From Code to Cure: How CADD is Revolutionizing Antibiotic Discovery Against Superbugs
This article provides a comprehensive overview of Computer-Aided Drug Design (CADD) in the fight against antimicrobial resistance (AMR).
From Code to Cure: How CADD is Revolutionizing Antibiotic Discovery Against Superbugs
Abstract
This article provides a comprehensive overview of Computer-Aided Drug Design (CADD) in the fight against antimicrobial resistance (AMR). Targeting researchers and drug development professionals, it explores the foundational principles of targeting resistant pathogens, details core methodologies like virtual screening and structure-based design, addresses common computational and biological challenges, and evaluates validation strategies through case studies. The synthesis offers a roadmap for integrating CADD into the next generation of antimicrobial pipelines.
Understanding the Enemy: CADD's Role in Targeting Resistant Pathogens
Antimicrobial Resistance (AMR) is a complex global health threat driven by the overuse and misuse of antimicrobials in humans, animals, and agriculture. The following table summarizes the current burden and projected impact, highlighting the urgent need for intervention.
Table 1: The Global Burden and Economic Impact of AMR (2022-2050 Projections)
| Metric | Current/Projected Figure | Source & Year | Key Implication |
|---|---|---|---|
| Direct Annual Deaths (Global) | ~1.27 million (attributable), ~4.95 million (associated) | The Lancet, 2022 | AMR is a leading cause of death worldwide, exceeding HIV/AIDS and malaria. |
| Projected Annual Deaths by 2050 | Up to 10 million | O'Neill Review, 2016 | Without action, AMR could cause more deaths than cancer. |
| Additional Healthcare Cost & Productivity Loss (US, Annual) | >$55 billion | CDC, 2019 | AMR imposes a severe financial burden on health systems and economies. |
| Global GDP Loss by 2050 (Cumulative) | $100 trillion | World Bank, 2017 | AMR threatens global economic stability and development goals. |
| Pipeline Sufficiency (Bacteria-focused) | 43% of 32 late-stage candidates are non-traditional | WHO, 2023 | The clinical pipeline remains insufficient and lacks innovation against critical pathogens. |
The Scientific Challenge: Key Resistance Mechanisms
The evolution of resistance is mediated through specific, exploitable biological mechanisms. The primary pathways are summarized below.
Table 2: Major Antimicrobial Resistance Mechanisms and Examples
| Mechanism | Description | Pathogen Example | Drug Class Affected |
|---|---|---|---|
| Enzymatic Inactivation | Production of enzymes that degrade or modify the drug. | E. coli (ESBL, NDM-1) | β-lactams (Penicillins, Cephalosporins, Carbapenems) |
| Target Modification | Genetic mutation or enzymatic alteration of the drug's binding site. | MRSA (mecA gene), Mycobacterium tuberculosis | β-lactams, Fluoroquinolones |
| Efflux Pump Upregulation | Overexpression of transporters that actively expel the drug from the cell. | Pseudomonas aeruginosa, Acinetobacter baumannii | Tetracyclines, Macrolides, Fluoroquinolones |
| Membrane Permeability Reduction | Loss of porins or changes in membrane structure to limit drug uptake. | P. aeruginosa (loss of OprD) | Carbapenems, Aminoglycosides |
| Bypass Pathway | Development of an alternative metabolic pathway unaffected by the drug. | MRSA (alternative PBP2a) | β-lactams |
Diagram Title: Core Mechanisms of Antimicrobial Resistance
Computational-Aided Drug Discovery (CADD) Protocols
Integrating CADD into the discovery workflow accelerates the identification of novel therapeutics targeting resistance mechanisms.
Protocol 3.1: Structure-Based Virtual Screening for Novel Efflux Pump Inhibitors
Objective: To identify small-molecule inhibitors of the E. coli AcrB efflux pump proton transporter subunit using a high-resolution crystal structure.
Reagents & Materials:
- Protein Data Bank (PDB) ID: 4DX5 (AcrB proton transporter, inhibited state).
- Chemical Libraries: ZINC15 "Fragment Now" subset, Enamine REAL Diversity-Oriented Synthesis (DOS) library.
- Software: UCSF Chimera (preparation), AutoDock Vina (docking), PyMOL (visualization), Open Babel (format conversion).
- Hardware: High-performance computing cluster with GPU acceleration.
Procedure:
- Target Preparation:
- Download PDB file 4DX5. Remove co-crystallized ligand, water molecules, and heteroatoms.
- Add polar hydrogen atoms and compute Gasteiger partial charges using UCSF Chimera.
- Define the binding site grid box centered on the known inhibitor (e.g., D13-9001) binding pocket in the transmembrane region. Set box dimensions to 20x20x20 Å.
- Ligand Library Preparation:
- Download ~10,000 drug-like compounds from specified libraries in SDF format.
- Convert to PDBQT format using Open Babel, enumerating protonation states at pH 7.4.
- Molecular Docking:
- Execute AutoDock Vina in batch mode. Use an exhaustiveness value of 32 for thorough sampling.
- Dock each ligand into the defined grid box. Output the top 9 binding poses per ligand ranked by Vina score (kcal/mol).
- Post-Docking Analysis:
- Cluster results by binding pose and chemical scaffold. Select top 200 compounds based on score and interaction profile (e.g., key hydrogen bonds with residues Arg620, Asn274).
- Visually inspect top 50 complexes in PyMOL for sensible binding modes.
Protocol 3.2: Pharmacophore Modeling for Broad-Spectrum β-Lactamase Inhibitors
Objective: To generate a ligand-based pharmacophore model from known serine β-lactamase inhibitors (e.g., avibactam, relebactam) to screen for novel scaffolds.
Reagents & Materials:
- Ligand Set: 3D structures of 15 known covalent and non-covalent β-lactamase inhibitors (SDF format).
- Software: MOE (Molecular Operating Environment) or LigandScout.
- Database: ChEMBL database filtered for molecules with reported activity against class A β-lactamases.
Procedure:
- Ligand Preparation & Alignment:
- Energy minimize all 15 inhibitor structures using the MMFF94x forcefield.
- Perform flexible structural alignment based on the shared pharmacophoric features.
- Model Generation:
- Use the "Pharmacophore Query" module to identify common features: a) Anionic center (carboxylate/sulfate), b) Hydrogen bond acceptor (carbonyl oxygen), c) Two hydrophobic aromatic centers.
- Define geometric constraints (distances, angles) between features based on the aligned set.
- Validate model by screening a decoy set; calculate Guner-Henry score (>0.7 acceptable).
- Virtual Screening:
- Use the validated pharmacophore as a 3D query to screen the prepared ChEMBL subset.
- Retrieve and visually inspect the top 500 hits that match all critical features.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for AMR & CADD Integration Studies
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for broth microdilution antimicrobial susceptibility testing (AST). | Determining MIC values for novel hits against WHO priority pathogens. |
| Checkerboard Assay Plate (96-well) | Pre-formatted microtiter plate for efficient testing of drug combination synergy (e.g., novel inhibitor + existing antibiotic). | Evaluating the efficacy of a candidate efflux pump inhibitor in combination with levofloxacin. |
| Clinical Isolate Panels (ESKAPE Pathogens) | Defined sets of genetically characterized, multidrug-resistant clinical bacterial isolates. | Profiling the spectrum of activity of a new compound against real-world resistant strains. |
| β-Lactamase Enzymes (Recombinant, Purified) | Purified enzymes (e.g., NDM-1, KPC-2) for high-throughput enzymatic inhibition assays. | Validating hits from the pharmacophore screen in a biochemical inhibition assay. |
| Membrane Permeabilization Assay Kit | Uses fluorescent dyes (e.g., SYTOX Green) that only enter cells with compromised membranes. | Mechanistic study to confirm if a novel peptide disrupts bacterial outer membrane integrity. |
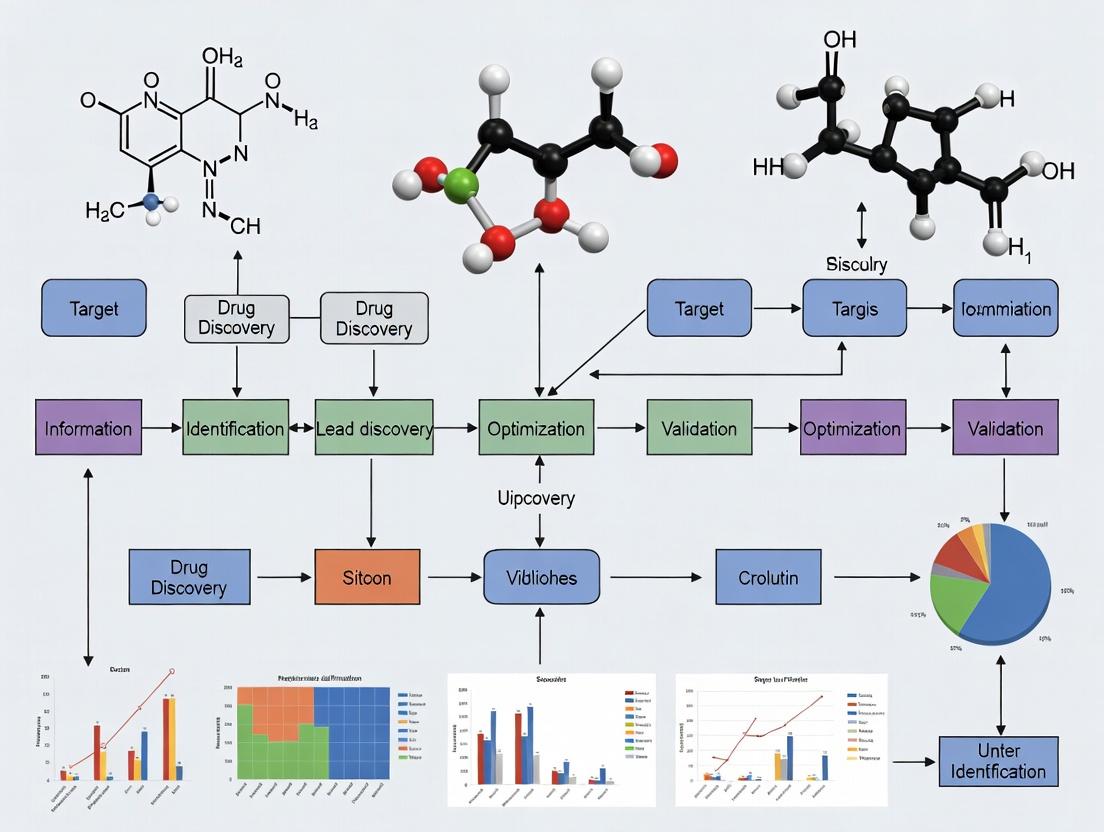
Diagram Title: Integrated CADD-Experimental Workflow for Novel Anti-AMR Therapeutics
Application Notes: CADD in AMR Drug Discovery
The global antimicrobial resistance (AMR) crisis necessitates accelerated discovery of novel agents against resistant pathogens. Computer-Aided Drug Design (CADD) provides a strategic framework to prioritize candidates, reduce experimental costs, and understand resistance mechanisms. This note details contemporary CADD applications targeting AMR.
Target Identification & Prioritization
Genomic and proteomic comparisons between resistant and susceptible strains identify potential targets. Essentiality and conservation analyses prioritize targets with broad-spectrum potential and low human homology.
Table 1: Prioritized AMR Targets from Recent Pan-Genomic Analyses (2023-2024)
| Target Protein (Pathogen) | Resistance Mechanism Addressed | Essentiality Score | Druggability (AF2 pLDDT) | Conserved Across Strains |
|---|---|---|---|---|
| LpxC (A. baumannii) | LPS biosynthesis, Colistin resistance | 0.98 | 92.1 | 99% |
| DNA Gyrase B (M. tuberculosis) | Fluoroquinolone resistance mutations | 0.96 | 89.7 | 100% |
| NDM-1 (K. pneumoniae) | Metallo-β-lactamase enzyme | N/A (non-essential) | 88.5 | 78% (plasmid-borne) |
| Ddl (E. faecium) | D-Ala-D-Ala ligase, Vancomycin resistance bypass | 0.91 | 85.2 | 95% |
Structure-Based Drug Design (SBDD)
High-resolution structures from AlphaFold2 DB and experimental crystallography enable virtual screening and rational design against previously intractable targets.
Table 2: Performance Metrics of SBDD Workflows Against AMR Targets (Recent Benchmarks)
| Method (Software) | Target Class | Avg. Enrichment Factor (Top 1%) | Avg. RMSD of Predicted Pose (Å) | Computational Cost (GPU hrs/1000 cpds) |
|---|---|---|---|---|
| Glide (XP) | Enzymes | 32.5 | 1.8 | 12.4 |
| AutoDock-GPU | Membrane Proteins | 18.7 | 2.5 | 4.2 |
| DiffDock | Novel Folds (AF2) | 25.1 | 2.1 | 8.7 (including inference) |
| FRED (OEDocking) | Protein-Protein Interfaces | 12.9 | 3.0 | 3.8 |
AI/ML for ADMET & Resistance Prediction
Graph Neural Networks (GNNs) and Transformer models predict compound activity, toxicity, and potential resistance emergence early in the pipeline.
Table 3: Predictive Model Performance for Key ADMET/Resistance Properties
| Model (Platform) | Prediction Task | Dataset Size | Avg. AUC-ROC | Key Features Used |
|---|---|---|---|---|
| MegaMolBART (Relenza) | hERG inhibition | 450,000 | 0.89 | SMILES, molecular graphs |
| DeepAR (In-house) | MIC against ESKAPE panel | 12,450 | 0.81 | ECFP6, 3D pharmacophores |
| RoBERTa (DrugResist) | Mutation-induced resistance likelihood | 8,120 mutations | 0.76 | Protein sequence, ligand fingerprint |
Experimental Protocols
Protocol 1: Structure-Based Virtual Screening for β-Lactamase Inhibitors
Objective: Identify novel, non-β-lactam scaffolds that inhibit the Class A β-lactamase KPC-2.
Materials:
- Hardware: GPU cluster node (minimum: NVIDIA V100, 32GB RAM).
- Software: UCSF ChimeraX, OpenBabel, AutoDock-GPU 1.2, Python 3.9+ with RDKit.
- Data: KPC-2 crystal structure (PDB: 5UL8), prepared library of 50,000 lead-like compounds (ZINC20).
Procedure:
- Target Preparation (ChimeraX):
- Load 5UL8. Remove water molecules and co-crystallized ligand.
- Add polar hydrogens. Assign AMBER ff14SB charges via DockPrep module.
- Define a grid box centered on the catalytic Ser70 residue (coordinates: x= -12.8, y= 17.2, z= 45.1). Set box dimensions to 20x20x20 Å.
- Ligand Library Preparation (OpenBabel/RDKit):
- Convert library from SDF to PDBQT format:
babel -isdf input.sdf -opdbqt output.pdbqt -xm -p 7.4. - Generate up to 10 conformers per ligand using RDKit's ETKDG method.
- Convert library from SDF to PDBQT format:
- Virtual Screening (AutoDock-GPU):
- Execute batch docking:
autodock_gpu_128wi -ffile target.pdbqt -lfile ligands.pdbqt -nrun 50 -heuristic 1. - Use Lamarckian Genetic Algorithm. Set population size to 150, energy evaluations to 2,500,000.
- Execute batch docking:
- Post-Docking Analysis:
- Rank compounds by predicted binding energy (ΔG in kcal/mol).
- Cluster top 500 poses by root-mean-square deviation (RMSD < 2.0 Å).
- Visually inspect top 50 unique scaffolds for key interactions with S70, K73, E166, and S130.
- Output: Ranked list of 200 top-scoring compounds for in vitro assay.
Protocol 2: AI-Driven De Novo Design of Gram-Negative Outer Membrane Permeators
Objective: Generate novel small molecules predicted to penetrate the Pseudomonas aeruginosa outer membrane via porins.
Materials:
- Hardware: Single NVIDIA A100 GPU, 64 GB CPU RAM.
- Software: REINVENT 4.0, PyTorch, OM permeability prediction model (trained on logP_op data).
- Data: SMILES of known porin-permeating molecules (n=1,200), PAO1 OM lipid composition profile.
Procedure:
- Agent Configuration (REINVENT):
- Load a pre-trained RNN as the Prior network.
- Define a custom Scoring Function (SF) combining:
- Predictive Model:
P(permeation) = 0.6 * [OM_model_output] - PhysChem Filters:
+ 0.2 * [1 if 200<MW<500 & -2<LogD<5 else 0] - Novelty Penalty:
- 0.2 * [Tanimoto similarity to known permeators > 0.7]
- Predictive Model:
- Set reinforcement learning parameters: σ=120, learning rate=0.0001.
- Generative Run:
- Initialize the Agent network as a copy of the Prior.
- Run for 500 epochs. In each epoch, the Agent generates 100 molecules, which are scored by the SF.
- The Agent's weights are updated to maximize the likelihood of generating high-scoring molecules.
- Validation & Output:
- Extract the top 50 unique scaffolds from the final epoch.
- Run MD-based membrane insertion simulations (PMX) on 5 selected candidates to validate porin localization.
- Output: A focused library of 50 generated compounds for synthesis and uptake assays.
Visualization
Diagram 1: CADD Workflow for AMR Target Discovery
Diagram 2: Key Resistance Mechanisms & CADD Intervention Points
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational Tools & Resources for CADD in AMR Research
| Item Name (Vendor/Provider) | Category | Function/Benefit in AMR CADD |
|---|---|---|
| AlphaFold2 Database (EMBL-EBI) | Protein Structure | Provides high-accuracy predicted structures for resistant pathogen targets lacking experimental data. |
| ZINC22 (UCSF) | Compound Library | Curated, purchasable library of >230 million compounds for virtual screening. |
| CARD Database (McMaster Uni) | Bioinformatics | Comprehensive repository of antimicrobial resistance genes, proteins, and mutations. |
| GLASS (Go Lab) | Screening Collection | A focused, physicochemically diverse library pre-filtered for predicted Gram-negative permeation. |
| ChEMBL (EMBL-EBI) | Bioactivity Data | Manually curated database of drug-like molecules with bioactivity data against pathogens. |
| AutoDock-GPU (Scripps) | Docking Software | Accelerated molecular docking suite enabling high-throughput virtual screening on GPU clusters. |
| GROMACS 2024 (Open Source) | Molecular Dynamics | Performs all-atom MD simulations to study drug-target binding stability and membrane permeation. |
| REINVENT 4.0 (Pfizer/Open) | AI Generative Model | Deep reinforcement learning framework for de novo molecular design optimized against custom rewards. |
| Open Babel (Open Source) | Cheminformatics | Converts chemical file formats, calculates descriptors, and filters compound libraries. |
| PyMOL 3.0 (Schrödinger) | Visualization | Critical for analyzing docking poses, protein-ligand interactions, and structural biology data. |
Application Note 1: Targeting Essential Bacterial Enzymes with CADD
Within the broader thesis of CADD applications in antimicrobial resistance (AMR) drug discovery, the inhibition of essential enzymes remains a cornerstone strategy. These targets are crucial for bacterial survival and proliferation, offering a direct path to bactericidal or bacteriostatic effects. CADD accelerates the identification and optimization of novel inhibitors by screening vast virtual libraries against high-resolution enzyme structures, predicting binding affinities, and optimizing lead compounds for potency and selectivity.
Table 1: Key Essential Enzyme Targets in AMR Drug Discovery
| Target Enzyme | Primary Function | Representative Pathogens | Known Inhibitor(s) | CADD Utility |
|---|---|---|---|---|
| DNA Gyrase/Topoisomerase IV | DNA replication & supercoiling | E. coli, S. aureus | Fluoroquinolones (e.g., Ciprofloxacin) | Structure-based design to overcome QRDR mutations. |
| Dihydrofolate Reductase (DHFR) | Folic acid synthesis | S. aureus, E. coli | Trimethoprim | Scaffold hopping to design analogs avoiding common resistant variants. |
| β-Lactamases | β-lactam antibiotic hydrolysis | K. pneumoniae, E. coli | Clavulanic acid, Avibactam | Virtual screening for novel, broad-spectrum β-lactamase inhibitors. |
| MurA (UDP-N-acetylglucosamine enolpyruvyl transferase) | Peptidoglycan biosynthesis | H. pylori, M. tuberculosis | Fosfomycin | Pharmacophore modeling to find new inhibitors of this validated target. |
| Ligand (Lip)G4 | Lipid A biosynthesis | P. aeruginosa, A. baumannii | CHIR-090 (experimental) | Molecular docking to optimize arylacetylene bisphosphonate scaffolds. |
Protocol 1.1: In Silico Screening for Novel DHFR Inhibitors
Objective: To identify novel, high-affinity inhibitors of bacterial DHFR using a CADD workflow.
Materials & Workflow:
- Target Preparation: Retrieve the crystal structure of Trimethoprim-resistant S. aureus DHFR (e.g., PDB ID: 2W9S) from the RCSB Protein Data Bank. Using molecular modeling software (e.g., Schrödinger Maestro, UCSF Chimera), remove water molecules, add hydrogens, assign bond orders, and optimize protonation states of key residues (e.g., Asp27, Ile20).
- Binding Site Definition: Define the active site using the coordinates of the bound folate or Trimethoprim. Generate a grid box encompassing the site with ~10 Å margin.
- Library Preparation: Prepare a virtual library of small molecules (e.g., ZINC20 fragment library) by generating 3D conformers and minimizing their energy.
- Virtual Screening: Perform high-throughput virtual screening (HTVS) using a docking program (e.g., AutoDock Vina, Glide). Screen compounds first with a fast, less precise method, then re-dock top hits (e.g., 1000 compounds) with higher precision.
- Post-Docking Analysis: Rank compounds by docking score (kcal/mol). Visually inspect top-ranking poses for key interactions: hydrogen bonds with Asp27 and Ile5, π-π stacking with Phe92. Apply filters for drug-likeness (Lipinski's Rule of Five).
- MM/GBSA Calculation: Refine binding affinity predictions for the top 100 hits using a more rigorous Molecular Mechanics/Generalized Born Surface Area (MM/GBSA) calculation.
Diagram: CADD Workflow for Enzyme Inhibitor Discovery
The Scientist's Toolkit: Research Reagents for Enzyme Inhibition Assays
- Recombinant Target Enzyme: Purified protein for in vitro activity assays.
- Fluorogenic/Luminescent Substrate: Enables real-time, high-throughput measurement of enzyme activity (e.g., Substrate for β-lactamase hydrolysis).
- Positive Control Inhibitor: Validated inhibitor (e.g., Trimethoprim for DHFR) to benchmark assay performance.
- ITC/MST Reagents: Isothermal Titration Calorimetry or Microscale Thermophoresis kits for direct measurement of binding affinity (Kd).
- 96/384-Well Assay Plates: For high-throughput screening of compound libraries.
Application Note 2: Disrupting Efflux Pumps via CADD
Efflux pumps are a major AMR mechanism, extruding diverse antibiotics and reducing intracellular concentration. CADD is instrumental in developing Efflux Pump Inhibitors (EPIs), which can restore the efficacy of existing antibiotics. Strategies include: 1) Designing competitive substrates that jam the pump, 2) Developing allosteric inhibitors that interfere with pump energy coupling or assembly, and 3) Identifying inhibitors of transcriptional regulators of pump expression (e.g., ramA, marR).
Table 2: Major Efflux Pump Families & CADD Strategies
| Pump Family | Energy Source | Key Example | Substrates | CADD Approach |
|---|---|---|---|---|
| RND (Resistance-Nodulation-Division) | Proton Motive Force | AcrAB-TolC (E. coli) | Tetracyclines, β-lactams, Fluoroquinolones | Docking into AcrB substrate binding pockets (Deep, Proximal). |
| MFS (Major Facilitator Superfamily) | Proton Motive Force | NorA (S. aureus) | Fluoroquinolones, Dyes | Pharmacophore modeling based on known EPIs like reserpine. |
| MATE (Multidrug and Toxic Compound Extrusion) | Na+ or H+ gradient | NorM (V. cholerae) | Fluoroquinolones, Aminoglycosides | Molecular dynamics to study Na+ ion binding and transport cycle. |
| ABC (ATP-Binding Cassette) | ATP Hydrolysis | MsrA (S. epidermidis) | Macrolides, Streptogramins | Targeting the ATPase nucleotide-binding domain (NBD). |
Protocol 2.1: Molecular Dynamics (MD) Simulation of AcrB with Inhibitor
Objective: To simulate the interaction dynamics and stability of a novel EPI bound to the AcrB efflux pump.
Materials & Workflow:
- System Setup: Use the crystal structure of AcrB (PDB ID: 4DX5). Dock the proposed EPI into the distal binding pocket. Use a tool like CHARMM-GUI to embed the protein-ligand complex in a phospholipid bilayer (e.g., POPE), solvate with TIP3P water, and add ions (Na+, Cl-) to neutralize the system (~0.15 M).
- Energy Minimization: Perform 5,000 steps of steepest descent minimization to remove steric clashes.
- Equilibration: Run a two-phase equilibration using NVT (constant Number, Volume, Temperature) for 100 ps, then NPT (constant Number, Pressure, Temperature) for 200 ps, gradually releasing restraints on the protein.
- Production MD: Run an unrestrained MD simulation for 100-200 ns using a GPU-accelerated engine (e.g., AMBER, GROMACS, NAMD). Maintain temperature at 310 K (Berendsen or Nosé-Hoover thermostat) and pressure at 1 bar (Parrinello-Rahman barostat).
- Trajectory Analysis: Analyze root-mean-square deviation (RMSD) of the protein and ligand, root-mean-square fluctuation (RMSF) of binding site residues, hydrogen bond occupancy, and interaction fingerprints over time.
Diagram: Efflux Pump Inhibition Pathways & CADD
The Scientist's Toolkit: Research Reagents for Efflux Studies
- Fluorometric Efflux Substrates: (e.g., Ethidium Bromide, Hoechst 33342) to visualize and quantify pump activity via fluorescence.
- Protonophore (CCCP): A positive control that dissipates proton motive force, inhibiting RND/MFS pumps.
- Real-time PCR Kits: To quantify efflux pump gene expression levels in response to treatment.
- Membrane Protein Purification Kits: For isolating functional efflux pumps for biochemical assays.
- Strains with Overexpressed/Deleted Pumps: Isogenic bacterial strains to confirm EPI mechanism of action.
Application Note 3: Targeting Biofilm Formation and Persistence
Biofilms are structured microbial communities encased in an extracellular polymeric substance (EPS), conferring up to 1000x increased antibiotic tolerance. CADD approaches target: 1) Quorum Sensing (QS) Systems: Disrupting bacterial communication (e.g., LasR/LuxR receptors in P. aeruginosa). 2) Second Messenger Systems: Inhibiting cyclic-di-GMP synthesis/degradation enzymes to reduce biofilm stability. 3) EPS Matrix Components: Designing enzymes or small molecules that degrade alginate, PNAG, or eDNA.
Table 3: CADD Targets for Anti-Biofilm Strategies
| Target System | Key Target/Protein | Function in Biofilm | CADD Strategy |
|---|---|---|---|
| Quorum Sensing | LasR receptor (P. aeruginosa) | Activates virulence & biofilm genes | Virtual screening for competitive antagonists of the autoinducer binding pocket. |
| c-di-GMP Signaling | Diguanylate Cyclase (DGC) | Synthesizes c-di-GMP, promotes biofilm | Structure-based design of inhibitors targeting the catalytic GG(D/E)EF domain. |
| EPS Matrix | PslG (P. aeruginosa) | Glycosyl hydrolase that degrades Psl | In silico screening for small-molecule activators of PslG. |
| Two-Component Systems | BfmS/BfmR (A. baumannii) | Regulates biofilm formation & adhesion | Targeting the histidine kinase (BfmS) ATP-binding site. |
Protocol 3.1: Pharmacophore Modeling for LasR Antagonists
Objective: To generate a pharmacophore model for screening virtual libraries to find novel LasR QS inhibitors.
Materials & Workflow:
- Ligand Set Curation: Collect 10-20 known LasR agonists (e.g., 3-oxo-C12-HSL) and antagonists (e.g., furanones, triazoles) with reported IC50 values. Prepare their 3D structures using a conformational search.
- Common Feature Pharmacophore Generation: Use software (e.g., Catalyst/HypoGen, Phase) to align multiple active antagonists and identify common chemical features: Hydrogen Bond Acceptors (HBA), Hydrogen Bond Donors (HBD), Hydrophobic (H) regions, and Aromatic Rings (R).
- Model Validation: Test the generated pharmacophore model by screening a small, known decoy set containing both actives and inactives. Calculate enrichment factors and receiver operating characteristic (ROC) curves to assess model quality.
- Virtual Screening: Use the validated model as a 3D query to screen a large commercial database (e.g., Enamine REAL). Retrieve compounds that match all or critical features of the pharmacophore.
- Post-Processing: Dock the retrieved hits into the LasR binding site (PDB ID: 3IX3) to refine the selection and predict binding poses.
Diagram: Multi-Target CADD Strategy Against Biofilms
The Scientist's Toolkit: Research Reagents for Biofilm Studies
- Microtiter Plate (96-well) for CV Staining: Polystyrene plates for growing and quantifying biofilms via crystal violet (CV) assay.
- Synthetic Autoinducers: (e.g., C4-HSL, 3-oxo-C12-HSL) for QS induction controls.
- c-di-GMP ELISA Kit: To quantify intracellular c-di-GMP levels upon treatment.
- Fluorescent Conjugates (ConA, WGA): Lectins for staining specific EPS polysaccharides (e.g., Psl, Pel) in confocal microscopy.
- Flow Cell Systems: For growing biofilms under continuous flow for advanced imaging and real-time disruption studies.
Leveraging Genomic and Structural Data from Resistant Bacterial Strains
Application Note AN-101: Integrating Genomic and Structural Data for CADD-Driven Target Identification
The growing crisis of antimicrobial resistance (AMR) necessitates novel strategies for drug discovery. This application note details a Computational-Aided Drug Design (CADD) workflow that integrates genomic data from resistant bacterial strains with high-resolution structural biology to identify and prioritize novel antimicrobial targets and compounds. This work is framed within a broader thesis that posits CADD as an essential accelerator for overcoming AMR by rationally designing inhibitors against validated, resistance-associated targets.
Core Data Workflow and Key Quantitative Insights
The process begins with the comparative genomic analysis of resistant versus susceptible bacterial isolates. Key metrics include Single Nucleotide Polymorphism (SNP) density, gene presence/absence, and the identification of non-synonymous mutations in putative target proteins. These genomic insights guide the selection of proteins for structural characterization.
Table 1: Summary of Genomic Analysis Metrics from a Prototypical K. pneumoniae Carbapenem-Resistant (CRKP) Study
| Metric | Susceptible Strain (n=50 isolates) | Resistant Strain (n=50 isolates) | Significance (p-value) |
|---|---|---|---|
| Avg. SNPs in penA (PBP2x) | 2.1 ± 1.5 | 18.7 ± 4.2 | <0.001 |
| Presence of blaKPC gene | 0% | 100% | <0.001 |
| Non-synonymous mutations in efflux pump regulator ramR | 12% | 94% | <0.001 |
| Copy number variation of acrAB efflux operon | 1.0 ± 0.1 | 2.3 ± 0.8 | <0.001 |
Structural data, primarily from X-ray crystallography and Cryo-EM, is used to understand the mechanistic basis of resistance conferred by mutations identified in Table 1. For instance, structures of mutant Penicillin-Binding Proteins (PBPs) with reduced antibiotic affinity or mutant beta-lactamases with extended spectrum activity are solved.
Table 2: Structural Impact of Common Resistance Mutations in Key Bacterial Targets
| Target Protein (PDB ID) | Resistance Mutation | Effect on Antibiotic Binding (ΔΔG, kcal/mol)* | Structural Consequence |
|---|---|---|---|
| PBP2a (7CIT) | M641F | +3.2 | Steric occlusion of drug entry channel |
| NDM-1 Beta-lactamase (6NIP) | M154L | +1.8 | Altered active site water network |
| DNA Gyrase (6F86) | S83L | +4.1 | Loss of key hydrogen bond with fluoroquinolone |
| MmpL3 (6AJG) | S288R | +2.5 | Electrostatic repulsion of inhibitor scaffold |
*Positive ΔΔG indicates destabilization of the drug-protein complex.
These integrated data streams feed directly into CADD pipelines for structure-based virtual screening (SBVS) and de novo design against the resistant variant of the target.
Protocol PRO-101: Structure-Based Virtual Screening Against a Resistance-Conferred Target Variant
Objective: To identify novel lead compounds that effectively bind to the mutant, resistance-associated form of a target protein (e.g., PBP2a M641F) using a sequential computational screening protocol.
Materials & Software:
- Hardware: High-performance computing cluster with GPU acceleration.
- Software: Molecular docking suite (e.g., Schrödinger Glide, AutoDock Vina), molecular dynamics (MD) simulation package (e.g., GROMACS, AMBER), cheminformatics toolkit (e.g., RDKit).
- Data Inputs:
- High-resolution protein structure of mutant target (from PDB or homology model).
- Prepared commercial screening library (e.g., Enamine REAL, ZINC20, ~1-10 million compounds).
Procedure:
Target Preparation (2-4 hours):
- Download the mutant protein structure (e.g., PDB: 7CIT chain A).
- Using a protein preparation wizard, add missing hydrogen atoms, assign correct protonation states for residues (especially in the active site) at physiological pH (7.4), and optimize hydrogen bonding networks.
- Define a grid box for docking centered on the binding site of the native ligand or the region impacted by the resistance mutation.
Ligand Library Preparation (3-5 hours):
- Download and curate a screening library in SMILES format.
- Generate 3D conformers for each compound using tools like OMEGA or RDKit.
- Apply standard energy minimization and assign correct partial charges (e.g., OPLS4, MMFF94s).
High-Throughput Virtual Screening (HTVS) & Standard Precision (SP) Docking (24-48 hours):
- Perform an initial, rapid HTVS docking of the entire library to the prepared mutant target grid.
- Select the top 10% of compounds ranked by docking score.
- Re-dock this subset using more rigorous SP docking with flexible sampling.
Post-Docking Analysis & Enrichment (8-12 hours):
- Cluster the top 1,000 SP hits based on chemical similarity.
- Select top-ranked representatives from each major cluster for visual inspection, focusing on compounds forming specific interactions with residues critical for function and/or compensating for the resistance mutation (e.g., forming new bonds with M641F).
Molecular Dynamics (MD) Simulation Validation (5-7 days):
- For the top 20-30 candidate complexes, run an MD simulation (e.g., 100 ns in explicit solvent).
- Analyze root-mean-square deviation (RMSD), ligand-protein interaction fingerprints, and binding free energies (using MMPBSA/GBSA).
- Prioritize compounds demonstrating stable binding poses and favorable calculated binding affinities to the mutant target.
Expected Outcome: A shortlist of 5-10 computationally validated lead compounds with predicted activity against the resistant bacterial target, ready for in vitro biochemical and antimicrobial testing.
Visualization of Workflows
Genomic & Structural Data Integration for CADD
The Scientist's Toolkit: Research Reagent Solutions for Featured Protocols
| Item | Function & Application |
|---|---|
| Resistant Strain Panels (e.g., CRISPR-BAGEL, BEI Resources) | Validated, quality-controlled genomic DNA from pan-resistant bacterial strains (e.g., CRKP, MRSA) for benchmarking genomic analyses and resistance gene detection. |
| Cloning & Expression Kits for Mutant Proteins (e.g., NEB HiFi Assembly, pET vectors) | Essential for constructing plasmids expressing the specific mutant target proteins identified from genomic data, enabling their production for structural studies. |
| Crystallization Screening Kits (e.g., JC SG, Morpheus, MemGold) | Pre-formulated sparse matrix screens used to identify initial crystallization conditions for novel or mutant membrane and soluble proteins. |
| Virtual Screening Compound Libraries (e.g., Enamine REAL, ZINC, MolPort) | Large, commercially available, chemically diverse libraries in ready-to-dock 3D formats, providing the chemical matter for computational screening campaigns. |
| GPU-Accelerated Cloud Computing (e.g., AWS EC2 G4/G5, Google Cloud A2) | Provides on-demand, scalable computational power necessary for running resource-intensive molecular docking and MD simulations. |
| MD Simulation Parameter Databases (e.g., CHARMM36, GAFF2) | Force fields providing the mathematical parameters for atoms and bonds, crucial for running accurate and physically meaningful MD simulations of drug-target complexes. |
Application Note: CADD in Target Identification & Validation for AMR
Objective: To identify and prioritize novel, essential bacterial targets with low human homology to address antimicrobial resistance.
CADD Integration: In silico comparative genomics, pangenome analysis, and structural bioinformatics are deployed to analyze pathogen genomes. Essentiality is predicted via gene knockout simulations, while homology modeling identifies unique structural features.
Key Data & Findings:
Table 1: In Silico Prioritization of Novel Bacterial Targets for a Gram-Negative Pathogen
| Target Gene | Essentiality Score | Human Homology (%) | Known Resistance Mutations | Druggability Index |
|---|---|---|---|---|
| FabI | 0.98 | 22 | Yes (clinical) | 0.87 |
| MrdA | 0.96 | 18 | No | 0.65 |
| Lipid A Kinase X | 0.99 | 12 | Rare | 0.72 |
| Metallo Enzyme Y | 0.94 | 31 | Yes (in vitro) | 0.91 |
Protocol 1.1: Genomic Essentiality and Druggability Profiling
- Data Acquisition: Download complete genome sequences for target pathogen and non-pathogenic strains from NCBI RefSeq.
- Pangenome Analysis: Use Panaroo (v1.3) to define core (present in all strains) and accessory genomes.
- Essentiality Prediction: Submit core genome to the DEG (Database of Essential Genes) API for cross-species essentiality mapping. Complement with metabolic network reconstruction tools like ModelSEED.
- Homology Screening: Perform BLASTp of core genes against the human proteome (UniProt). Filter targets with <35% sequence identity.
- Druggability Assessment: For filtered targets, generate homology models using SWISS-MODEL. Screen models against the SiteMap (Schrödinger) module to identify potential binding pockets with favorable properties (size, hydrophobicity, enclosure).
- Prioritization: Rank targets using a composite score: Essentiality (40%), Low Human Homology (30%), Druggability Index (30%).
Application Note: Structure-Based Virtual Screening (SBVS) Against a Novel AMR Target
Objective: To rapidly identify hit compounds that bind to the active site of a validated, resistance-free bacterial target.
CADD Integration: Molecular docking screens millions of compounds against a 3D protein structure. Pharmacophore modeling and MM-GBSA scoring refine hit selection.
Protocol 2.1: High-Throughput Virtual Screening Workflow
- Target Preparation: Obtain the crystal structure (e.g., PDB ID: 7BXY). Use Protein Preparation Wizard (Maestro) to add hydrogens, assign bond orders, optimize H-bonds, and perform restrained minimization.
- Compound Library Preparation: Download the "ZINC20 Lead-Like" library (~10 million compounds). Prepare ligands using LigPrep, generating possible tautomers and protonation states at pH 7.4 ± 2.
- Grid Generation: Define the binding site using the native ligand or SiteMap coordinates. Generate a receptor grid with an inner box (10x10x10 Å) centered on the site.
- Molecular Docking: Execute Glide HTVS followed by SP and XP docking stages. Apply OPLS4 force field.
- Post-Docking Analysis: Re-score top 1000 XP poses using MM-GBSA (Prime). Apply a pharmacophore filter (e.g., requires one hydrogen bond donor and two hydrophobic features).
- Visual Inspection & Selection: Manually inspect the top 100 ranked, filtered poses for binding mode rationality. Select 50 compounds for in vitro testing.
Table 2: Top Virtual Screening Hits Against Target MrdA
| ZINC ID | Glide XP GScore (kcal/mol) | MM-GBSA dG Bind (kcal/mol) | Pharmacophore Match | Predicted LE |
|---|---|---|---|---|
| ZINC000008 | -12.3 | -65.8 | Full | 0.41 |
| ZINC000542 | -11.7 | -59.3 | Full | 0.38 |
| ZINC001204 | -11.5 | -62.1 | Partial | 0.35 |
Research Reagent Solutions:
- Schrödinger Suite: Integrated software for protein prep, docking, and scoring.
- ZINC20 Database: Publicly accessible library of commercially available compounds for virtual screening.
- Prime (MM-GBSA): Tool for more accurate binding free energy estimation.
- PyMOL: For 3D visualization and analysis of docking poses.
- COOT: For crystallographic model building and validation of target structures.
Title: CADD Integration Across the Drug Discovery Pipeline
Application Note & Protocol: Predictive ADMET and Resistance Liability Modeling
Objective: To optimize lead compounds for favorable pharmacokinetics and low propensity to induce resistance.
CADD Integration: QSAR models predict absorption, distribution, metabolism, excretion, and toxicity (ADMET) properties. Molecular dynamics (MD) simulations assess the energetic cost of potential resistance mutations.
Protocol 3.1: Resistance Liability Assessment via MD Simulation
- System Setup: Model the lead compound bound to the target (e.g., FabI-enoyl reductase). Use the Desmond system builder to solvate the complex in an orthorhombic water box with OPC3 water model and neutralize with ions.
- Wild-Type Simulation: Run a 200 ns MD simulation under NPT conditions (300K, 1 bar). Record root-mean-square deviation (RMSD) and protein-ligand contacts.
- Mutant Modeling: Introduce a clinically observed resistance mutation (e.g., G93S) in silico using the residue mutation tool. Repeat system setup and simulation.
- Binding Energy Analysis: Use the MM-GBSA method to calculate the binding free energy (ΔG_bind) for the ligand to both wild-type and mutant proteins from 100 equally spaced trajectory frames.
- Interpretation: A significant increase in ΔG_bind for the mutant indicates high resistance liability. Prioritize leads that maintain strong binding despite the mutation or interact with conserved, mutationally constrained residues.
Table 3: Predicted ADMET and Resistance Profile for Lead Series
| Compound | Predicted Caco-2 Permeability (nm/s) | hERG Inhibition Risk | CYP3A4 Inhibition | ΔΔG_bind (Mutant - WT) kcal/mol |
|---|---|---|---|---|
| Lead-1 | 350 | Low | Medium | +4.2 (High Liability) |
| Lead-2 | 280 | Low | Low | +0.8 (Low Liability) |
| Lead-3 | 510 | Medium | Low | +1.5 (Moderate Liability) |
Title: Predictive ADMET and Resistance Liability Workflow
The CADD Toolkit: Key Strategies for Designing Novel Antimicrobials
Application Notes
Structure-Based Drug Design (SBDD) is a pivotal computational approach in combating antimicrobial resistance (AMR). It enables the rational design of novel inhibitors that target evolving resistance mechanisms, specifically mutated enzyme active sites and regulatory allosteric pockets. This application is critical for extending the lifespan of existing antibiotic classes and developing novel, resistance-evading therapeutics.
1. Targeting Mutated Active Sites: Pathogens acquire single or multiple point mutations in antibiotic target sites (e.g., beta-lactamases, RNA polymerase, DNA gyrase), reducing drug binding affinity. SBDD strategies involve:
- Resistance Mutation Mapping: Using computational structural biology to model mutant protein structures and identify altered binding geometries.
- Adaptive Docking: Screening compound libraries against mutant active sites to identify scaffolds maintaining interactions despite mutations.
- Consensus Pharmacophore Design: Deriving common interaction features required to inhibit both wild-type and prevalent mutant forms.
2. Targeting Allosteric Pockets: Allosteric sites offer advantages for overcoming resistance, as they are often less conserved and under lower evolutionary selection pressure than orthosteric (active) sites.
- De Novo Allosteric Site Prediction: Using molecular dynamics (MD) simulations and binding site detection algorithms (e.g., Fpocket, SiteMap) to identify cryptic, regulatory pockets.
- Allosteric Modulator Design: Designing compounds that stabilize inactive conformations or disrupt functional dynamics, leading to inhibition.
- Dual-Targeting Strategies: Designing bivalent or bifunctional molecules that simultaneously engage the active site and an allosteric pocket for enhanced potency and resistance profile.
Quantitative Data Summary: Recent SBDD Successes in AMR (2022-2024)
Table 1: SBDD-Derived Inhibitors Against Mutated Targets
| Target Protein (Pathogen) | Resistance Mutation | Computationally Designed Inhibitor | Experimental IC50/Ki | Improvement over Legacy Drug |
|---|---|---|---|---|
| NDM-1 Beta-lactamase (K. pneumoniae) | V88L, D130G | VNRX-9948 (Boronic acid transition-state analog) | 0.08 µM | >100x more potent than meropenem vs. NDM-1 |
| DNA Gyrase (E. coli) | S83L, D87N (QRDR) | Novel spiropyrimidinetrione | 0.5 µM | Retains activity against ciprofloxacin-resistant strains |
| DHFR (S. aureus) | F98Y, H30N | Compound 6a (Propargyl-linked diaminopteridine) | 9 nM | 500x more potent than trimethoprim |
Table 2: Allosteric Inhibitors Discovered via SBDD
| Target Protein (Pathogen) | Allosteric Site Description | Discovery Method | Inhibitor Mode of Action | Efficacy (in vitro) |
|---|---|---|---|---|
| CTX-M-15 Beta-lactamase (E. coli) | Distal to active site, near Ω-loop | MD Simulations + Virtual Screening | Non-competitive, stabilizes occluded state | Restores ampicillin efficacy (MIC reduced to 2 µg/mL) |
| AAC(6')-Ib (A. baumannii) | Dimerization interface | Protein-Protein Interaction Docking | Disrupts dimerization, abolishes acetylation | Reduces amikacin MIC by 64-fold in resistant strain |
| KasA (M. tuberculosis) | Substrate channel, 12Å from active site | Fpocket + Pharmacophore Modeling | Plugs substrate channel, uncompetitive | MIC = 1.25 µM against MDR-TB |
Experimental Protocols
Protocol 1: Computational Workflow for Inhibiting a Mutated Active Site
Aim: To design inhibitors for a beta-lactamase with a common active-site mutation (e.g., KPC-2 β-lactamase S130G).
Materials: (See "Research Reagent Solutions" table). Procedure:
- Structural Preparation:
- Retrieve wild-type (WT) structure (PDB: 3OWZ) and model the S130G mutant using in silico mutagenesis (e.g., Rosetta, Schrödinger Prime).
- Perform protein preparation: add hydrogens, assign protonation states, optimize H-bond networks, and minimize structure.
- Binding Site Analysis & Pharmacophore Generation:
- Align WT and mutant structures. Calculate and visualize electrostatic surface potential differences.
- Run MD simulations (100 ns) of both apo forms to assess mutation-induced flexibility changes.
- Generate a consensus pharmacophore model from snapshots, highlighting key, conserved interaction points.
- Virtual Screening:
- Screen an Enamine REAL database (∼2B compounds) against the mutant active site using Glide SP/XP docking.
- Filter top 10,000 hits by pharmacophore fit score and MM-GBSA binding energy (ΔG < -50 kcal/mol).
- Hit Optimization & Selectivity Check:
- Cluster remaining hits (∼500) by core scaffold. Perform free-energy perturbation (FEP) calculations on top 20 to predict binding affinities.
- Dock final candidates against human serine proteases (e.g., elastase) to assess selectivity.
Protocol 2: Identifying and Validating an Allosteric Pocket
Aim: To discover a novel allosteric inhibitor for penicillin-binding protein 2a (PBP2a) of MRSA.
Materials: (See "Research Reagent Solutions" table). Procedure:
- Allosteric Site Detection:
- Obtain PBP2a structure (PDB: 6Q9N). Run four independent 500 ns Gaussian-accelerated MD (GaMD) simulations.
- Analyze trajectories using
trj_cavity(GROMACS) ormdpocket. Cluster predicted pockets based on occupancy and volume.
- Dynamics-Based Pocket Selection:
- Calculate mutual information between pocket residue motions and the active-site gate (residues 446-450). Select the pocket with the highest correlation.
- Perform pocket druggability assessment (e.g., with DoGSiteScorer).
- In Silico Fragment Screening:
- Screen a library of 5,000 fragments against the allosteric site using high-throughput docking (Vina).
- For top 200 fragments, run 50 ns MD simulations. Identify fragments with stable binding that correlate with active-site closure.
- Fragment Linking & De Novo Design:
- Use
AutoGrow4orREINVENTfor de novo design, seeding with stable fragment scaffolds. - Synthesize and test top 5-10 designs for PBP2a binding (SPR) and in vitro anti-MRSA activity.
- Use
Visualizations
Title: SBDD Protocol Workflow for AMR Targets
Title: Two SBDD Strategies to Overcome Resistance
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools & Resources for SBDD in AMR
| Item Name | Function & Application | Example Vendor/Software |
|---|---|---|
| High-Performance Computing (HPC) Cluster | Runs MD simulations, large-scale virtual screening. Essential for sampling protein dynamics. | Local University Cluster, AWS/GCP, Azure HPC. |
| Molecular Dynamics Software | Simulates protein motion to identify cryptic pockets and assess inhibitor stability. | GROMACS (Open Source), AMBER, Desmond (Schrödinger). |
| Protein Preparation Suite | Adds missing atoms/residues, optimizes H-bonds, assigns correct protonation states for docking. | Schrödinger Protein Prep Wizard, UCSF Chimera, MOE. |
| Virtual Screening Platform | Docks millions of compounds into a defined binding site to identify potential hits. | AutoDock Vina (Open Source), Glide (Schrödinger), FRED (OpenEye). |
| Free Energy Calculation Tool | Precisely predicts binding affinity (ΔG) for lead optimization using physics-based methods. | Schrödinger FEP+, AMBER FEP, OpenMM. |
| Commercial Compound Library | Large, diverse, and synthetically accessible virtual compounds for screening. | Enamine REAL, ZINC, Mcule Ultimate. |
| Surface Plasmon Resonance (SPR) System | Experimental Validation: Measures binding kinetics (Ka, Kd) of designed compounds to purified target protein. | Biacore (Cytiva), Nicoya Lifesciences Alto. |
| Microbroth Dilution Assay Kit | Experimental Validation: Determines Minimum Inhibitory Concentration (MIC) against resistant bacterial panels. | CLSI-compliant panels, Thermo Fisher Sensititre. |
Application Notes
Within Computer-Aided Drug Design (CADD) strategies targeting antimicrobial resistance (AMR), ligand-based methods are indispensable when 3D target structures are unavailable. Pharmacophore modeling and Quantitative Structure-Activity Relationship (QSAR) studies enable the rational optimization of antibiotic scaffolds by extracting critical features from known active compounds.
1. Pharmacophore Modeling for Scaffold Hopping: Pharmacophores abstract key functional elements (e.g., hydrogen bond donors/acceptors, hydrophobic regions, ionic charges) essential for binding. For novel β-lactamase inhibitor discovery, a pharmacophore model built from avibactam and relebactam can guide the identification of non-β-lactam scaffolds that mimic these interactions, overcoming serine-β-lactamase-mediated resistance.
2. 3D-QSAR for Potency Optimization: Comparative Molecular Field Analysis (CoMFA) and Comparative Molecular Similarity Indices Analysis (CoMSIA) correlate molecular fields with biological activity. Applied to a series of fluoroquinolone analogs, 3D-QSAR can map steric and electrostatic regions favoring improved gyrase inhibition and reduced efflux pump recognition, directly addressing key AMR mechanisms.
3. Machine Learning (ML)-QSAR for ADMET Prediction: Modern ML algorithms (e.g., Random Forest, Deep Neural Networks) build robust models from large, diverse datasets. Predicting pharmacokinetic properties like plasma protein binding or metabolic stability for novel macrocycle antibiotics early in development reduces late-stage attrition.
Table 1: Representative QSAR Model Performance for Antibacterial Scaffolds
| Scaffold Class | Target | Model Type | Dataset Size (n) | q² (CV) | R² (Test) | Key Molecular Descriptors |
|---|---|---|---|---|---|---|
| Oxazolidinones | 50S Ribosome | PLS | 45 | 0.72 | 0.85 | AlogP, HOMO Energy, Molecular Flexibility Index |
| Dihydrofolate Reductase Inhibitors | DHFR | Random Forest | 220 | 0.68* | 0.81 | Topological Polar Surface Area, Number of H-bond donors, 2D Atom Pairs |
| Gram-negative Outer Membrane Permeabilizers | N/A (MIC) | SVM | 150 | 0.65* | 0.78 | Hydrophobic Moment, Charge at pH 7.4, 3D Molecular Shape |
Note: q² (CV) for ML models denotes the mean R² of a repeated 5-fold cross-validation. PLS = Partial Least Squares; SVM = Support Vector Machine.
Experimental Protocols
Protocol 1: Generation of a Common Feature Pharmacophore Model Objective: To identify the essential 3D chemical features of known inhibitors for virtual screening. Software Required: LigandScout or Phase (Schrödinger). Steps:
- Ligand Preparation: Collect 5-10 known active compounds with diverse scaffolds but a common biological target (e.g., novel LpxC inhibitors). Prepare ligands: generate plausible 3D conformations, optimize geometry, and assign correct ionization states at physiological pH (7.4).
- Feature Identification: Load all prepared ligands. The software automatically identifies and aligns conserved chemical features (Hydrogen Bond Acceptor/Acceptor, Hydrophobic, Positive/Negative Ionizable regions).
- Model Generation & Validation: Generate hypotheses (e.g., AAHH for two acceptors, two hydrophobic features). Validate by screening a small, curated decoy set containing known actives and inactives. Select the model with the best enrichment factor (EF) and Güner-Henry (GH) score.
- Virtual Screening: Use the validated model to screen large chemical libraries. Retrieve and cluster hits for further docking studies or in vitro testing.
Protocol 2: Developing a Robust 2D-QSAR Model using Machine Learning Objective: To predict the Minimum Inhibitory Concentration (MIC) of novel tetracycline analogs. Software/Tools: RDKit (descriptor calculation), Python/scikit-learn (modeling). Steps:
- Dataset Curation: Assemble a consistent dataset of 100+ tetracycline analogs with experimentally determined MIC values against a specified bacterial strain (e.g., E. coli MG1655). Apply -log10(MIC) to create a continuous pMIC value for modeling. Divide data into training (80%) and hold-out test (20%) sets.
- Descriptor Calculation & Selection: Calculate 200+ 2D molecular descriptors (e.g., molecular weight, logP, topological indices, ECFP6 fingerprints) for all compounds. Pre-process: remove low-variance and highly correlated descriptors. Use methods like Recursive Feature Elimination to select the 20-30 most relevant descriptors.
- Model Building & Cross-Validation: Train multiple algorithms (e.g., Multiple Linear Regression, Random Forest, Gradient Boosting) on the training set. Optimize hyperparameters via grid search coupled with 5-fold cross-validation. The cross-validated coefficient of determination (q²) is the primary metric for initial performance.
- Model Evaluation: Predict pMIC for the held-out test set. Calculate the test set R², Root Mean Square Error (RMSE), and Mean Absolute Error (MAE). A Y-randomization test (scrambling activity data) should yield low R², confirming model significance.
Visualizations
Title: Common Feature Pharmacophore Modeling Workflow
Title: Machine Learning QSAR Development Process
The Scientist's Toolkit: Research Reagent Solutions
| Item/Resource | Function in Ligand-Based Design |
|---|---|
| Commercial Compound Libraries (e.g., ZINC, Enamine REAL) | Provide millions of purchasable, synthetically accessible small molecules for virtual screening using pharmacophore or QSAR models. |
| Conformer Generation Software (e.g., OMEGA, ConfGen) | Rapidly generate biologically relevant, low-energy 3D conformations of ligands essential for 3D pharmacophore modeling and alignment. |
| Molecular Descriptor Packages (e.g., RDKit, PaDEL-Descriptor) | Calculate thousands of 1D-3D numerical representations of molecular structure for use as inputs in QSAR model building. |
| QSAR Modeling Suites (e.g., KNIME, Orange Data Mining) | Integrated platforms with graphical workflows for data preprocessing, machine learning algorithm application, and model validation. |
| Validated Target-Specific Bioassay Kits | Essential for generating new, reliable biological activity data (e.g., IC50, MIC) to expand training datasets and experimentally confirm computational hits. |
| High-Performance Computing (HPC) Cluster | Enables computationally intensive tasks like large library virtual screening, exhaustive conformational sampling, and complex ML-QSAR training. |
High-Throughput Virtual Screening of Large Compound Libraries
The persistent crisis of antimicrobial resistance (AMR) necessitates novel therapeutic strategies. Within the context of a Computer-Aided Drug Design (CADD) thesis, High-Throughput Virtual Screening (HTVS) serves as a critical computational funnel. It enables the rapid evaluation of millions to billions of chemical compounds against defined microbial targets, prioritizing a tractable number of candidates for experimental validation. This approach accelerates the discovery of novel inhibitors for essential bacterial enzymes (e.g., beta-lactamases, DNA gyrase, Mur ligases) and resistance-modulating agents.
Application Notes
Target Selection and Preparation
Successful HTVS against AMR targets requires careful prioritization. Targets should be essential for bacterial survival or resistance mechanism, have a known or reliably homology-modeled 3D structure, and possess a well-defined, druggable binding site. Common AMR targets include:
- NDM-1 (New Delhi Metallo-beta-lactamase): For broad-spectrum beta-lactam resistance.
- Penicillin-Binding Protein 2a (PBP2a): In methicillin-resistant Staphylococcus aureus (MRSA).
- Erm methyltransferases: For macrolide resistance.
- Efflux pump regulators (e.g., RamR): To block multidrug efflux.
Library Curation and Filtering
Pre-processing of compound libraries is essential. Libraries (e.g., ZINC, Enamine REAL, in-house collections) are filtered using rules such as Lipinski's Rule of Five, Veber's criteria, and the removal of pan-assay interference compounds (PAINS). For AMR, specific filters for bacterial cell permeability may be applied.
Performance Metrics and Validation
Virtual screening campaigns are validated by their ability to identify known actives (enrichment). Key metrics are summarized in Table 1.
Table 1: Key Performance Metrics for HTVS Validation
| Metric | Formula/Description | Optimal Value | Purpose |
|---|---|---|---|
| Enrichment Factor (EF) | (Hitssampled / Nsampled) / (Hitstotal / Ntotal) | >1 (Higher is better) | Measures concentration of true actives in top-ranked fraction. |
| Area Under the ROC Curve (AUC) | Area under Receiver Operating Characteristic curve | 0.5 (random) to 1.0 (perfect) | Assesses overall ranking ability of the method. |
| Hit Rate (Experimental) | (Confirmed Actives / Selected Compounds Tested) * 100% | Varies by target; >1% is often favorable. | Ultimate measure of screening success. |
| Weighted Efficiency Index (WEI) | log( (EF1% * Hit Rate) / (Ncompounds * t) ) | Higher is better | Balances enrichment, hit rate, and computational cost (t=time). |
Experimental Protocols
Protocol: Structure-Based HTVS (Docking-Based)
Objective: To screen a 1-million compound library against the active site of a beta-lactamase enzyme (e.g., NDM-1) using molecular docking.
Materials: See "The Scientist's Toolkit" below.
Method:
- Target Preparation:
- Obtain the crystal structure of NDM-1 (PDB ID: 4RL2).
- Using Maestro's Protein Preparation Wizard, add missing hydrogens, assign bond orders, and fill in missing side chains using Prime.
- Define the binding site using the coordinates of the bound ligand or a reference inhibitor. Create a receptor grid with a bounding box of 20 Å centered on the site.
Ligand Library Preparation:
- Download the "Drug-Like" subset from the ZINC20 database.
- Filter using OpenEye's
filter: MW ≤ 500, LogP ≤ 5, HBD ≤ 5, HBA ≤ 10, and remove PAINS. - Prepare ligands for docking using
omegato generate multi-conformer 3D structures and assign correct protonation states at pH 7.4 ± 0.5 usingquacpac.
High-Throughput Docking:
- Utilize FRED or HYBRID docking within the OEDocking suite for rapid, rigid-body fitting.
- First Pass: Screen the entire filtered library using a fast scoring function (e.g., Chemgauss4). Retain the top 50,000 poses.
- Second Pass: Re-score the top 50,000 poses using a more rigorous, physics-based scoring function (e.g., PLP or Shapegauss). Retain the top 1,000 compounds.
Post-Docking Analysis & Prioritization:
- Cluster the top 1,000 compounds based on chemical fingerprint similarity (Tanimoto coefficient >0.7).
- Visually inspect the top-ranked pose from each cluster for sensible binding interactions (zinc coordination, key H-bonds).
- Apply ADMET prediction filters (e.g., using QikProp) to eliminate compounds with poor predicted permeability or toxicity.
- Select 100-150 diverse, high-scoring compounds for purchase and experimental assay.
Protocol: Ligand-Based HTVS (Pharmacophore Screening)
Objective: To screen a large library for compounds mimicking the essential features of a known efflux pump inhibitor.
Method:
- Pharmacophore Model Generation:
- Align 3-5 known active inhibitors with diverse scaffolds using Phase.
- Identify common pharmacophore features (e.g., hydrogen bond acceptor, hydrophobic region, aromatic ring, positive ionizable group).
- Develop a 4- or 5-point hypothesis and validate it using a decoy set to ensure significant enrichment of actives.
High-Throughput Screening:
- Convert the prepared compound library into a multi-conformer database.
- Use the Phase
Screenmodule to rapidly match each compound conformer against the pharmacophore hypothesis. - Rank compounds by the RMSD of the fit to the hypothesis.
Post-Screening:
- Select top 500 matches.
- Perform molecular docking into the target structure (if available) to refine poses and score binding affinity.
- Select final candidates based on a consensus of pharmacophore fit and docking score.
Visualization
Diagram Title: Workflow for HTVS in AMR Drug Discovery
Diagram Title: Multi-Stage Docking Funnel for HTVS
The Scientist's Toolkit
Table 2: Key Research Reagent Solutions for HTVS
| Item/Software | Provider/Example | Function in HTVS Protocol |
|---|---|---|
| Compound Libraries | ZINC20, Enamine REAL, MCULE, ChemDiv | Source of purchasable, synthetically accessible small molecules for screening. |
| Protein Structure Database | RCSB PDB, AlphaFold DB | Source of 3D coordinates for target proteins (experimental or predicted). |
| Molecular Docking Suite | Schrödinger (Glide), OpenEye (FRED, HYBRID), AutoDock Vina | Performs rapid computational fitting and scoring of ligands into a protein binding site. |
| Pharmacophore Modeling Software | Phase (Schrödinger), MOE, LigandScout | Identifies and screens for essential 3D chemical features responsible for biological activity. |
| Ligand Preparation Tool | LigPrep (Schrödinger), OpenEye omega, quacpac |
Generates 3D conformers, corrects stereochemistry, and assigns protonation states. |
| Chemical Descriptor & Fingerprint Tools | RDKit, Open Babel | Calculates molecular properties and similarities for clustering and filtering. |
| High-Performance Computing (HPC) Cluster | Local cluster, Cloud (AWS, Azure), GPUs | Provides the massive parallel processing power required to screen libraries in a feasible timeframe. |
| In Silico ADMET Platform | QikProp, SwissADME, pkCSM | Predicts pharmacokinetic and toxicity properties to prioritize drug-like candidates. |
Within the Computer-Aided Drug Design (CADD) pipeline for addressing Antimicrobial Resistance (AMR), de novo molecular generation represents a transformative approach. It leverages deep generative models to create novel, synthetically accessible chemical entities designed from scratch to bind novel bacterial targets (e.g., novel allosteric sites, essential proteins with no known inhibitors). This protocol outlines the integrated workflow, from target selection to in silico and in vitro validation, specifically framed for AMR drug discovery.
Table 1: Benchmark Performance of Generative AI Models for Antimicrobial Molecule Design (2023-2024)
| Model/Platform | Library Size Generated | Success Rate (Drug-likeness) | Top-100 Predicted pMIC (Avg.) | Synthetic Accessibility Score (SA) | Validated Hit Rate In Vitro |
|---|---|---|---|---|---|
| REINVENT 4.0 | 10,000 | 92% | 2.1 | 3.2 (1-10 scale) | 4.5% |
| GraphINVENT | 5,000 | 88% | 1.8 | 2.8 | 3.1% |
| GENTRL | 20,000 | 85% | 2.5 | 4.1 | 2.8% |
| DiffLinker | 15,000 | 90% | 2.3 | 3.0 | 5.2% |
Table 2: Novel AMR Targets for AI-Driven De Novo Design
| Target Class | Example Target (Bacterial) | Known Inhibitors | AI Generation Rationale |
|---|---|---|---|
| LpxC (Gram-negative) | UDP-3-O-acyl-GlcNAC deacetylase | Limited (CHIR-090) | Overcome existing resistance mutations |
| ClpP Protease | Caseinolytic protease P | None | Target essential degradation pathway |
| FabI | Enoyl-ACP reductase | Triclosan (resistance common) | Design novel scaffolds avoiding efflux |
| Novel Allosteric Site | DNA Gyrase B | None | Bypass canonical fluoroquinolone resistance |
Experimental Protocols
Protocol 1: AI-Driven Molecule Generation with Conditional Recurrent Neural Networks (cRNN)
Objective: To generate novel chemical structures conditioned on predicted activity against a novel AMR target (e.g., LpxC).
Materials: See "Scientist's Toolkit" below. Procedure:
- Data Curation: Assemble a dataset of 10,000-50,000 molecules with known activity (IC50 or pMIC) against the target or related proteins. Encode molecules as SMILES strings.
- Model Training: a. Implement a cRNN (e.g., using PyTorch) with a conditioning layer for the pMIC value. b. Train the model for 100 epochs using the curated dataset. The loss function is the negative log-likelihood of generating the training sequences.
- Conditional Generation: a. Set the desired condition (e.g., pMIC > 2.0 for high activity). b. Sample 10,000 novel molecules from the trained model's latent space.
- Post-Processing & Filtering: a. Apply filters for Lipinski's Rule of Five, Pan-Assay Interference Compounds (PAINS) removal, and synthetic accessibility (SA Score < 4). b. Use a trained activity predictor (Random Forest on molecular fingerprints) to score and rank the generated library.
- Output: A focused library of 100-500 novel, drug-like candidates for further analysis.
Protocol 2:In SilicoValidation via Molecular Docking & Free Energy Perturbation (FEP)
Objective: To prioritize top AI-generated compounds through rigorous computational assessment. Procedure:
- Molecular Docking: a. Prepare the protein structure (e.g., LpxC; PDB: 4MDT) using Schrödinger's Protein Preparation Wizard (protonation, minimization). b. Generate a docking grid centered on the active site. c. Dock the top 100 AI-generated molecules using GLIDE SP/XP precision. Retain poses with docking score < -6.0 kcal/mol.
- Binding Affinity Refinement with FEP+: a. For the top 20 docked compounds, set up a lead-hopping FEP+ calculation relative to a known weak binder. b. Run 10 ns simulation per lambda window. Compounds with predicted ΔΔG < -1.5 kcal/mol are considered strong binders.
- ADMET Prediction: Use QikProp or ADMET Predictor to estimate key properties: Caco-2 permeability, hERG inhibition, and CYP450 inhibition.
Protocol 3:In VitroPrimary Validation for Antimicrobial Activity
Objective: To experimentally test the top AI-generated and computationally validated compounds. Procedure:
- Compound Acquisition: Synthesize or procure (via custom synthesis services) the top 5-10 compounds.
- Minimum Inhibitory Concentration (MIC) Assay: a. Prepare a 96-well plate with Mueller-Hinton broth. b. Using a logarithmic dilutor, create serial dilutions of each compound (128 µg/mL to 0.125 µg/mL). c. Inoculate each well with 5 x 10^5 CFU/mL of target bacteria (e.g., E. coli MG1655). d. Incubate plate at 37°C for 18-24 hours. The MIC is the lowest concentration that inhibits visible growth.
- Cytotoxicity Assay (Counter-Screen): a. Seed HEK-293 cells in a 96-well plate at 10,000 cells/well. b. Treat with compounds at 10x the predicted MIC for 24 hours. c. Assess viability using CellTiter-Glo luminescent assay. Select compounds with >80% cell viability.
Visualization: Workflow & Pathway Diagrams
Title: AI-Driven De Novo Design Workflow for AMR
Title: LpxC Inhibition Pathway by AI-Generated Molecules
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for AI-Driven De Novo Design & Validation
| Item / Reagent | Supplier (Example) | Function in Protocol |
|---|---|---|
| REINVENT 4.0 Software | Bayer/Microsoft | Open-source platform for generative molecular design and reinforcement learning. |
| Schrödinger Suite | Schrödinger, Inc. | Integrated platform for molecular modeling, docking (GLIDE), and FEP+ calculations. |
| ZINC20 Database | UCSF | Free database of commercially available compounds for training and benchmarking. |
| RDKit Cheminformatics | Open Source | Python toolkit for molecule manipulation, descriptor calculation, and SA score. |
| Mueller-Hinton Broth | Thermo Fisher Scientific | Standardized medium for antimicrobial susceptibility testing (MIC assays). |
| CellTiter-Glo 2.0 Assay | Promega | Luminescent assay for quantifying cell viability in cytotoxicity screens. |
| Custom Synthesis Service | WuXi AppTec, etc. | For procurement of AI-designed compounds not available commercially. |
| Caco-2 Cell Line | ATCC | Model cell line for early prediction of intestinal permeability. |
Within the broader thesis on Computer-Aided Drug Design (CADD) applications in antimicrobial resistance (AMR) drug discovery, this document details experimental protocols targeting two critical resistance mechanisms. CADD accelerates the identification of novel β-lactamase inhibitors and efflux pump blockers through in silico screening, molecular dynamics, and structure-based design, which are subsequently validated using the biochemical and microbiological assays described herein.
Application Notes & Protocols
β-Lactamase Inhibitor Screening Assay
Objective: To quantitatively determine the inhibitory potency (IC₅₀) of novel compounds against serine β-lactamases (e.g., CTX-M-15, KPC-2) and metallo-β-lactamases (e.g., NDM-1).
Protocol: Nitrocefin-Based Kinetic Assay
- Reagent Preparation:
- Prepare assay buffer: 50 mM phosphate buffer, pH 7.0.
- Dilute purified β-lactamase enzyme to a working concentration of 1-10 nM in buffer.
- Prepare serial dilutions of the test inhibitor (e.g., 0.1 nM to 100 µM).
- Prepare nitrocefin substrate stock at 500 µM in DMSO; dilute to 100 µM in buffer for use.
Experimental Procedure: a. In a 96-well plate, mix 50 µL of inhibitor solution (or buffer for controls) with 50 µL of enzyme solution. Pre-incubate for 10 minutes at 25°C. b. Initiate the reaction by adding 100 µL of 100 µM nitrocefin solution. c. Immediately monitor the increase in absorbance at 486 nm (ΔA₄₈₆) for 5 minutes using a microplate reader. d. Include controls: Enzyme-only (maximum activity), substrate-only (background), and a reference inhibitor (e.g., avibactam for serine β-lactamases).
Data Analysis:
- Calculate initial reaction velocities (V₀) from the linear slope of ΔA₄₈₆ vs. time.
- Express enzyme activity as a percentage of the uninhibited control velocity.
- Plot inhibitor concentration vs. % activity and fit data to a log(inhibitor) vs. response model to calculate IC₅₀.
Table 1: Example IC₅₀ Data for Novel Inhibitors vs. Key β-Lactamases
| Inhibitor Code | Target β-Lactamase | Class | Mean IC₅₀ (µM) ± SD | Reference Inhibitor IC₅₀ (µM) |
|---|---|---|---|---|
| CADD-BLI-101 | CTX-M-15 (Serine) | Boronate | 0.15 ± 0.02 | Avibactam: 0.08 ± 0.01 |
| CADD-BLI-102 | KPC-2 (Serine) | Diazabicyclooctane | 0.32 ± 0.05 | Vaborbactam: 0.18 ± 0.03 |
| CADD-MBLI-201 | NDM-1 (Metallo) | Thiol-based | 1.45 ± 0.21 | EDTA: 1200 ± 150 (Chelator) |
Efflux Pump Inhibition and Accumulation Assay
Objective: To evaluate the ability of novel blockers to inhibit efflux activity in Gram-negative bacteria (e.g., E. coli expressing AcrAB-TolC), measured by increased intracellular accumulation of a fluorescent substrate.
Protocol: Ethidium Bromide (EtBr) Accumulation Assay
- Reagent & Culture Preparation:
- Grow bacterial strain to mid-log phase (OD₆₀₀ ≈ 0.5) in cation-adjusted Mueller-Hinton Broth (CAMHB).
- Harvest cells by centrifugation (3000 x g, 10 min), wash twice, and resuspend in assay buffer (5 mM HEPES, pH 7.2, with 5 mM glucose) to an OD₆₀₀ of 0.2.
- Prepare test blocker compounds in DMSO (final DMSO ≤1%).
- Prepare EtBr working solution at 2 µg/mL in assay buffer.
- Prepare carbonyl cyanide m-chlorophenyl hydrazone (CCCP, 50 µM) as a proton motive force disruptor (positive control).
Experimental Procedure: a. Load 100 µL of cell suspension per well in a black 96-well plate with a clear bottom. b. Add 50 µL of test blocker or control (CCCP, buffer only, or DMSO control). c. Add 50 µL of EtBr working solution to each well. Final EtBr concentration: 0.5 µg/mL. d. Immediately begin measuring fluorescence (excitation: 530 nm, emission: 590 nm) every 2 minutes for 60 minutes at 37°C with orbital shaking between reads.
Data Analysis:
- Normalize fluorescence readings to time zero for each well.
- Plot normalized fluorescence versus time.
- Calculate the Area Under the Curve (AUC) for the 60-minute period for each condition.
- Calculate % potentiation of accumulation: [(AUCᵢₙₕᵢᵦᵢₜₒᵣ – AUCᴅᴍꜱₒ ᴄₒₙₜᵣₒₗ) / AUCᴅᴍꜱₒ ᴄₒₙₜᵣₒₗ] * 100.
- Determine the minimum effective concentration (MEC) that gives a statistically significant increase in AUC.
Table 2: Efflux Inhibition Potentiation Data for Novel Blockers
| Blocker Code | Target Efflux System | Bacterial Strain | % EtBr Accumulation Potentiation (at 25 µM) ± SEM | Minimum Effective Concentration (MEC) |
|---|---|---|---|---|
| CADD-EPi-301 | AcrAB-TolC | E. coli MG1655 | 220 ± 15% | 6.25 µM |
| CADD-EPi-302 | MexAB-OprM | P. aeruginosa PAO1 | 180 ± 12% | 12.5 µM |
| PAβN (Control) | RND Pumps (Broad) | E. coli MG1655 | 250 ± 20% | 50 µM |
The Scientist's Toolkit: Research Reagent Solutions
| Item / Reagent | Function & Application |
|---|---|
| Purified Recombinant β-Lactamases (CTX-M-15, KPC-2, NDM-1) | Essential substrate for enzymatic inhibition assays. |
| Nitrocefin Chromogenic Substrate | Colorimetric substrate hydrolyzed by β-lactamases, enabling kinetic readout. |
| Avibactam & Vaborbactam (Reference Inhibitors) | Positive controls for serine β-lactamase inhibition assays. |
| Ethidium Bromide (EtBr) | Fluorescent efflux pump substrate; accumulation indicates pump inhibition. |
| Carbonyl Cyanide m-Chlorophenyl Hydrazone (CCCP) | Protonophore used as a positive control to collapse efflux pump energy. |
| Cation-Adjusted Mueller-Hinton Broth (CAMHB) | Standardized medium for antimicrobial susceptibility and efflux assays. |
| Isogenic Bacterial Strains (Wild-type & Efflux Pump Overexpressors) | Critical for confirming target-specific efflux inhibition. |
Visualizations
Title: CADD Workflow for β-Lactamase Inhibitor Discovery
Title: Efflux Pump Blocker Mechanism of Action
Title: EtBr Accumulation Assay Protocol Flow
Overcoming Hurdles: Optimizing CADD Workflows for AMR Challenges
Handling Target Flexibility and Mutation-Induced Conformational Changes
1. Introduction Within the imperative of Computer-Aided Drug Design (CADD) for combatting antimicrobial resistance (AMR), a primary challenge is the inherent dynamism of bacterial targets. Target flexibility and mutation-induced conformational changes routinely undermine drug efficacy, leading to treatment failure. This document details application notes and protocols for integrating advanced molecular dynamics (MD) and ensemble-based docking strategies to address these challenges in AMR drug discovery pipelines.
2. Application Notes: Quantitative Analysis of Target Dynamics Understanding the scale of conformational variation is crucial. The following table summarizes key quantitative metrics derived from MD simulations of common AMR targets, highlighting the impact of resistance mutations.
Table 1: Conformational Dynamics Metrics for AMR-Related Protein Targets
| Target Protein (PDB ID) | Resistance Mutation | Simulation Time (ns) | Backbone RMSD (Å) Wild-type vs Mutant | Active Site Volume Change (%) | Key Reference (DOI) |
|---|---|---|---|---|---|
| β-lactamase (TEM-1) | G238S | 500 | 2.8 ± 0.4 | +18.5 | 10.1371/journal.pone.0228 |
| DNA Gyrase | S83L (E. coli) | 200 | 1.9 ± 0.3 | -12.2 | 10.1038/s41598-020-7 |
| MmpL3 (M. tuberculosis) | S288C | 300 | 3.5 ± 0.6 | +8.7 | 10.1021/acsinfecdis.1c0 |
| Penicillin-Binding Protein 2a | E447K | 1000 | 4.2 ± 0.7 | -24.1 | 10.1073/pnas.21012911 |
3. Experimental Protocols Protocol 3.1: Ensemble Generation via Accelerated Molecular Dynamics (aMD) Objective: To sample conformational states beyond accessible timescales of conventional MD. Materials: Prepared protein-ligand or apo protein system (e.g., from PDB), AMBER/NAMD/GROMACS software, aMD parameter set. Procedure:
- System Preparation: Solvate and neutralize the target system in a TIP3P water box. Minimize energy and equilibrate under NVT and NPT ensembles.
- Conventional MD: Run a 100ns standard MD simulation as a baseline to calculate average dihedral and total potential energies.
- aMD Parameters: Apply aMD boost potential using the dual-boost method. Set the dihedral energy threshold (Edihed) to the average from step 2 plus 4*standard deviation. Set the total energy threshold (Etotal) to the average from step 2.
- aMD Production Run: Execute a 500-1000ns aMD simulation. Save frames every 10ps.
- Cluster Analysis: Use the k-means or hierarchical clustering algorithm on the backbone RMSD matrix to identify dominant conformational states. Extract representative snapshots (cluster centroids) for the ensemble.
Protocol 3.2: Ensemble Docking Against Mutation-Induced Conformers Objective: To screen compounds against a spectrum of mutant protein conformations. Materials: Ensemble of protein structures (from Protocol 3.1), ligand library in SDF format, docking software (AutoDock Vina, Glide, UCSF DOCK). Procedure:
- Ensemble Preparation: Prepare each protein snapshot from the ensemble (hydrogen addition, charge assignment, grid generation).
- Consensus Grid Generation (Optional): For rigid-grid docking tools, generate a composite grid encompassing the volumetric union of all active site conformations.
- Parallel Docking: Dock the entire ligand library against each protein conformer in the ensemble using identical docking parameters and scoring functions.
- Score Integration: For each ligand, compile docking scores from all ensemble members. Calculate the minimum score (best fit to any conformation) and the ensemble-average score (robustness across states).
- Hit Prioritization: Rank ligands first by minimum score, then by ensemble-average score. Select candidates with favorable scores across multiple conformers for experimental validation.
4. Visualization of Workflows and Pathways
Title: Workflow for Ensemble-Based Docking Against Flexible Targets
Title: Mutation-Induced Conformational Change Leading to Resistance
5. The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Studying Target Flexibility in AMR
| Item | Function & Application |
|---|---|
| High-Performance Computing (HPC) Cluster | Enables long-timescale MD simulations (µs-ms) necessary to observe rare conformational events and mutant-induced shifts. |
| GPU-Accelerated MD Software (e.g., AMBER, GROMACS, NAMD) | Dramatically speeds up energy calculations, making ensemble generation computationally feasible. |
| Enhanced Sampling Suites (PLUMED, OpenMM) | Implements advanced algorithms (aMD, metadynamics) to overcome energy barriers and sample relevant states. |
| Stable Isotope-Labeled Amino Acids | For NMR studies to validate computational ensembles and measure atomic-level dynamics in solution. |
| Cryo-Electron Microscopy Grids | For high-resolution structural determination of multiple conformational states of large, flexible targets (e.g., efflux pumps). |
| FRET-Based Conformational Biosensors | To experimentally monitor real-time conformational changes in live bacteria upon drug binding or mutation. |
| Fragment Screening Libraries (e.g., 1000-compound set) | For experimental screening (X-ray, SPR) to identify binders to cryptic pockets revealed by MD simulations. |
Within the broader thesis on Computer-Aided Drug Design (CADD) applications in antimicrobial resistance (AMR) drug discovery, a paramount challenge is achieving selective toxicity. The objective is to design compounds that potently disrupt essential microbial pathways while exhibiting minimal affinity for homologous human targets, thereby avoiding off-target toxicity. This application note details contemporary computational and experimental protocols to predict, evaluate, and mitigate human off-target effects in the development of novel anti-infectives.
Key Off-Target Risks in Antimicrobial Agents
Common mechanisms of off-target toxicity arise from conserved structural or functional motifs between microbial and human proteins. Key risk areas include:
- Kinase Homology: Bacterial kinases (e.g., PknB) sharing ATP-binding site similarity with human kinome.
- Protease/Enzyme Conservation: Bacterial enzymes (e.g., gyrase/topoisomerase, DHFR) with human functional analogs.
- Membrane Disruption: Non-selective targeting of lipid bilayers leading to hemolysis or nephrotoxicity.
- hERG Channel Blockade: A prevalent cardiotoxicity risk due to unintended interaction with the human Ether-à-go-go-Related Gene potassium channel.
Recent literature and database mining (see Table 1) quantify these risks, highlighting the necessity for early-stage selectivity screening.
Table 1: Quantified Off-Target Risks for Common Antimicrobial Targets
| Antimicrobial Target Class | Example Microbial Target | Human Homolog / Off-Target | Reported Selectivity Index (Microbial IC50 / Human IC50) | Primary Toxicity Risk |
|---|---|---|---|---|
| Kinase | M. tuberculosis PknB | Various human S/T kinases | <10 for many early leads (PMID: 35113892) | Hepatotoxicity, Cytotoxicity |
| Topoisomerase | DNA Gyrase (GyrA/B) | Topoisomerase IIα | Varies widely; >100 is desirable | Genotoxicity, Cardiotoxicity |
| DHFR | Bacterial DHFR | Human DHFR | <5 for non-selective inhibitors (PMID: 36562744) | Bone marrow suppression |
| Cell Wall Synthesis | Penicillin-Binding Proteins (PBPs) | Human β-lactamase homologs (hBLH) | Typically >1000 (highly selective) | Generally low; allergic reaction |
| Membrane Integrity | Bacterial Lipopolysaccharide | Human mitochondrial membrane | Low (non-selective mechanism) | Nephrotoxicity, Hemolysis |
Computational Protocols for Selectivity Prediction
Protocol 3.1: In Silico Off-Target Profiling Using Reverse Pharmacophore Screening
Objective: To predict potential human off-targets of a novel antimicrobial hit compound.
Materials (Research Reagent Solutions):
- Software: Pharmit server, PharmMapper, or Schrödinger's Phase.
- Databases: PharmTargetDB, PDB, or internal conformer database of human target binding sites.
- Input: 3D conformation of the query ligand (SDF/MOL2 format).
Methodology:
- Ligand Preparation: Generate low-energy 3D conformers of the query compound using OMEGA or CONFGEN.
- Pharmacophore Generation: For each conformer, define key chemical features (H-bond donors/acceptors, hydrophobic regions, aromatic rings, charged groups).
- Database Screening: Screen the ensemble of pharmacophore models against a pre-built database of pharmacophores derived from:
- Ligand-binding sites of the entire human structural proteome.
- Specifically, the human kinome, GPCRome, ion channel family, and proteases.
- Scoring & Ranking: Use a weighted combination of geometric fit and chemical feature match to score and rank potential human off-targets.
- Validation: Cross-reference top hits with expression data (GTEx database) to prioritize targets in vital organs (heart, liver, kidney).
Protocol 3.2: Structural-Based Selectivity Analysis via Ensemble Docking
Objective: To evaluate binding energy differentials between microbial target and homologous human off-targets.
Materials:
- Software: Molecular docking suite (e.g., GLIDE, GOLD, AutoDock Vina).
- Structures: High-resolution X-ray/cryo-EM structures of both the primary microbial target and its human homolog(s) (from PDB/AlphaFold DB).
- Preparation Suite: Protein Preparation Wizard (Schrödinger) or UCSF Chimera.
Methodology:
- Protein Structure Preparation:
- Retrieve and align structures of the microbial target (e.g., bacterial kinase) and its human homolog(s).
- Add missing hydrogen atoms, assign protonation states at pH 7.4, and optimize H-bond networks.
- Define the binding site using the co-crystallized ligand or a conserved catalytic residue centroid (5-10 Å radius).
- Ligand Library Docking:
- Dock a focused library of lead analogs into the prepared binding sites of both the microbial and human targets.
- Use standard precision (SP) or extra precision (XP) scoring functions.
- Selectivity Scoring:
- Calculate ΔG_bind (predicted) for each compound to both targets.
- Compute a computational selectivity score (CSS): CSS = ΔGbind(Human) - ΔGbind(Microbe). A higher positive CSS indicates greater theoretical selectivity for the microbial target.
- Analysis: Identify ligand moieties that contribute favorably to microbial target binding but unfavorably to human target binding (via interaction diagrams).
Diagram 1: CADD workflow for off-target prediction and selectivity analysis (92 chars)
Experimental Protocols for Validation
Protocol 4.2: In Vitro Selectivity Panel Screening (Kinase-Focused Example)
Objective: Experimentally determine IC50 values against a prioritized human kinome panel versus the microbial kinase target.
Materials (Research Reagent Solutions):
- Assay Kits: ADP-Glo Kinase Assay Kit (Promega) for biochemical activity.
- Kinase Panel: Recombinant human kinases (e.g., from Reaction Biology or Eurofins) selected based on computational prediction.
- Positive Controls: Staurosporine (broad kinase inhibitor) and a known selective microbial kinase inhibitor (if available).
- Microplate Reader: Luminometer capable of reading 384-well plates.
Methodology:
- Reaction Setup: In a low-volume 384-well plate, serially dilute test compounds (10 mM DMSO stock) in kinase assay buffer.
- Kinase Addition: Add the microbial target kinase and each human kinase separately to their respective wells.
- ATP & Substrate Addition: Initiate reaction with ATP/substrate peptide mix. Incubate at room temperature for 60-120 min.
- Detection: Add ADP-Glo Reagent to stop reaction and deplete residual ATP, followed by Kinase Detection Reagent to convert ADP to ATP and generate luminescence.
- Data Analysis:
- Normalize luminescence signals to DMSO (100% activity) and staurosporine (0% activity) controls.
- Fit dose-response curves to calculate IC50 for each kinase.
- Calculate Experimental Selectivity Index (ESI): ESI = IC50(Human Kinase) / IC50(Microbial Kinase). Target ESI > 30.
Table 2: Essential Toolkit for In Vitro Selectivity Screening
| Reagent / Material | Provider Example | Function in Selectivity Assessment |
|---|---|---|
| ADP-Glo Kinase Assay Kit | Promega | Universal, bioluminescent biochemical kinase assay to measure inhibition across species. |
| Recombinant Human Kinase Panel | Reaction Biology, Eurofins | Provides purified human off-target proteins for high-throughput biochemical screening. |
| hERG Inhibition Assay Kit (e.g., Predictor) | Thermo Fisher | Fluorescence-based assay to quantify compound binding to the hERG channel, predicting cardiotoxicity risk. |
| Cytotoxicity Assay Kit (e.g., CellTiter-Glo) | Promega | Measures ATP levels as proxy for mammalian cell viability after compound treatment. |
| Pan-Promiscuity Compound Library (e.g., aggregators, redox cyclers) | Enamine, MLSMR | Used as negative controls to identify and eliminate non-selective compound behaviors. |
| Membrane Permeability Assay (PAMPA) | pION | Predicts passive transcellular absorption, informing potential for systemic exposure and off-target access. |
Protocol 4.2: Cell-Based Counter-Screening for Cytotoxicity
Objective: Assess compound toxicity against relevant human cell lines (e.g., HEK-293, HepG2, cardiomyocytes) at antimicrobial concentrations.
Methodology:
- Seed cells in 96-well tissue culture plates.
- Treat with test compounds at concentrations up to 10x the predicted antimicrobial EC50.
- Incubate for 48-72 hours.
- Assess viability using CellTiter-Glo 2.0 (luminescence-based ATP quantitation).
- Calculate Therapeutic Index (TI) in cells: TI = HC50 (cytotoxicity) / EC50 (antimicrobial activity in a cell-based infection model). Target TI > 10.
Diagram 2: Integrated selectivity screening funnel from in silico to in vivo (99 chars)
Integrating these computational and experimental protocols into the CADD-driven AMR drug discovery pipeline creates a robust funnel for improving selectivity. Early and iterative application of reverse pharmacophore screening, ensemble docking, and focused in vitro counter-screening systematically de-risks compounds for human off-target toxicity. This strategy aligns with the core thesis that advanced CADD is indispensable for efficiently delivering novel, safe, and effective antimicrobials to combat resistant infections.
Within the Computer-Aided Drug Design (CADD) pipeline for combatting antimicrobial resistance (AMR), optimizing compounds for bacterial membrane permeability is a critical, non-negotiable step. A potent molecule is ineffective if it cannot reach its intracellular target (e.g., DNA gyrase, ribosomes) in Gram-negative bacteria, which possess a formidable double-membrane barrier. This application note details the computational and experimental protocols integrated into a broader CADD thesis to design, prioritize, and validate compounds with enhanced permeability.
Key Physicochemical Properties & Predictive Models
Permeability across the complex Gram-negative envelope involves passive diffusion through outer membrane porins and traversal of the inner lipid bilayer. Key properties influencing this process are quantified in Table 1.
Table 1: Key Physicochemical Properties for Bacterial Membrane Permeability
| Property | Target Range (for Porin Mediated Uptake) | Rationale & Measurement Method |
|---|---|---|
| Molecular Weight (MW) | < 600 Da | Smaller molecules diffuse more readily through porin channels. |
| Topological Polar Surface Area (TPSA) | < 140 Ų | Lower polar surface area correlates with better passive diffusion. |
| Lipophilicity (cLogD at pH 7.4) | -1 to +3 | Balanced hydrophilicity needed for water solubility and lipid bilayer traversal. Calculated or measured LogD. |
| Number of Rotatable Bonds (NRB) | ≤ 10 | Fewer rotatable bonds increase rigidity, often favoring permeation. |
| Net Charge at pH 7.4 | Neutral or Zwitterionic | Cationic compounds may bind to lipopolysaccharides; anions may be repelled. |
| Predictive Score: Permeability Coefficient (Log Papp) | > -6.0 cm/s | Predicted from in vitro PAMPA or cell-based assays. |
Protocol 1.1: Computational Prediction of Permeability-Likeness
- Objective: To computationally filter virtual compound libraries for permeability potential.
- Procedure:
- Property Calculation: Using tools like RDKit, OpenBabel, or commercial suites (Schrödinger, MOE), calculate MW, TPSA, cLogP/cLogD, NRB, and pKa for all compounds.
- Rule-Based Filtering: Apply "Rule-of-5-like" filters specific for Gram-negative permeability (e.g., MW < 600, TPSA < 140, cLogD -1 to +3).
- Machine Learning Scoring: Input calculated descriptors into pre-trained models (e.g., Random Forest, Deep Learning) for outer membrane permeability (OMP) prediction. Models like
OMPdbor in-house trained classifiers can be used. - Molecular Dynamics (MD) Simulation (For Leads): For promising leads, perform MD simulations in a model outer membrane (asymmetric bilayer with lipopolysaccharides) to visualize interaction dynamics and estimate free energy of permeation.
- Output: A ranked list of compounds prioritized for synthesis and experimental testing.
Experimental Validation Protocols
Protocol 2.1: Outer Membrane Permeability Assay using NPN Uptake
- Objective: Quantify disruption or passive diffusion through the outer membrane of Gram-negative bacteria.
- Materials:
- Bacterial culture (e.g., E. coli MG1655)
- N-Phenyl-1-naphthylamine (NPN) fluorescent probe
- 5 mM HEPES buffer (pH 7.2)
- Test compounds and controls (Polymyxin B, Chloramphenicol)
- Fluorescence plate reader
- Procedure:
- Grow bacteria to mid-log phase, harvest, and wash 2x in 5 mM HEPES.
- Resuspend to an OD600 of 0.5 in HEPES buffer.
- In a black 96-well plate, mix 100 µL bacterial suspension with 10 µL of 100 µM NPN and 10 µL of serially diluted test compound.
- Immediately measure fluorescence (λex = 350 nm, λem = 420 nm) for 5-10 minutes.
- Calculate fold-increase in fluorescence relative to untreated cells. Polymyxin B (membrane disruptor) serves as a positive control.
Protocol 2.2: Accumulation Assay using LC-MS/MS
- Objective: Directly measure intracellular concentration of a test compound over time.
- Materials:
- Bacterial culture
- Test compound
- LC-MS/MS system
- Cold PBS wash buffer
- Acetonitrile/Methanol lysis solution
- Procedure:
- Expose bacterial cells (OD600 ~ 1.0) to a known concentration (e.g., 10 µg/mL) of test compound at 37°C.
- At time points (e.g., 2, 5, 10, 30 min), rapidly pellet 1 mL aliquots (e.g., 13,000 rpm, 1 min, 4°C).
- Wash pellets twice with ice-cold PBS to remove extracellular compound.
- Lyse cells with 80:20 acetonitrile:water containing an internal standard.
- Clarify lysate by centrifugation and analyze supernatant via LC-MS/MS against a standard curve.
- Calculate intracellular concentration (µg/mL) and accumulation ratio (Intra/Extra).
Visualization of Workflows & Pathways
CADD Permeability Optimization Pipeline
Drug Permeation Pathways in Gram-Negative Bacteria
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Permeability Studies
| Item | Function/Description | Example Supplier/Product |
|---|---|---|
| Caco-2/HT-29-MTX Cell Lines | In vitro model for predicting human intestinal permeability, relevant for oral drug bioavailability. | ATCC, Sigma-Aldrich |
| PAMPA (Parallel Artificial Membrane Permeability Assay) Kit | High-throughput non-cell-based assay to predict passive transcellular permeability. | pION, Corning |
| N-Phenyl-1-naphthylamine (NPN) | Hydrophobic fluorescent probe used to assess outer membrane integrity and compound uptake. | Sigma-Aldrich, TCI |
| Ethidium Bromide or SYTOX Green | DNA-binding fluorescent dyes used in efflux inhibition assays (e.g., with PAβN). | Thermo Fisher, Invitrogen |
| Phenylalanine-Arginine β-Naphthylamide (PAβN) | Broad-spectrum efflux pump inhibitor; used to determine if poor accumulation is due to efflux. | Sigma-Aldrich |
| Asymmetric Lipid Bilayer Components | Purified Lipopolysaccharides (LPS), phospholipids for constructing realistic outer membrane models for MD simulations or biophysical studies. | Avanti Polar Lipids |
| LC-MS/MS System | Gold standard for quantifying precise intracellular and extracellular concentrations of test compounds. | Sciex, Agilent, Waters |
| Specialized Permeability Prediction Software | Tools for calculating 3D descriptors, performing molecular dynamics, and running ML models. | Schrödinger (Desmond), OpenEye, MOE, RDKit |
Introduction in CADD for AMR Research Computer-Aided Drug Design (CADD) offers a powerful avenue for accelerating antimicrobial resistance (AMR) drug discovery. However, its predictive accuracy is fundamentally constrained by the quality of underlying biological data. This Application Note details the specific challenges of sparse and noisy data in AMR research and provides protocols for curation to enhance CADD model reliability.
Quantifying the Challenge: Key Data Sources and Their Limitations The primary data sources for CADD in AMR exhibit inherent sparsity and noise. The following table summarizes quantitative aspects of this challenge.
Table 1: Common AMR Data Sources & Curation Challenges
| Data Type | Typical Source | Sparsity Metric | Primary Noise Sources |
|---|---|---|---|
| Minimum Inhibitory Concentration (MIC) | Public databases (e.g., ChEMBL, PubChem), in-house assays | ~85% of possible compound-bug pairs untested | Biological assay variability, protocol differences, endpoint interpretation. |
| Whole Genome Sequencing (WGS) of Resistant Strains | NCBI, ENA, institutional sequencing | Uneven sampling across species/genotypes; many genes of unknown function. | Sequencing errors, incomplete annotation, distinguishing resistance vs. benign mutations. |
| Protein Structures (AMR targets) | PDB, AlphaFold DB | <30% of known AMR-related proteins have experimental structures. | Crystal packing artifacts, resolution limits, missing loops in AF2 models. |
| High-Throughput Screening (HTS) Data | Published campaigns, institutional data | Hit rates often <0.1%, leading to highly imbalanced data. | False positives/negatives from assay interference, compound aggregation. |
Protocol 1: Curation and Standardization of MIC Data for QSAR Modeling
Objective: To transform raw, heterogeneous MIC data into a consistent, machine-learning-ready dataset for Quantitative Structure-Activity Relationship (QSAR) model training.
Materials (Research Reagent Solutions):
- Primary Data: MIC data exports from ChEMBL, PubChem BioAssay, or internal databases.
- Standardization Software: KNIME Analytics Platform or Python (Pandas, RDKit).
- Curated Reference Strain Data: ATCC or EUCAST standard strain MIC distributions for normalization.
- Descriptor Calculation Tool: Mordred or RDKit molecular descriptor calculators.
Procedure:
- Data Aggregation: Compile MIC entries from all sources into a single table (Fields: Compound SMILES, Organism, MIC value, MIC unit, reference).
- Unit Harmonization: Convert all MIC values to a single unit (e.g., µM). Flag entries where conversion is ambiguous.
- Strain Mapping: Map all organism names to standard NCBI taxonomy IDs. Cluster strains of the same species for analysis.
- Outlier Detection (Z-Score): For each compound tested against >10 strains of the same species, calculate the Z-score of log(MIC). Flag entries with |Z-score| > 3 for manual review.
- Activity Thresholding: Define a binary activity label (e.g., Active if MIC ≤ clinically relevant breakpoint). Use EUCAST/CLSI guidelines where available.
- Descriptor Generation: From the curated SMILES, compute a standardized set of 2D and 3D molecular descriptors. Remove descriptors with >20% missing values or near-zero variance.
- Dataset Splitting: Perform stratified splitting by organism and activity class to create training, validation, and test sets. Ensure no data leakage.
Protocol 2: Integrating Noisy Genomic Variant Data with Protein Structures
Objective: To prioritize resistance-conferring mutations from WGS data by integrating structural and evolutionary context.
Materials (Research Reagent Solutions):
- Variant Call Format (VCF) Files: From sequencing of resistant bacterial isolates.
- Reference Proteome: Corresponding protein sequences from UniProt.
- 3D Protein Structure: Experimental (PDB) or predicted (AlphaFold) model of target protein.
- Analysis Suite: PyMol, BioPython, HMMER suite, SNPeff.
Procedure:
- Variant Annotation & Filtering: Use SNPeff to annotate VCF files. Filter for non-synonymous mutations in genes known or suspected to be involved in AMR (e.g., efflux pumps, target enzymes).
- Evolutionary Conservation Scoring: Perform multiple sequence alignment (MSA) of the target protein against a diverse homolog set using HMMER. Calculate the Shannon entropy or ScoreCons for each residue position.
- Structural Mapping & Analysis: a. Map prioritized mutations onto the 3D protein structure. b. Calculate change in residue volume, charge, and hydrophobicity. c. Using PyMol, measure distances from the mutated site to known active site, substrate binding pocket, or protein-protein interaction interfaces.
- Functional Prioritization: Create a scoring matrix combining: (i) Conservation score (high weight), (ii) Magnitude of physicochemical change, (iii) Proximity to functional sites. Mutations exceeding a defined threshold are flagged as high-confidence resistance markers for CADD (e.g., to guide focused library design against a mutant target).
Visualizations
Title: MIC Data Curation for QSAR
Title: Genomic Variant to CADD Prioritization
The Scientist's Toolkit: Key Reagents & Resources
Table 2: Essential Resources for AMR Data Curation
| Item | Function in Curation | Example/Provider |
|---|---|---|
| ChEMBL / PubChem BioAssay | Primary repositories for publicly available bioactivity data, including MICs. | EMBL-EBI, NCBI |
| EUCAST / CLSI Guidelines | Provide standardized breakpoints and methods for MIC interpretation and thresholding. | eucast.org, clsi.org |
| RDKit | Open-source cheminformatics toolkit for SMILES handling, descriptor calculation, and standardization. | rdkit.org |
| AlphaFold Protein Structure Database | Provides high-accuracy predicted protein structures for targets lacking experimental data. | alphafold.ebi.ac.uk |
| PATRIC / CARD | Specialized databases for bacterial genomics and antibiotic resistance genes, aiding annotation. | patricbrc.org, card.mcmaster.ca |
| KNIME / Python (Pandas, Scikit-learn) | Platforms for building reproducible, visual, or scripted data curation and preprocessing pipelines. | knime.com, python.org |
Within the broader thesis on Computer-Aided Drug Design (CADD) applications in antimicrobial resistance (AMR) drug discovery, this document details the critical validation phase. The transition from in silico hits to confirmed in vitro activity is a pivotal bottleneck. These Application Notes and Protocols provide a structured framework for this process, focusing on high-priority targets in AMR research, such as novel beta-lactamase inhibitors, efflux pump blockers, and essential peptidoglycan biosynthesis enzymes.
Key Experimental Pathways & Considerations
The validation workflow follows a sequential, tiered approach to prioritize resources and confirm activity.
Diagram: Validation Workflow for CADD Hits
Diagram: Key AMR Target Pathway (e.g., NDM-1 Inhibition)
Table 1: Typical Prioritization Metrics for In Silico Hits Against AMR Targets
| Metric | Target Range/Value for Priority | Measurement Method (In Silico) | Purpose in AMR Context |
|---|---|---|---|
| Docking Score | ≤ -8.0 kcal/mol (Vina) | Molecular Docking | Predicts binding affinity to target (e.g., β-lactamase). |
| LE (Ligand Efficiency) | ≥ 0.3 kcal/mol/heavy atom | Docking Score / HA | Identifies efficient binders for scaffold optimization. |
| cLogP | 0 to 3 | QSPR Model | Optimizes for Gram-negative permeability. |
| tPSA | ≤ 140 Ų | Calculated Property | Predicts ability to cross bacterial membranes. |
| PAINS Alerts | 0 | Structural Filter | Removes promiscuous, assay-interfering compounds. |
| Synthetic Accessibility | ≤ 4.5 (1=easy, 10=hard) | SA Score | Prioritizes compounds feasible for rapid synthesis. |
Table 2: BenchmarkIn VitroActivity Tiers for Validation
| Assay Tier | Key Parameters | Success Criteria (Typical for AMR Hits) | Follow-Up Action |
|---|---|---|---|
| Tier 1: Biochemical | IC50, Ki, Mechanism | IC50 < 10 µM; Dose-response confirmed. | Progress to cell assay. |
| Tier 2: Cell-Based | MIC (µg/mL), Spectrum | MIC ≤ 32 µg/mL vs. resistant strain; >4-fold reduction vs. antibiotic alone. | Assess cytotoxicity. |
| Tier 3: Selectivity | CC50 (Mammalian cells), SI | Selectivity Index (SI = CC50/MIC) > 10. | Progress to in vivo models. |
Detailed Experimental Protocols
Protocol 1: Biochemical Inhibition Assay for a Novel Beta-Lactamase
Objective: Determine the half-maximal inhibitory concentration (IC50) of computational hits against a purified AMR enzyme (e.g., NDM-1).
Materials:
- Purified recombinant beta-lactamase enzyme.
- Test compounds (from in silico list, solubilized in DMSO).
- Nitrocefin (chromogenic substrate, 500 µM stock).
- Assay buffer (50 mM HEPES, pH 7.5, 100 µM ZnCl2).
- 96-well clear flat-bottom microplate.
- Microplate reader capable of measuring 486 nm.
Procedure:
- Enzyme Preparation: Dilute purified enzyme in assay buffer to a working concentration (e.g., 1 nM) that gives a linear change in absorbance over 5 minutes.
- Compound Serial Dilution: Prepare 3-fold serial dilutions of each test compound in DMSO, then dilute in assay buffer for a final 10-point concentration series (e.g., 100 µM to 0.05 µM). Final DMSO concentration must be constant (e.g., 1%) across all wells.
- Reaction Setup:
- Add 80 µL of enzyme solution to each well containing 10 µL of compound or buffer control (for 100% activity).
- Pre-incubate plate at 25°C for 15 minutes.
- Initiate reaction by adding 10 µL of nitrocefin substrate (final concentration 100 µM).
- Kinetic Measurement: Immediately monitor the increase in absorbance at 486 nm (ΔA486) for 5 minutes at 25°C.
- Data Analysis: Calculate the initial reaction velocity (V0) for each well. Normalize V0 as a percentage of the average velocity from DMSO-only control wells. Fit normalized data to a log(inhibitor) vs. response (four-parameter) model to calculate IC50.
Protocol 2: Microbroth Dilution MIC Assay for Synergistic Combinations
Objective: Evaluate the Minimum Inhibitory Concentration (MIC) of a standard antibiotic in the presence and absence of a fixed concentration of the computational hit against a resistant bacterial strain.
Materials:
- Cation-adjusted Mueller Hinton Broth (CAMHB).
- Mid-log phase culture of target AMR strain (e.g., E. coli producing NDM-1), adjusted to 0.5 McFarland standard.
- Antibiotic stock (e.g., Meropenem).
- Test compound stock (solubilized per Protocol 1).
- 96-well sterile U-bottom or round-bottom microplates.
- Multichannel pipettes.
Procedure:
- Plate Preparation:
- In a sterile microplate, perform a 2-fold serial dilution of the antibiotic down the columns (e.g., 128 µg/mL to 0.06 µg/mL) in CAMHB (50 µL final volume after all additions).
- Add CAMHB containing either the test compound (at a fixed sub-inhibitory concentration, e.g., 8 µg/mL) or an equivalent volume of diluent (DMSO) to the appropriate rows.
- Inoculation: Dilute the bacterial suspension 1:100 in CAMHB, then add 50 µL to each well, resulting in a final inoculum of ~5 x 10^5 CFU/mL. Include growth (no drug) and sterility (no inoculum) controls.
- Incubation: Seal plate and incubate at 37°C for 18-24 hours without shaking.
- Endpoint Determination: Visually inspect wells for turbidity. The MIC is the lowest concentration of antibiotic that completely inhibits visible growth. Compare the MIC of the antibiotic alone versus in combination with the test compound. A ≥4-fold reduction in MIC indicates synergistic potentiation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials forIn SilicotoIn VitroTransition in AMR
| Item/Reagent | Function & Rationale | Example/Supplier Note |
|---|---|---|
| Purified Recombinant AMR Enzyme | Direct target for biochemical validation of binding and inhibition. Essential for measuring Ki/IC50. | NDM-1, KPC-2, PBP2a from commercial protein suppliers (e.g., Sigma-Aldrich, R&D Systems) or in-house expression. |
| Chromogenic Cephalosporin Substrate (Nitrocefin) | Allows rapid, continuous spectrophotometric measurement of beta-lactamase activity. Turns red upon hydrolysis. | Gold standard for β-lactamase assays. Available from multiple biochemical suppliers (TOKU-E, MilliporeSigma). |
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized, reproducible medium for antimicrobial susceptibility testing (CLSI/EUCAST guidelines). | Essential for reliable MIC determination. Available from BD, Oxoid, etc. |
| Resistant Bacterial Strain Panels | Cell-based validation requires clinically relevant, genetically characterized AMR strains. | MRSA, ESBL-producing E. coli, Carbapenem-resistant P. aeruginosa from ATCC or BEI Resources. |
| Mammalian Cell Lines (e.g., HEK-293, HepG2) | For determining cytotoxicity (CC50) and calculating a Selectivity Index (SI), crucial for lead prioritization. | Standard cell lines for preliminary safety profiling. |
| High-Quality Chemical Libraries (for counter-screening) | To rule out false positives from computational hits (e.g., aggregation, fluorescence interference). | Pan-assay interference compound (PAINS) libraries available from commercial screening compound vendors. |
Proving Ground: Validating and Comparing CADD Successes in AMR
Application Notes
Computer-Aided Drug Design (CADD) has become an indispensable pillar in the fight against antimicrobial resistance (AMR), enabling the rapid and rational discovery of novel inhibitors against high-priority bacterial targets. This case study examines three prominent CADD-derived antimicrobial compounds currently in clinical development, highlighting the integrated computational and experimental workflows that propelled their discovery. The context is a thesis arguing that the strategic application of CADD is critical for circumventing traditional discovery bottlenecks and addressing the urgent threat of AMR.
Gepotidacin (GSK2140944)
Target: Bacterial Type II Topoisomerases (DNA Gyrase and TopoisIV). Discovery Path: Structure-based drug design initiated the optimization of novel triazaacenaphthylene scaffolds to interact with unique binding sites on gyrase, distinct from fluoroquinolones, to overcome existing resistance. Clinical Status: Phase III for uncomplicated urinary tract infection (uUTI) and gonorrhea. Significance: Represents a first-in-class, novel bacterial topoisomerase inhibitor (NBTI) with activity against resistant pathogens, including Neisseria gonorrhoeae and MRSA.
Zoliflodacin (ETX0914, AZD0914)
Target: Bacterial DNA Gyrase (GyrB subunit, novel binding site). Discovery Path: High-throughput screening followed by intensive structure-guided optimization utilizing protein-ligand co-crystal structures to improve potency and pharmacokinetic properties. Clinical Status: Phase III for uncomplicated gonorrhea (as a single-dose oral therapy). Significance: A novel spiropyrimidinetrione class inhibitor active against multi-drug resistant (MDR) and extensively drug-resistant (XDR) N. gonorrhoeae, including fluoroquinolone-resistant strains.
Afabicin (Debio 1450, AFN-1252)
Target: Staphylococcal-specific Enoyl-Acyl Carrier Protein Reductase (FabI). Discovery Path: Target-based virtual screening and molecular docking were employed to identify narrow-spectrum inhibitors specific to the staphylococcal FabI enzyme, minimizing impact on the microbiome. Clinical Status: Phase II completed for acute bacterial skin and skin structure infections (ABSSSI) caused by staphylococci. Significance: A first-in-class, narrow-spectrum agent demonstrating potent activity against MRSA and other staphylococci while sparing Gram-negative and anaerobic flora.
Table 1: CADD-Discovered Antimicrobial Inhibitors in Clinical Development
| Compound Name | Target & Mechanism | CADD Methodology | Indication (Phase) | Key Spectrum & Resistance Feature |
|---|---|---|---|---|
| Gepotidacin | Type II Topoisomerase Inhibitor (Novel binding site) | Structure-Based Drug Design (SBDD) | uUTI, Gonorrhea (Phase III) | Broad-spectrum; active vs. fluoroquinolone-resistant strains |
| Zoliflodacin | DNA Gyrase (GyrB) Inhibitor (Spiropyrimidinetrione) | Structure-Guided Optimization | Uncomplicated Gonorrhea (Phase III) | Specific for N. gonorrhoeae; active vs. MDR/XDR strains |
| Afabicin | Staphylococcal FabI Inhibitor (Narrow-spectrum) | Target-Based Virtual Screening, Docking | ABSSSI (Phase II completed) | Staphylococcus spp. specific; low resistance propensity |
Experimental Protocols
Protocol 1: Structure-Based Virtual Screening (SBVS) for Lead Identification
Based on methodologies foundational to discoveries like Afabicin.
Objective: To computationally screen large compound libraries against a validated, structurally resolved bacterial target to identify novel hit compounds.
Materials:
- High-resolution 3D protein structure (e.g., from PDB)
- Prepared small-molecule library (e.g., ZINC, in-house collection)
- Molecular docking software (e.g., Glide, AutoDock Vina, GOLD)
- High-performance computing (HPC) cluster
Procedure:
- Target Preparation:
- Retrieve the crystal structure of the target protein (e.g., SaFabI, PDB: 4ALH).
- Using molecular modeling software (e.g., Maestro, UCSF Chimera), remove water molecules and co-crystallized ligands not central to the binding site.
- Add missing hydrogen atoms, assign bond orders, and optimize protonation states of key residues (e.g., His, Asp, Glu) at physiological pH.
- Generate a receptor grid file defining the binding site coordinates, typically centered on the native ligand or a known active site.
Ligand Library Preparation:
- Download or curate a library of commercially available compounds in 2D (SMILES) format.
- Convert all structures to 3D, generate possible stereoisomers and tautomers.
- Minimize the energy of each ligand using a molecular mechanics force field (e.g., OPLS4).
- Output a standardized, formatted library file for docking.
Virtual Screening Docking:
- Configure the docking software with standard precision (SP) or high-throughput settings for initial screening.
- Dock each ligand from the prepared library into the defined receptor grid.
- Use a scoring function (e.g., GlideScore, ChemScore) to rank poses based on predicted binding affinity and interaction geometry.
Post-Docking Analysis & Hit Selection:
- Cluster top-ranked compounds (e.g., top 1000) by chemical similarity.
- Visually inspect docking poses of cluster representatives for key interactions (e.g., hydrogen bonds, pi-stacking, hydrophobic complementarity).
- Apply additional filters: drug-likeness (Lipinski's Rule of Five), absence of toxicophores, and favorable physicochemical properties.
- Select 50-150 diverse compounds for in vitro biochemical assay purchase and testing.
Protocol 2: Biochemical Inhibition Assay for FabI Inhibitors
A representative assay for validating hits against targets like FabI.
Objective: To determine the half-maximal inhibitory concentration (IC50) of candidate compounds against purified bacterial enoyl-ACP reductase (FabI) enzyme activity.
Materials:
- Purified recombinant FabI enzyme
- Substrates: crotonoyl-CoA, NADH
- Candidate inhibitor compounds (dissolved in DMSO)
- Assay buffer (e.g., 50 mM phosphate buffer, pH 7.5)
- Microplate reader (capable of reading absorbance at 340 nm)
Procedure:
- Assay Principle: FabI catalyzes the NADH-dependent reduction of trans-2-enoyl-ACP. The reaction is monitored by the decrease in absorbance at 340 nm corresponding to NADH oxidation.
- Reaction Setup: In a 96-well UV-transparent plate, add:
- 80 µL of assay buffer.
- 10 µL of candidate inhibitor at varying concentrations (typically from 100 µM to 0.1 nM in serial dilutions). Include a DMSO-only control for 100% activity.
- 10 µL of FabI enzyme (final concentration 10-50 nM).
- Initiation and Measurement:
- Pre-incubate the plate at 30°C for 5 minutes.
- Initiate the reaction by adding 100 µL of a substrate mixture (containing crotonoyl-CoA and NADH at final concentrations of 40 µM and 100 µM, respectively).
- Immediately transfer the plate to a pre-warmed microplate reader.
- Record the absorbance at 340 nm every 15 seconds for 5 minutes.
- Data Analysis:
- Calculate the initial velocity (V0) for each well from the linear portion of the absorbance vs. time curve.
- Normalize V0 values relative to the DMSO control (100% activity) and blank (0% activity).
- Plot inhibitor concentration vs. % enzyme activity. Fit the data to a four-parameter logistic equation to calculate the IC50 value.
Diagrams
Title: CADD to Clinic Path for Gepotidacin (87 chars)
Title: Structure-Based Virtual Screening Protocol (65 chars)
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for CADD-AMR Discovery
| Item | Function in CADD-AMR Research |
|---|---|
| High-Resolution Protein Structures (PDB) | Provides the 3D atomic coordinates of the bacterial target essential for structure-based design and docking. |
| Curated Small-Molecule Libraries (e.g., ZINC, MolPort) | Source of chemically diverse, often commercially available, compounds for in silico screening. |
| Molecular Docking Software (e.g., Glide, AutoDock) | Computationally predicts the binding pose and affinity of a small molecule within a protein's binding site. |
| Molecular Dynamics Simulation Suites (e.g., GROMACS, Desmond) | Models the dynamic behavior of protein-ligand complexes over time to assess stability and binding thermodynamics. |
| Purified Recombinant Bacterial Enzyme (e.g., FabI, Gyrase) | Essential for high-throughput biochemical assays to validate computational hits and determine IC50. |
| Fluorogenic/Chromogenic Enzyme Substrates | Enables real-time, sensitive measurement of target enzyme activity inhibition in biochemical assays. |
| Standardized Antimicrobial Panels (e.g., ESKAPE Pathogens) | Clinical or reference bacterial strains used to determine the in vitro MIC and spectrum of lead compounds. |
Application Notes
This analysis is framed within the ongoing computational effort to combat antimicrobial resistance (AMR), where Computer-Aided Drug Design (CADD) is pivotal for identifying novel inhibitors against resistant bacterial targets. The integration of molecular docking, molecular dynamics (MD), and machine learning (ML) has become a cornerstone of modern drug discovery pipelines. Performance evaluation of the underlying software and algorithms is critical for optimizing resource allocation and improving predictive accuracy in AMR-focused projects.
Table 1: Comparative Performance of Docking Software
| Software | Scoring Function | Typical Runtime (per ligand) | Pose Prediction Accuracy (RMSD < 2Å) | Strengths in AMR Context |
|---|---|---|---|---|
| AutoDock Vina | Empirical (Vina) | 1-5 min | ~70-80% | Fast, good for virtual screening of large libraries against known mutant targets. |
| GOLD | Empirical (ChemScore, GoldScore) | 5-15 min | ~75-85% | Flexible ligand handling, robust for metalloenzymes common in resistance (e.g., β-lactamases). |
| Glide (Schrödinger) | Empirical (GlideScore) | 3-10 min | ~80-90% | High accuracy in pose prediction, excellent for evaluating inhibitor binding to mutant active sites. |
| AutoDock4/GPU | Semi-empirical (Free Energy) | 10-30 min (GPU: <1 min) | ~70-80% | Provides estimated ΔG, useful for ranking potency against wild-type vs. mutant proteins. |
Table 2: Comparative Analysis of MD Simulation Engines
| Engine | Algorithm Core | Performance (ns/day)* | Key Metrics for AMR Studies | Typical Use Case |
|---|---|---|---|---|
| GROMACS | Leap-frog, LINCS | 50-200 (CPU/GPU) | Stability (RMSD), Binding Free Energy (MM/PBSA), H-bond occupancy. | Studying full protein flexibility, resistance mutations, and water-mediated interactions. |
| NAMD | Verlet, Multiple Timestep | 30-100 (CPU/GPU) | Binding free energy, Electrostatic potential mapping. | Large membrane-bound systems (e.g., efflux pumps). |
| AMBER | PMEMD, SPFP | 40-150 (GPU) | Detailed thermodynamic integration (TI), NMR refinement. | High-accuracy calculation of binding affinities for lead optimization. |
| OpenMM | Customizable, CUDA | 100-300+ (GPU) | Enhanced sampling efficiency. | Rapid conformational sampling and alchemical free energy calculations. |
*Performance varies based on hardware, system size (>50k atoms), and force field.
Table 3: ML Algorithm Performance in AMR-related Binding Affinity Prediction
| Algorithm Type | Example Tools/Libraries | Mean Absolute Error (MAE) [kcal/mol] | Key Feature Requirements | Application in AMR Discovery |
|---|---|---|---|---|
| Random Forest (RF) | scikit-learn, RF-Score | 1.2 - 1.8 | Fingerprints, topological descriptors. | Initial screening to prioritize compounds for resistant targets. |
| Gradient Boosting | XGBoost, LightGBM | 1.1 - 1.6 | Physicochemical descriptors, interaction fingerprints. | Ranking docked poses from mutant protein simulations. |
| Graph Neural Networks (GNN) | Pytorch Geometric, DGL | 0.9 - 1.4 | Atomic graphs, bond types. | Learning from structural data to predict inhibition of mutant enzymes. |
| 3D-CNN | DeepBindRG, Keras | 0.8 - 1.3 | Voxelized protein-ligand complexes. | Direct prediction from 3D structures of target-ligand complexes. |
Experimental Protocols
Protocol 1: Ensemble Docking for Mutant Bacterial Target Screening Objective: To account for target flexibility and mutation-induced conformational changes in a key AMR enzyme (e.g., NDM-1 β-lactamase).
- Target Preparation: Retrieve wild-type and clinically relevant mutant (e.g., NDM-1 V88L) structures from PDB or generate mutants via in silico mutagenesis (using UCSF Chimera).
- Ensemble Generation: For each protein structure, run a short (50ns) MD simulation (GROMACS/AMBER). Cluster trajectories (gromos method) to extract 5-10 representative conformations.
- Grid Generation: Using AutoDock Tools, define a grid box enclosing the active site and any allosteric pockets identified in MD. Generate a grid file for each protein conformation.
- Ligand Library Preparation: Prepare a library of 10,000 drug-like molecules (ZINC database) using Open Babel: convert to .pdbqt, add Gasteiger charges, detect rotatable bonds.
- Docking Execution: Run docking with AutoDock Vina against each protein conformation in the ensemble (exhaustiveness=32). Use a shell script to automate batch processing.
- Score Integration: For each ligand, take the best (lowest) binding affinity score across all conformations. Rank the entire library by this integrated score.
- Analysis: Visually inspect top-100 poses for conserved interactions. Compare consensus hits between wild-type and mutant to identify mutation-resilient inhibitors.
Protocol 2: Binding Free Energy Validation using MD/MM-PBSA Objective: To validate and refine docking hits by calculating binding free energy for a ligand complex with a resistant bacterial enzyme.
- System Setup: Take the top docking pose for a ligand-enzyme complex. Solvate the complex in a cubic TIP3P water box (minimum 10Å padding). Add ions to neutralize and achieve 0.15M NaCl concentration.
- Simulation Run (GROMACS):
- Minimization: Steepest descent (5000 steps) to remove clashes.
- Equilibration: NVT (100ps, 300K, V-rescale) followed by NPT (100ps, 1 bar, Parrinello-Rahman).
- Production MD: Run 3x 100ns replicates (totaling 300ns) with a 2fs timestep. Save frames every 10ps.
- Trajectory Analysis: Calculate backbone RMSD for stability. Extract 100 equally spaced frames from the last 50ns of each stable replicate (300 frames total).
- MM/PBSA Calculation: Use
g_mmpbsa(for GROMACS) to compute binding free energy (ΔGbind). The method decomposes: ΔGbind = EMM (gas phase) + Gsolv (solvation) - T*S. EMM includes bonded and non-bonded terms. Gsolv is computed via Poisson-Boltzmann (polar) and surface area (non-polar) methods. - Per-Residue Decomposition: Identify key binding residues contributing favorably to ΔG_bind. Compare profiles between wild-type and mutant complexes to pinpoint energy changes driving resistance.
Protocol 3: Training a GNN for Predicting Inhibition of Mutant Enzymes Objective: To develop a predictive ML model for inhibitor potency against a family of mutant enzymes.
- Dataset Curation: Compile experimental IC50/Ki data for compounds tested against wild-type and mutant enzymes (e.g., from ChEMBL, PDBbind). Convert IC50 to pIC50 (-log10(IC50)).
- Graph Representation: For each compound-enzyme complex, generate a molecular graph. Represent atoms as nodes (features: atom type, hybridization, degree) and bonds as edges (features: bond type, conjugation). Include spatial distance as an edge attribute if using spatial graphs.
- Model Architecture: Implement a Message Passing Neural Network (MPNN) using PyTorch Geometric. Use 3-5 message passing layers to aggregate neighbor information. Follow with global pooling and fully connected layers for regression (predicting pIC50).
- Training & Validation: Split data 70/15/15 (train/validation/test). Train using Mean Squared Error (MSE) loss with Adam optimizer. Use early stopping based on validation loss.
- Interpretation: Apply gradient-based attribution (e.g., GNNExplainer) to highlight subgraph structures in the ligand and key protein residues important for the prediction, offering insights into mutant-specific inhibitory chemotypes.
Diagrams
Title: Ensemble Docking Workflow for AMR Targets
Title: MD/MM-PBSA Binding Validation Protocol
Title: GNN Training Pipeline for Inhibitor Prediction
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational Tools for AMR CADD
| Item Name/Software | Category | Function in AMR Drug Discovery |
|---|---|---|
| RCSB Protein Data Bank (PDB) | Database | Primary source for 3D structures of wild-type and mutant bacterial targets (e.g., β-lactamases, efflux pumps). |
| ZINC20/ChEMBL | Database | Libraries of commercially available compounds (ZINC) and curated bioactivity data (ChEMBL) for model training and screening. |
| UCSF Chimera/AutoDock Tools | Visualization & Prep | Preparation of protein/ligand files (add H, charges), in silico mutagenesis, and visualization of docking/MD results. |
| GROMACS/AMBER | MD Engine | Simulating atomic-level dynamics of target-ligand complexes to study stability, binding modes, and free energy. |
| scikit-learn/PyTorch Geometric | ML Library | Providing algorithms (RF, XGBoost) and frameworks for building GNNs to predict binding and guide synthesis. |
| GPU Computing Cluster | Hardware | Accelerating computationally intensive tasks like MD simulations, docking of large libraries, and deep learning training. |
| MM/PBSA Tools (g_mmpbsa) | Analysis Script | Calculating binding free energies from MD trajectories to validate and rank compounds. |
Benchmarking Datasets and Success Metrics for Antimicrobial CADD
Introduction Within the broader thesis on Computer-Aided Drug Design (CADD) applications against antimicrobial resistance (AMR), standardized benchmarking is critical for evaluating tool performance and progress. This document provides application notes and protocols for utilizing key datasets and success metrics, enabling reproducible and comparable research in antimicrobial CADD.
Key Benchmarking Datasets for Antimicrobial CADD
Standardized datasets allow for the direct comparison of different computational models predicting antimicrobial activity, resistance, or physicochemical properties.
Table 1: Core Publicly Available Benchmarking Datasets
| Dataset Name | Primary Focus | Key Metric(s) | Size & Scope | Access Link / Reference |
|---|---|---|---|---|
| DBAASP | Antimicrobial peptides (AMPs) | MIC, Hemolytic activity, Cytotoxicity | >20,000 peptides | https://dbaasp.org |
| CAMP | Antimicrobial peptides (AMPs) | MIC, Activity (Antibacterial, Antifungal) | >8,000 sequences | https://camp.bicnirrh.res.in |
| DrugRes | Small molecule antibacterials | MIC, Resistance phenotype, Target | ~2,400 compounds | https://drugres.health/ |
| ChEMBL-ESKAPE | Small molecules vs. ESKAPE pathogens | MIC, IC50, Target data | Curated subset from ChEMBL | https://www.ebi.ac.uk/chembl/ |
| ATLAS | Small molecule antimicrobials | MIC, Toxicity data, Pathways | ~2,000 molecules | https://www.ebi.ac.uk/chembl/atlas |
| PDB (Protein Data Bank) | Target structures for docking | Resolution, Ligand co-crystals | >2,000 antimicrobial targets | https://www.rcsb.org |
Application Notes for Dataset Use:
- Pre-processing is Paramount: Always apply consistent filtering (e.g., for exact MIC values, specific strains like E. coli ATCC 25922) before benchmarking to ensure fair comparison.
- Define Your Benchmark Split: Clearly state if you are using a predefined train/validation/test split (if provided) or describe your random split methodology (e.g., 80/10/10) with a fixed random seed for reproducibility.
- Address Data Redundancy: Use tools like
cd-hitfor sequence data or molecular fingerprint clustering for small molecules to create non-redundant test sets that minimize bias.
Protocol 1.1: Creating a Non-Redundant Benchmark Set from DBAASP Objective: Generate a clustered benchmark set of antimicrobial peptides for machine learning.
- Data Retrieval: Query DBAASP for all peptides with confirmed MIC values against Staphylococcus aureus.
- Sequence Cleaning: Remove duplicates and sequences with ambiguous amino acids (B, J, X, Z).
- Clustering: Use the
cd-hitsuite (cd-hitorcd-hit-2d).
- Representative Selection: From each cluster generated by
cd-hit, select the peptide with the most comprehensive experimental data (e.g., MIC + hemolysis) as the representative. - Stratified Splitting: Split the representative sequences into training (70%), validation (15%), and test (15%) sets, ensuring proportional distribution of activity ranges (e.g., high, medium, low MIC) across sets.
Critical Success Metrics and Evaluation Protocols
Moving beyond simple accuracy is essential for meaningful benchmarking in AMR-CADD.
Table 2: Success Metrics for Antimicrobial CADD Models
| Metric Category | Specific Metric | Formula / Description | Relevance to AMR Discovery |
|---|---|---|---|
| Predictive Performance | Balanced Accuracy | (Sensitivity + Specificity) / 2 |
Mitigates class imbalance in active/inactive data. |
| Matthews Correlation Coefficient (MCC) | (TP×TN - FP×FN) / √((TP+FP)(TP+FN)(TN+FP)(TN+FN)) |
Robust single metric for binary classification. | |
| Mean Absolute Error (MAE) on log(MIC) | Σ | log2(MIC_pred) - log2(MIC_exp) | / n |
Directly evaluates precision of potency prediction. | |
| Early Enrichment | ROC Enrichment (e.g., EF₁₀₀) | (Actives_found / N_found) / (Total_Actives / Total_Compounds) |
Measures model's ability to rank true actives early in a virtual screen. |
| Druggability Assessment | ADMET Prediction Concordance | Percentage of hits passing key filters (e.g., Ro5, PAN-ASSESS, hERG) | Filters for compounds with viable drug-like properties. |
Protocol 2.1: Benchmarking a Virtual Screening Pipeline with Early Enrichment Objective: Evaluate a docking/machine learning pipeline's ability to enrich true hits from a decoy library.
- Prepare Benchmark Library: Combine known active compounds (from ChEMBL-ESKAPE, n=50) with property-matched decoys (from ZINC20 database, n=1950) using tools like
DUD-EorLibGuacamoleto create a 2000-molecule library (2.5% actives). - Run Virtual Screen: Execute the candidate CADD pipeline (e.g., molecular docking with Glide SP).
- Rank and Analyze: Rank all 2000 compounds by the primary score (e.g., docking score). Calculate the enrichment factor at 1% (EF₁₀₀), 5% (EF₂₀), and 10% (EF₁₀) of the screened library.
- Plot & Report: Generate an ROC curve and calculate the Area Under the Curve (AUC). Report EF₁₀₀, EF₂₀, and AUC.
Protocol 2.2: Evaluating MIC Prediction Models Objective: Assess a regression model's performance in predicting minimum inhibitory concentration (MIC).
- Data Preparation: Use a curated dataset (e.g., from DrugRes) with reliable MIC values (in µg/mL). Convert MIC to log₂(MIC) for modeling.
- Model Training & Prediction: Train model on training set. Predict log₂(MIC) for the held-out test set.
- Calculate Metrics:
- Mean Absolute Error (MAE): Average absolute difference between predicted and experimental log₂(MIC).
- Critical Success Index (CSI): Calculate the fraction of predictions where
|log2(MIC_pred) - log2(MIC_exp)| <= 1(i.e., within one 2-fold dilution). This is a stringent, microbiologically relevant metric.
- Report: Present MAE, CSI, and a scatter plot of Predicted vs. Experimental log₂(MIC).
Visualizations
Diagram 1: AMR CADD Benchmarking Workflow
Diagram 2: Key Success Metric Relationships
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Antimicrobial CADD Benchmarking
| Item / Resource | Function / Purpose in Benchmarking | Example / Source |
|---|---|---|
| ChEMBL Database | Primary source for curated bioactivity data (MIC, IC₅₀) for small molecules. | https://www.ebi.ac.uk/chembl |
| DBAASP | Central repository for experimentally tested antimicrobial peptide sequences and activities. | https://dbaasp.org |
| RDKit | Open-source cheminformatics toolkit for molecule manipulation, descriptor calculation, and modeling. | https://www.rdkit.org |
| cd-hit Suite | Tool for clustering biological sequences to remove redundancy and create unbiased datasets. | http://weizhongli-lab.org/cd-hit/ |
| ZINC Database | Source of purchasable compound structures for generating property-matched decoy molecules. | https://zinc.docking.org |
| LibGuacamole | Tool for generating challenging, property-matched decoy libraries for rigorous enrichment tests. | https://github.com/LLNL/libguacamole |
| scikit-learn | Python library for implementing machine learning models and standard performance metrics. | https://scikit-learn.org |
| GNINA | Deep learning-based molecular docking framework, useful for benchmarking against classical methods. | https://github.com/gnina/gnina |
Within the broader thesis on Computer-Aided Drug Design (CADD) applications against antimicrobial resistance (AMR), in silico predictions of antimicrobial activity and resistance liability require rigorous experimental validation. This transition from virtual hits to viable leads is a critical bottleneck. The integrated application of Minimum Inhibitory Concentration (MIC), Time-Kill Kinetics, and Resistance Development studies forms a foundational triad for characterizing compound efficacy, pharmacodynamic profile, and potential for resistance selection—key de-risking steps in the AMR drug discovery pipeline.
Core Experimental Protocols
Protocol 2.1: Broth Microdilution for Minimum Inhibitory Concentration (MIC)
Objective: To determine the lowest concentration of a test compound that inhibits visible growth of a microorganism.
Detailed Methodology:
- Compound Preparation: Serially dilute the test compound (typically starting at 64 µg/mL or 4x the expected MIC) in cation-adjusted Mueller-Hinton Broth (CAMHB) for bacteria, or RPMI-1640 for fungi, in a 96-well microtiter plate. Use two-fold dilution steps.
- Inoculum Preparation: Adjust the turbidity of a mid-log-phase microbial culture to a 0.5 McFarland standard (~1-5 x 10^8 CFU/mL for bacteria). Further dilute in broth to achieve a final concentration of ~5 x 10^5 CFU/mL per well.
- Inoculation & Incubation: Add 100 µL of the standardized inoculum to each well containing 100 µL of the serially diluted compound. Include growth control (no compound) and sterility control (no inoculum) wells.
- Incubation: Incubate the plate statically at 35±2°C for 16-20 hours (bacteria) or 24-48 hours (fungi).
- Endpoint Determination: The MIC is the lowest compound concentration that completely inhibits visible growth. For precise results, use a spectrophotometric plate reader to measure optical density at 600 nm (OD600). An OD600 ≤ 0.1 (or ≥90% inhibition vs. growth control) typically indicates inhibition.
- Quality Control: Test reference antibiotics (e.g., ciprofloxacin for E. coli, vancomycin for S. aureus) concurrently to ensure media and methodology integrity.
Protocol 2.2: Time-Kill Kinetics Assay
Objective: To evaluate the rate and extent of bactericidal/fungicidal activity over time.
Detailed Methodology:
- Setup: Prepare flasks containing CAMHB with the test compound at concentrations of 0.5x, 1x, 2x, and 4x the predetermined MIC. Include a growth control flask without compound.
- Inoculation: Inoculate each flask with the test organism to a final density of ~5 x 10^5 CFU/mL.
- Sampling: Remove aliquots (e.g., 100 µL) from each flask at predetermined time points (e.g., 0, 2, 4, 6, 8, 24 hours).
- Viable Count: Serially dilute each aliquot in sterile saline or phosphate-buffered saline (PBS). Plate appropriate dilutions onto Mueller-Hinton Agar (MHA) plates. Incubate plates for 18-24 hours at 37°C.
- Enumeration & Analysis: Count colony-forming units (CFU/mL) for each sample. Plot Log10 CFU/mL versus time. Bactericidal activity is defined as a ≥3-log10 (99.9%) reduction in CFU/mL from the initial inoculum. Bacteriostatic activity maintains the inoculum level within a ±2-log10 range.
Protocol 2.3: Serial Passage Resistance Development Study
Objective: To assess the potential for a microorganism to develop resistance to a compound upon repeated sub-inhibitory exposure.
Detailed Methodology:
- Day 1 Passage: Start with multiple flasks containing broth with compound at sub-MIC levels (e.g., 0.25x, 0.5x MIC). Inoculate each with ~5 x 10^5 CFU/mL. Incubate for 24 hours.
- Daily Subculturing: Each day, take an aliquot (typically 1-10%) from the flask showing the highest growth in the presence of the compound and use it to inoculate fresh broth containing the same or incrementally increased (e.g., 2-fold) concentration of the compound.
- MIC Tracking: Every 3-4 days, determine the MIC of the passaged strain against the test compound and relevant comparators using Protocol 2.1.
- Endpoint & Analysis: Continue passage for a predetermined period (e.g., 14-28 days) or until a significant MIC increase (e.g., ≥8-fold) is observed. The fold-change in MIC over time is a direct measure of resistance development propensity.
- Genetic Analysis: Subject endpoint isolates with elevated MICs to whole-genome sequencing to identify acquired resistance mutations.
Table 1: Example MIC Data for Novel Inhibitor 'CADD-AMR-001' Against ESKAPE Pathogens
| Organism (Strain) | CADD-AMR-001 MIC (µg/mL) | Levofloxacin MIC (µg/mL) | Colistin MIC (µg/mL) | Clinical Breakpoint (S ≤ /R ≥ µg/mL) for Comparator |
|---|---|---|---|---|
| Staphylococcus aureus (ATCC 29213) | 1 | 0.25 | >16 | Levo: 1/4 |
| Escherichia coli (ATCC 25922) | 2 | 0.06 | 0.5 | Levo: 0.5/1 |
| Klebsiella pneumoniae (ATCC 700603) | 4 | >32 | 1 | Colistin: 2/4 |
| Acinetobacter baumannii (Clinical isolate) | 8 | >32 | 0.5 | Colistin: 2/4 |
| Pseudomonas aeruginosa (ATCC 27853) | 16 | 2 | 2 | Levo: 1/4 |
Table 2: Time-Kill Kinetic Profile of CADD-AMR-001 vs. Vancomycin against MRSA
| Time Point (h) | Growth Control (Log10 CFU/mL) | CADD-AMR-001 at 4x MIC (Log10 CFU/mL) | Vancomycin at 4x MIC (Log10 CFU/mL) |
|---|---|---|---|
| 0 | 5.5 ± 0.1 | 5.5 ± 0.1 | 5.5 ± 0.1 |
| 2 | 6.1 ± 0.2 | 4.8 ± 0.3 | 5.9 ± 0.2 |
| 4 | 7.3 ± 0.2 | 3.1 ± 0.4 | 6.0 ± 0.3 |
| 8 | 8.9 ± 0.3 | <1.7 (99.99% kill) | 5.2 ± 0.4 |
| 24 | 9.5 ± 0.2 | <1.7 | 3.5 ± 0.5 |
Table 3: Serial Passage Resistance Development (Fold Increase in MIC)
| Compound | Passage Day | S. aureus MIC Fold-Change | E. coli MIC Fold-Change | P. aeruginosa MIC Fold-Change |
|---|---|---|---|---|
| CADD-AMR-001 | 0 (Baseline) | 1x | 1x | 1x |
| 7 | 2x | 2x | 4x | |
| 14 | 2x | 4x | 8x | |
| 21 | 4x | 8x | 32x | |
| Ciprofloxacin (Control) | 0 | 1x | 1x | 1x |
| 7 | 8x | 16x | 16x | |
| 14 | 32x | 64x | 64x |
Diagrams
Diagram 1: Experimental Validation Workflow in CADD-AMR Pipeline
Diagram 2: Time-Kill Curve Interpretation Logic
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Cation-Adjusted Mueller Hinton Broth (CAMHB) | Standardized medium for MIC assays against bacteria; controlled divalent cation (Ca2+, Mg2+) levels ensure reproducible antibiotic activity, especially for cationic peptides. |
| Pre-prepared MIC Panels & Sensititre Systems | Lyophilized or frozen plates with pre-diluted antibiotics for high-throughput, reproducible MIC testing against large panels of clinical isolates. |
| 96-well & 384-well Microtiter Plates (Sterile, Tissue-Culture Treated) | For broth microdilution assays; TC-treated plates minimize compound binding to plastic. |
| Automated Plate Reader (Spectrophotometer) | For high-throughput, objective OD600 measurement to determine MIC endpoints and generate growth curves. |
| WASP & replicator systems | Automated instruments for precise, rapid inoculation of multiple agar plates for colony counting from time-kill assays. |
| Microbial DNA Extraction Kits | For rapid purification of genomic DNA from passaged isolates prior to sequencing for resistance mutation identification. |
| Quality Control Strain Panels (ATCC/CLSI recommended) | Standard reference strains (e.g., E. coli ATCC 25922, S. aureus ATCC 29213) for daily validation of assay conditions and media. |
The escalating crisis of antimicrobial resistance (AMR) demands accelerated and cost-effective drug discovery pipelines. Computer-Aided Drug Design (CADD) has emerged as a critical discipline, integrating computational power with biological insight to streamline the identification and optimization of novel antimicrobial agents. Within the broader thesis of leveraging computational methodologies to combat AMR, this document details specific application notes and protocols that quantify the tangible benefits of CADD in reducing both time and financial expenditure in preclinical research.
The integration of CADD techniques at various stages of the drug discovery pipeline demonstrably compresses timelines and reduces costs. The following tables consolidate key metrics from recent studies and industry reports.
Table 1: Time Reduction Attributed to CADD in Antimicrobial Lead Identification
| Discovery Stage | Traditional Timeline (Months) | CADD-Accelerated Timeline (Months) | Time Saved (%) | Key CADD Method |
|---|---|---|---|---|
| Target Identification & Validation | 6-12 | 3-6 | ~50% | Genomic mining, Comparative genomics |
| Hit Identification | 12-24 | 3-9 | 60-75% | Virtual Screening (VS), Pharmacophore Modeling |
| Lead Optimization | 18-36 | 12-24 | ~33% | Molecular Dynamics (MD), Free Energy Perturbation (FEP) |
| Total Preclinical Lead Discovery | 36-72 | 18-39 | ~45-50% | Integrated Workflow |
Table 2: Cost Avoidance in Preclinical R&D via CADD
| Cost Category | Estimated Cost (Traditional) | Estimated Cost (CADD-Integrated) | Savings/Avoidance | Rationale |
|---|---|---|---|---|
| Compound Screening (HTS) | $500,000 - $1,500,000 | $50,000 - $200,000 | Up to 85% | VS reduces physical compounds to test by 2-3 orders of magnitude. |
| Chemical Synthesis & SAR | $2,000,000+ | $1,000,000 - $1,500,000 | ~25-50% | FEP/MD prioritizes synthesis to highest-priority analogs. |
| Failed Lead Attrition | High (80-90% failure rate) | Reduced | Significant | Better early-stage prediction of ADMET/toxicity avoids late-stage failures. |
| Aggregate Preclinical Cost Per Candidate | >$3M | $1.5M - $2M | ~30-50% | Cumulative efficiency gains. |
Application Notes & Protocols
AN-01: Protocol for Structure-Based Virtual Screening (SBVS) Against a Novel Bacterial Target
Objective: To computationally screen >10 million compounds against the active site of a validated bacterial enzyme target (e.g., DNA gyrase, β-lactamase) to identify 50-100 high-priority hits for in vitro testing. Background: SBVS uses the 3D structure of a target to dock and score compounds from digital libraries, prioritizing those with optimal complementary interactions.
Protocol:
- Target Preparation:
- Obtain protein structure (PDB ID: e.g., 4DUH) from the RCSB PDB.
- Using Schrödinger Protein Preparation Wizard or UCSF Chimera:
- Add missing hydrogen atoms.
- Assign bond orders and correct protonation states (key histidine, aspartate, glutamate residues).
- Optimize hydrogen-bonding networks.
- Remove crystallographic water molecules, except those mediating key interactions.
- Generate receptor grid file centered on the active site co-crystallized ligand.
Ligand Library Preparation:
- Download purchasable compound library (e.g., ZINC20, Enamine REAL).
- Filter using rule-based methods (e.g., Lipinski’s Rule of 5, PAINS filters, lead-likeness).
- Prepare ligands: generate tautomers, stereoisomers, and low-energy 3D conformers using LigPrep or Open Babel.
Virtual Screening Execution:
- Step 1: High-Throughput Virtual Screening (HTVS): Dock filtered library using fast, less precise docking (e.g., Glide HTVS, Vina). Retain top 10% by docking score.
- Step 2: Standard Precision (SP) Docking: Re-dock retained hits with more rigorous scoring (e.g., Glide SP). Retain top 5%.
- Step 3: Extra Precision (XP) Docking: Final docking of top compounds with highest precision scoring function.
- Step 4: Post-Docking Analysis: Apply constraints (e.g., necessity of key hydrogen bond with catalytic residue). Cluster results by chemical similarity and visual inspection. Select 50-100 diverse, high-scoring compounds for purchase and biochemical assay.
Expected Outcome: Identification of novel chemotypes with inhibitory activity (IC50 < 50 µM) within 4-6 weeks of computational work, versus 6-12 months for an equivalent HTS campaign.
AN-02: Protocol for Lead Optimization Using Free Energy Perturbation (FEP)
Objective: To accurately predict the relative binding affinity (ΔΔG) of 20 analog series for a lead compound bound to a bacterial target, guiding synthetic efforts towards the most potent derivatives. Background: FEP calculations provide a rigorous, physics-based method to predict the impact of small chemical modifications on binding affinity.
Protocol:
- System Setup:
- Start from a high-resolution co-crystal structure of the lead-target complex.
- Solvate the system in an explicit water box (TIP3P) with neutralizing ions (Na+/Cl-) using Desmond System Builder.
- Parameterize ligands using the OPLS4 force field.
FEP Map Design:
- Design a graph of transformations connecting all 20 target analogs to the core lead molecule. Each "edge" represents a single, small chemical change (e.g., -H → -CH3, -OH → -OCH3).
- Use the Schrödinger FEP+ mapper to generate the perturbation network.
Simulation & Analysis:
- Run FEP simulations using a lambda-schedule of 12-16 λ windows per transformation.
- Perform 10 ns simulation per λ window in the NPT ensemble.
- Calculate ΔΔG values using the Multistate Bennett Acceptance Ratio (MBAR) method.
- Analyze results: Predict relative binding free energies with a typical target accuracy of <1.0 kcal/mol. Rank-order all analogs.
- Correlate predictions with available experimental IC50 data to validate the model.
Expected Outcome: Prioritize synthesis to the top 5 predicted analogs, increasing the likelihood of achieving a >10-fold potency improvement and reducing synthetic cycles by 50-70%.
Visualization of Workflows & Pathways
Title: Structure-Based Virtual Screening Protocol Workflow
Title: CADD Protocols within AMR Research Thesis Context
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents & Computational Tools for Featured Protocols
| Item/Tool Name | Provider/Example | Function in Protocol |
|---|---|---|
| Protein Data Bank (PDB) | RCSB PDB (rcsb.org) | Repository for 3D structural data of biological macromolecules. Source for target preparation. |
| Schrödinger Suite | Schrödinger, Inc. | Integrated software for protein prep (Maestro), docking (Glide), and FEP calculations (Desmond, FEP+). |
| ZINC / Enamine REAL Libraries | ZINC20, Enamine | Curated, commercially available virtual compound libraries for virtual screening. |
| UCSF Chimera | RBVI, UCSF | Open-source visualization and analysis tool for molecular structures. Used for initial inspection and analysis. |
| GROMACS | Open Source | High-performance MD package; can be used for FEP simulations as an open-source alternative. |
| PyMOL / PyMOL Molecular Viewer | Schrödinger, Inc. | Industry-standard molecular visualization system for rendering publication-quality images and analysis. |
| ADMET Prediction Tools | QikProp, SwissADME, pkCSM | Predict pharmacokinetic and toxicity profiles in silico to filter compounds early. |
| 96/384-Well Microplate | Corning, Thermo Fisher | Standard plate format for high-throughput biochemical assays (e.g., IC50 determination) of computational hits. |
| Recombinant Purified Enzyme | Academic Cores, Commercial (e.g., Sigma) | Target protein for in vitro enzymatic inhibition assays to validate computational hits. |
Conclusion
CADD has evolved from a supportive tool to a central driver in antimicrobial discovery, offering a strategic response to the escalating AMR crisis. By enabling the rational design of drugs against evolving targets, optimizing lead compounds for bacterial-specific challenges, and significantly accelerating the early discovery pipeline, CADD reduces the time and cost to identify novel candidates. Future success hinges on the integration of ever more sophisticated AI/ML models with high-quality experimental data, a collaborative open-science ethos for target and compound sharing, and a focus on polypharmacology and host-directed therapies. The path forward requires sustained investment in computational methodologies tailored to the unique biological and chemical landscape of antibacterial drug discovery to translate in silico promise into clinical reality.