the model is an accurate representation of the real world from the perspective of the intended uses [6] [105].
The Researcher's Toolkit: Essential Components for Credibility Assessment
Successfully implementing the methodologies in VVUQ 40.1 requires a suite of conceptual tools and reagents. The table below details the key "research reagents" — the core components and techniques — essential for conducting a comprehensive credibility assessment.
Table 2: Essential Research Reagents for Computational Model Credibility Assessment
| Tool/Component | Category | Function in Credibility Assessment |
|---|---|---|
| Credibility Assessment Plan | Documentation | Outlines specific V&V activities, goals, and acceptance criteria commensurate with model risk [6] [103]. |
| Software Quality Assurance | Verification | Provides evidence that the software code is implemented correctly and functions reliably [6]. |
| Systematic Mesh Refinement | Verification | Method for estimating and reducing discretization error through controlled grid convergence studies [7]. |
| Validation Comparator | Validation | Representative experimental data (in vitro or in vivo) used to assess the model's agreement with physical reality [6]. |
| Uncertainty Quantification | Uncertainty Analysis | Produces quantitative measures of confidence in simulation results by characterizing numerical and parametric uncertainties [102] [27]. |
| Risk Assessment Matrix | Risk Framework | Tool for systematically evaluating model influence and decision consequence to determine overall model risk [6] [103]. |
Quantitative Data and Comparative Analysis of Credibility Activities
The VVUQ framework does not prescribe universal acceptance criteria but emphasizes that credibility goals must be risk-informed. The following table synthesizes example quantitative data and comparative rigor levels for key credibility activities, drawing from implementations discussed in the search results.
Table 3: Quantitative Data and Comparison of Credibility Activities
| Credibility Factor | Low-Risk Context | High-Risk Context | Measurement Metrics |
|---|---|---|---|
| Discretization Error (Verification) | Grid convergence index < 10% [104] | Grid convergence index < 3% [7] | Grid Convergence Index (GCI), Richardson Extrapolation [7] |
| Output Validation | Qualitative trend agreement | Quantitative comparison with strict statistical equivalence [6] | Statistical equivalence testing (e.g., p > 0.05), R² value [6] |
| Model Input Uncertainty | Single-point estimates | Probabilistic distributions with sensitivity analysis [27] | Sensitivity indices (e.g., Sobol), confidence intervals [27] |
| Code Verification | Comparison with analytical solutions for standard cases [104] | Comprehensive suite of analytical and manufactured solutions [104] | Error norms (L1, L2, L∞) relative to exact solutions [104] |
Application of this risk-based approach is illustrated by recent research in patient-specific computational models. One working group is developing a classification framework for comparators used to validate patient-specific models for femur-fracture prediction, highlighting how credibility activities evolve for high-consequence applications [7]. Similarly, the importance of systematic mesh refinement is emphasized in blood hemolysis modeling, where non-systematic approaches can yield misleading verification results [7].
Future Directions and Cross-Domain Applications
The principles exemplified in VVUQ 40.1 are rapidly propagating beyond traditional engineering into new domains, indicating the framework's versatility. Several key emerging trends demonstrate the future direction of credibility examples:
In Silico Clinical Trials: The credibility demands for ISCTs present unique challenges, as direct validation against human data is often limited by practical and ethical constraints. The ASME VVUQ 40 Sub-Committee is actively exploring how the risk-based framework can be adapted for these high-consequence applications where simulation may augment or replace human trials [7].
Patient-Specific Model Credibility: A dedicated working group within the VVUQ 40 Sub-Committee is developing a new technical report focused on patient-specific models (e.g., for femur-fracture prediction). This effort includes creating a classification framework for different types of comparators, addressing the unique challenge of validating models for individual patients rather than population averages [7].
AI Model Credibility: The FDA has explicitly adopted a nearly identical risk-based framework for establishing AI model credibility in drug development [73] [103]. This cross-pollination demonstrates the broader utility of the VVUQ approach beyond traditional physics-based models.
Digital Twin Credibility: Research is ongoing to extend VVUQ standards for digital twins in manufacturing, where continuous validation and uncertainty quantification throughout the system life cycle present new challenges beyond initial model qualification [27].
These developments signal a concerted move toward standardized, yet adaptable, credibility frameworks across multiple industries and application domains, with VVUQ 40.1 serving as a foundational template for future technical reports and standards.
In silico clinical trials (ISCTs), which use computer simulations to evaluate medical products, are transitioning from a promising technology to a validated component of drug and device development. Their acceptance by regulatory bodies and the scientific community hinges on a critical factor: credibility. Establishing this credibility requires a multi-faceted strategy, blending rigorous risk-based frameworks, robust clinical validation, and transparent methodology. This guide examines the current standards and experimental protocols that underpin credible ISCTs, providing a comparative analysis for research professionals.
Theoretical Foundations: Risk-Based Credibility Frameworks
The credibility of a computational model is not a binary state but a function of the context in which it is used. A risk-based framework is the cornerstone of modern ISCT validation, ensuring that the level of evidence required is proportional to the model's intended impact on regulatory or development decisions.
The Model Risk Assessment Framework evaluates the risk associated with a specific ISCT application based on three independent factors [106]:
- Scope: Is the model used to support a single decision or to provide comprehensive evidence for a product's safety and efficacy?
- Coverage: What proportion of the total evidence for a regulatory submission is generated by the ISCT?
- Severity: What is the potential impact on patient health if the model produces an incorrect prediction?
This risk assessment then directly informs the Credibility Requirements, which focus on the clinical validation activities. The credibility factors specific to these activities include [106]:
- Clinical Comparator: The quality, statistical power, and clinical variability of the real-world dataset used to validate the virtual cohort.
- Validation Model: The representativeness and accounting for clinical variability within the virtual cohort itself.
- Agreement: The rigor of the statistical comparison between the validation model and the clinical comparator, including both input and output agreement.
- Applicability: The similarity between the device or treatment used in the validation activities and the one being tested in the intended ISCT.
This framework ensures that models used in high-stakes decisions, such as replacing a Phase III trial, undergo far more extensive validation than those used for early-stage dose selection.
Validation in Practice: Protocols and Quantitative Outcomes
Theoretical frameworks are brought to life through concrete experimental protocols. The following case studies and datasets illustrate how credibility is built and demonstrated in different therapeutic areas.
Case Study: AI-Driven Drug Discovery for IPF
A landmark example is the development and validation of Rentosertib, a TNIK inhibitor for Idiopathic Pulmonary Fibrosis (IPF) discovered and designed using a generative AI platform. The subsequent Phase IIa clinical trial served as a crucial validation step for both the drug and the AI discovery platform [107].
Experimental Protocol:
- Objective: To evaluate the safety, tolerability, and efficacy of Rentosertib in patients with IPF.
- Trial Design: A double-blind, placebo-controlled trial (GENESIS-IPF) across 22 sites.
- Participants: 71 IPF patients randomly assigned to placebo, 30 mg QD, 30 mg BID, or 60 mg QD Rentosertib.
- Duration: 12 weeks of treatment.
- Primary Endpoint: Safety and tolerability profile.
- Secondary Endpoint: Change in Forced Vital Capacity (FVC), a gold-standard measure of lung function.
- Exploratory Analysis: Dose- and time-dependent changes in serum protein biomarkers (e.g., COL1A1, MMP10, FAP, IL-10) and their correlation with FVC changes.
Quantitative Outcomes: Table 1: Key Efficacy and Biomarker Results from Rentosertib Phase IIa Trial [107]
| Parameter | Placebo Group | Rentosertib 60 mg QD Group | Statistical Note |
|---|---|---|---|
| Mean FVC Change from Baseline | -20.3 mL | +98.4 mL | Greatest improvement in the high-dose group. |
| Profibrotic Protein Reduction | -- | Significant reduction in COL1A1, MMP10, FAP | Dose-dependent change observed. |
| Anti-inflammatory Marker | -- | Significant increase in IL-10 | Dose-dependent change observed. |
| Correlation with FVC | -- | Protein changes correlated with FVC improvement | Supports biological mechanism. |
The trial successfully validated the AI-discovered target, demonstrating a manageable safety profile and positive efficacy signal. The exploratory biomarker analysis provided crucial evidence linking the drug's mechanism of action to clinical outcomes, thereby validating the biological assumptions built into the AI platform [107].
Validation Tooling: Open-Source Statistical Environments
Beyond single-case validation, the field requires generic tools for ongoing assessment. The SIMCor project, an EU-Horizon 2020 initiative, developed an open-source statistical web application for validating virtual cohorts and analyzing ISCTs [108].
Experimental Protocol for Virtual Cohort Validation:
- Data Input: Load the virtual cohort dataset and the real-world clinical dataset intended to serve as the comparator.
- Cohort Comparison: The application provides a menu of statistical techniques to compare the two cohorts.
- Descriptive Statistics: Generate summary statistics for both cohorts to compare population baselines.
- Graphical Analysis: Create plots (e.g., histograms, scatter plots) to visualize the distribution of key variables in both cohorts.
- Statistical Tests: Perform tests (e.g., Kolmogorov-Smirnov) to assess the similarity between the virtual and real populations.
- Output: A comprehensive report detailing the degree of agreement, which supports the judgement of whether the virtual cohort is sufficiently representative for its intended use.
This tool, built on R/Shiny and issued under a GNU-2 license, addresses a critical gap by providing a user-friendly, open platform for a fundamental step in establishing ISCT credibility [108].
The Research Toolkit: Essential Reagents and Platforms
Building and validating credible ISCTs requires a suite of technological and methodological "reagents." The table below details key solutions and their functions in the ISCT workflow.
Table 2: Essential Research Reagent Solutions for In Silico Clinical Trials
| Research Reagent Solution | Primary Function | Examples / Context of Use |
|---|---|---|
| Mechanistic Modeling Platforms | Simulate the interaction between a therapy and human biological systems. | Physiologically Based Pharmacokinetic (PBPK) models; Quantitative Systems Pharmacology (QSP) models [22]. |
| Virtual Patient Cohort Generators | Create synthetic, representative patient populations for simulation. | Use Generative Adversarial Networks (GANs) and large language models (LLMs) to generate cohorts with specified characteristics [22]. |
| Open-Source Validation Software | Statistically compare virtual cohorts to real-world datasets to validate representativeness. | The SIMCor R-statistical web application provides a menu-driven environment for validation analysis [108]. |
| Cloud-Native Simulation Frameworks | Provide scalable, high-performance computing power to run complex, resource-intensive simulations. | Pay-per-use exascale GPU clusters from global cloud providers democratize access to necessary compute power [109] [17]. |
| AI-powered Predictive Algorithms | Act as surrogate models to approximate complex simulations faster or predict clinical outcomes. | Machine learning models used to predict toxicity, optimize trial design, and forecast patient recruitment [110] [111]. |
| Digital Twin Constructs | Create a virtual replica of an individual patient's physiology to test interventions personalized. | Used in oncology to simulate tumor growth and response, and in cardiology to model device implantation [19] [109]. |
Visualizing the Credibility Pathway
The journey from model development to a credible ISCT involves a structured, iterative process of verification and validation. The workflow below maps this critical pathway.
This workflow highlights the non-linear, iterative nature of establishing credibility. The regulatory credibility assessment, guided by frameworks like the FDA's and standards like ASME V&V 40, determines whether the evidence is sufficient or requires refinement and re-submission [106] [111].
The validation of in silico clinical trials is an exercise in building trust through evidence. A risk-based framework ensures that validation efforts are commensurate with the decision-making stakes, while concrete experimental protocols—from prospective clinical trials to statistical validation of virtual cohorts—provide the necessary proof. As regulatory acceptance grows, evidenced by the FDA's phased removal of animal testing mandates for some drugs and its guidance on computational modeling for devices, the demand for rigorous, transparent, and validated ISCTs will only intensify [19] [111]. For researchers and drug developers, mastering the credibility demands outlined here is not merely academic; it is a fundamental prerequisite for leveraging the full potential of in silico methods to create safer and more effective therapies.
Conclusion
Establishing computational model credibility is not a one-time task but a continuous, risk-informed process integral to biomedical innovation. The synthesis of foundational frameworks like ASME V&V 40, rigorous methodological application of V&V, proactive troubleshooting of data and bias issues, and robust comparative validation creates a foundation of trust necessary for regulatory acceptance and clinical impact. As the field advances, the proliferation of in silico clinical trials and patient-specific models will further elevate the importance of standardized credibility assessment. Future success will depend on the widespread adoption of these practices, ongoing development of domain-specific technical reports, and a cultural commitment to transparency and ethical AI, ultimately accelerating the delivery of safe and effective therapies to patients.
References
- 1. Assessing Computational Model Credibility Using a Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6493688/]
- 2. Adapting modeling and simulation credibility standards to ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04290-5]
- 3. Assessing the Credibility of Computational Modeling and ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/assessing-credibility-computational-modeling-and-simulation-medical-device-submissions]
- 4. VV 40 - Assessing Credibility of Computational Modeling ... [https://www.asme.org/codes-standards/find-codes-standards/assessing-credibility-of-computational-modeling-through-verification-and-validation-application-to-medical-devices]
- 5. Credibility of Computational Models Program: Research on ... [https://www.fda.gov/medical-devices/medical-device-regulatory-science-research-programs-conducted-osel/credibility-computational-models-program-research-computational-models-and-simulation-associated]
- 6. Consideration of a Credibility Assessment Framework in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6966181/]
- 7. Current Applications and Future Developments of the ASME ... [https://dmd.umn.edu/2025/vv40]
- 8. Scientific and regulatory evaluation of mechanistic in silico ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8376137/]
- 9. Risk-based evaluation of machine learning-based ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-02909-9]
- 10. The computational model lifecycle: Opportunities and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402556/]
- 11. Adapting modeling and simulation credibility standards to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10369698/]
- 12. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 13. The ASME V&V 40 Standard [https://dmd.umn.edu/2023/vv-40]
- 14. FDA vs EMA: Key Regulatory Differences for ... [https://lsacademy.com/en/fda-vs-ema-key-regulatory-differences-for-pharmaceuticals/]
- 15. EMA & FDA: What Are the Similarities & Differences in Risk ... [https://www.biomapas.com/ema-and-fda-risk-management/]
- 16. A Rubric for Assessing Conformance to the Ten Rules ... [https://ntrs.nasa.gov/citations/20240003228]
- 17. In Silico Clinical Trials Market Size & Share Forecast 2030 [https://www.mordorintelligence.com/industry-reports/in-silico-clinical-trial-market]
- 18. FDA Announces Plan to Phase Out Animal Testing ... [https://www.fda.gov/news-events/press-announcements/fda-announces-plan-phase-out-animal-testing-requirement-monoclonal-antibodies-and-other-drugs]
- 19. In Silico Research Is Rewriting the Rules of Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070237/]
- 20. A Recent Timeline of U.S. Actions to Reduce and Replace ... [https://emulatebio.com/alternatives-to-animal-testing-in-drug-development/]
- 21. Credibility assessment of computational models according ... [https://www.sciencedirect.com/science/article/pii/S0169260723003930]
- 22. How in silico trials are reshaping clinical development [https://www.zs.com/insights/in-silico-trials-clinical-research]
- 23. In-Silico Clinical Trials Market to hit $6.39B by 2033 [https://www.einpresswire.com/article/868133151/in-silico-clinical-trials-market-to-hit-6-39b-by-2033-key-growth-drivers-outlook-2025]
- 24. In-Silico Clinical Trials Market Growth, Trends & Forecast ... [https://www.datamintelligence.com/research-report/in-silico-clinical-trials-market]
- 25. Decision Inputs in Drug Development—Big Vs. Small Pharma [https://www.appliedclinicaltrialsonline.com/view/decision-inputs-drug-development-big-small-pharma]
- 26. Regulatory Adoption of AI, ML, Computational Modeling & ... [https://pubmed.ncbi.nlm.nih.gov/41055689/]
- 27. Credibility consideration for digital twins in manufacturing [https://www.sciencedirect.com/science/article/abs/pii/S2213846322002097]
- 28. Verification, Validation and Sensitivity Studies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3361760/]
- 29. Finite Element Mesh Refinement Definition and Techniques [https://www.comsol.com/multiphysics/mesh-refinement]
- 30. Ansys Mechanical in 2025 R1: Advanced Techniques for Mesh ... [https://blog.cadfem.ai/ansys-mechanical-in-2025r1/]
- 31. Frontiers | Finite element analysis of cardiovascular stent frames... [https://www.frontiersin.org/journals/medical-engineering/articles/10.3389/fmede.2025.1606951/full]
- 32. Error Estimation in Engineering Refining - Simple Science Models [https://scisimple.com/en/articles/2025-11-10-refining-error-estimation-in-engineering-models--a9rq4mq]
- 33. CMES | A Simple and Robust Mesh Implementation in... Refinement [https://www.techscience.com/CMES/v144n3/63944]
- 34. Current Needs, Gaps, and Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7179957/]
- 35. A "Threshold-based" Approach to Determining an Acceptance ... [https://cdrh-rst.fda.gov/threshold-based-approach-determining-acceptance-criterion-computational-model-validation]
- 36. Essential guidelines for computational method benchmarking [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584985/]
- 37. DeepDTAGen: a multitask deep learning framework for ... [https://www.nature.com/articles/s41467-025-59917-6]
- 38. Making science run at the speed of thought: the reality of AI ... [https://www.drugtargetreview.com/article/190632/making-science-run-at-the-speed-of-thought-the-reality-of-ai-in-drug-discovery-part-1/]
- 39. ICME | CAVS [https://www.cavs.msstate.edu/icme/DesignOpt/Uncertainty.php]
- 40. 5 Model Validation and Prediction | Assessing the Reliability of... [https://nap.nationalacademies.org/read/13395/chapter/7]
- 41. Calibration after bootstrap for accurate uncertainty in... quantification [https://www.nature.com/articles/s41524-022-00794-8?error=cookies_not_supported&code=8d43777d-97f5-4229-a601-13d727c28768]
- 42. Addressing low statistical power in computational ... [https://www.nature.com/articles/s41562-025-02348-6]
- 43. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 44. Optimized FDA Blood Pump: A Case Study in System ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12575595/]
- 45. Computational fluid dynamics analysis and experimental ... [https://www.sciencedirect.com/science/article/pii/S2590093522000406]
- 46. Comparative Study of Turbulence Models for Hemolysis ... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5431214]
- 47. Characteristics and hemolysis analysis of centrifugal blood ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1575971/full]
- 48. Optimized FDA Blood Pump: A Case Study in System ... [https://link.springer.com/article/10.1007/s10439-025-03834-8]
- 49. Computational fluid dynamics simulating of the FDA ... [https://pubmed.ncbi.nlm.nih.gov/39177925/]
- 50. Ghost Cells as a Two‐Phase Blood Analog Fluid [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625480/]
- 51. Craven Enhances Baylor's Biomedical Engineering Research [https://www.ecs.baylor.edu/news/story/2025/craven-enhances-baylors-biomedical-engineering-research]
- 52. ( Explainable ) in AI : Balancing Performance and Interpretability XAI 2025 [https://www.suryasys.com/post/explainable-ai-xai-in-2025-balancing-performance-and-interpretability]
- 53. What Is AI Transparency? [https://www.ibm.com/think/topics/ai-transparency]
- 54. ( Explainable ) in AI : How to Trust XAI in 2025 AI 2025 [https://blog.bismart.com/en/explainable-ai-business-trust]
- 55. : Bringing Transparency And Trust To Algorithmic Decisions XAI [https://www.forbes.com/councils/forbestechcouncil/2025/02/14/the-rise-of-explainable-ai-bringing-transparency-and-trust-to-algorithmic-decisions/]
- 56. What is AI transparency? A comprehensive guide [https://www.zendesk.com/blog/ai-transparency/]
- 57. Top 10 Tools for Achieving AI Transparency and ... [https://superagi.com/top-10-tools-for-achieving-ai-transparency-and-explainability-in-2025-2/]
- 58. What is AI transparency? - Explained in detail (2025) [https://www.tredence.com/blog/navigating-ai-transparency-evaluating-explainable-ai-systems-for-reliable-and-transparent-ai]
- 59. Top 10 AI Transparency Reporting Tools in 2025 [https://www.devopsschool.com/blog/top-10-ai-transparency-reporting-tools-in-2025-features-pros-cons-comparison/]
- 60. The future of AI regulation in drug development: a comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598624/]
- 61. Bias in AI | Examples, Causes & Mitigation Strategies 2025 [https://kodexolabs.com/bias-in-ai/]
- 62. Regulating the Use of AI in Drug Development: Legal ... [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 63. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 64. Practical Perspectives on Enhancing Predictive Modeling ... [https://link.springer.com/article/10.1007/s40495-025-00426-x]
- 65. Data Quality Management for AI Success: Your 2025 Guide [https://www.alation.com/blog/data-quality-management-ai-success-2025/]
- 66. Mitigating Data Bias in AI Practices - Trailhead [https://trailhead.salesforce.com/content/learn/modules/data-bias-recognition-and-prevention/mitigate-data-bias]
- 67. Complexity, simplicity, and credibility in mathematical biology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12002325/]
- 68. AI in Pharma and Biotech: Market Trends 2025 and Beyond [https://www.coherentsolutions.com/insights/artificial-intelligence-in-pharmaceuticals-and-biotechnology-current-trends-and-innovations]
- 69. Pharma's AI Skills Gap: A 2025 Data-Driven Analysis [https://intuitionlabs.ai/articles/pharma-ai-skills-gap]
- 70. AI Talent Shortage: Why It Exists and How Companies Can ... [https://qubit-labs.com/ai-talent-shortage/]
- 71. The Fearless Future: 2025 Global AI Jobs Barometer [https://www.pwc.com/gx/en/services/ai/ai-jobs-barometer.html]
- 72. Top 50+ Global AI Talent Shortage Statistics 2025 [https://www.secondtalent.com/resources/global-ai-talent-shortage-statistics/]
- 73. FDA Proposes Framework to Advance Credibility of AI ... [https://www.fda.gov/news-events/press-announcements/fda-proposes-framework-advance-credibility-ai-models-used-drug-and-biological-product-submissions]
- 74. Advarra's Perspective on FDA's Draft AI Guidance [https://www.advarra.com/blog/advarras-perspective-on-fdas-draft-ai-guidance-advancing-responsible-innovation/]
- 75. Integrating Legacy Systems: How to Do It and What ... [https://www.confluent.io/learn/legacy-system-integration/]
- 76. How to Integrate Legacy Systems: Top Challenges and ... [https://devsquad.com/blog/integrate-legacy-systems]
- 77. Busting the Legacy System Integration Myth: AI's Seamless ... [https://thetaray.com/busting-the-legacy-system-integration-myth-ais-seamless-fit/]
- 78. 10 Workflow Optimization Best Practices for 2024 - Comidor [https://www.comidor.com/blog/business-process-management/workflow-optimization-best-practices/]
- 79. Compliance workflow best practices for company growth [https://www.diligent.com/resources/blog/compliance-workflow-best-practices]
- 80. Toward a more credible assessment of the ... - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11420151/]
- 81. A rubric for assessing conformance to the Ten Rules for ... [https://pubmed.ncbi.nlm.nih.gov/40560895/]
- 82. AI and Privacy: Shifting from 2024 to 2025 | CSA [https://cloudsecurityalliance.org/blog/2025/04/22/ai-and-privacy-2024-to-2025-embracing-the-future-of-global-legal-developments]
- 83. Technical Performance | The 2025 AI Index Report [https://hai.stanford.edu/ai-index/2025-ai-index-report/technical-performance]
- 84. Data Privacy Trends Shaping 2025 and the Years Ahead [https://usercentrics.com/guides/data-privacy/data-privacy-trends/]
- 85. Data Privacy in 2025: 7 Trends Every CDO Needs to ... [https://www.alation.com/blog/data-privacy-in-2025-trends/]
- 86. New Research Shows How Strict Data Regulations ... [https://itif.org/publications/2025/10/10/the-relationship-between-data-protection-regulation-and-biopharmaceutical-r-and-d/]
- 87. Data Privacy & AI Ethics Best Practices - TrustCommunity [https://community.trustcloud.ai/docs/grc-launchpad/grc-101/governance/data-privacy-and-ai-ethical-considerations-and-best-practices/]
- 88. Model Integration in Computational Biology: The Role of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10002468/]
- 89. SBML.org [https://sbml.org/]
- 90. The CellML 1.1 Specification [https://pubmed.ncbi.nlm.nih.gov/26528557/]
- 91. SBML [https://en.wikipedia.org/wiki/SBML]
- 92. Standards [https://www.systems-biology.org/2003/04/standards.html]
- 93. SBML Specifications [https://sbml.org/documents/specifications/]
- 94. Evaluation framework for systems models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8923730/]
- 95. Credibility Assessment of the Patient-Specific Modeling ... [https://link.springer.com/article/10.1007/s13239-025-00801-1]
- 96. Credibility assessment of patient-specific modeling in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471802/]
- 97. In the literature: October 2025 highlights [https://www.vph-institute.org/news/in-the-literature-october-2025-highlights.html]
- 98. Benchmarking large language models for personalized ... [https://www.nature.com/articles/s41746-025-01996-2]
- 99. Benchmarking the Confidence of Large Language Models in ... [https://medinform.jmir.org/2025/1/e66917]
- 100. Why high-quality clinical development data is essential [https://www.intelligencia.ai/high-quality-clinical-development-data/]
- 101. Top 50 AI Model Benchmarks & Evaluation Metrics (2025 Guide) [https://o-mega.ai/articles/top-50-ai-model-evals-full-list-of-benchmarks-october-2025]
- 102. Verification, Validation and Uncertainty Quantification ... [https://www.asme.org/codes-standards/publications-information/verification-validation-uncertainty]
- 103. A Model's Credibility Is in the Details: FDA Draft Guidance ... [https://www.troutman.com/insights/a-models-credibility-is-in-the-details-fda-draft-guidance-on-the-use-of-ai-models-in-drug-and-biological-product-development/]
- 104. Overview of CFD Verification & Validation [https://www.grc.nasa.gov/www/wind/valid/tutorial/overview.html]
- 105. Understand the Difference Between Verification and ... [https://www.isixsigma.com/measurement-systems-analysis-msa-gage-rr/understand-the-difference-between-verification-and-validation/]
- 106. A risk and credibility framework for in silico clinical trials of ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260723004790]
- 107. Insilico Announces Nature Medicine Publication of Phase ... [https://insilico.com/tpost/tnrecuxsc1-insilico-announces-nature-medicine-publi]
- 108. An open source statistical web application for validation ... [https://www.nature.com/articles/s41598-025-99720-3]
- 109. In Silico Clinical Trials Market Size & Share 2025-2032 [https://www.360iresearch.com/library/intelligence/in-silico-clinical-trials]
- 110. Clinical trial data analytics: Revolution in 2025 [https://lifebit.ai/blog/clinical-trial-data-analytics/]
- 111. In Silico Trials - Transforming Medical Device Innovation [https://www.biomedstat.com/knowledge-base/in-silico-trials-medical-device]