How Machine Learning is Revolutionizing Biomarker Discovery: From Multi-Omics Integration to Clinical Validation
This article provides a comprehensive overview of the transformative impact of machine learning (ML) and artificial intelligence (AI) on biomarker discovery for researchers, scientists, and drug development professionals.
How Machine Learning is Revolutionizing Biomarker Discovery: From Multi-Omics Integration to Clinical Validation
Abstract
This article provides a comprehensive overview of the transformative impact of machine learning (ML) and artificial intelligence (AI) on biomarker discovery for researchers, scientists, and drug development professionals. It explores the foundational shift from single-analyte approaches to ML-driven analysis of complex multi-omics datasets, detailing key methodologies from feature selection to deep learning. The scope extends to practical applications across oncology, neurology, and infectious diseases, while critically addressing central challenges including data heterogeneity, model interpretability, and overfitting. Furthermore, the article outlines rigorous validation frameworks and comparative analyses of ML techniques essential for translating computational biomarkers into clinically validated tools for precision medicine, synthesizing current evidence and future directions in the field.
The New Paradigm: How AI is Redefining Biomarker Discovery
{LIMITATIONS OF SINGLE-FEATURE BIOMARKERS} The reliance on a single biological feature as a definitive classifier for disease state or treatment response introduces several critical vulnerabilities into the research and development pipeline. These limitations not only hinder clinical utility but also contribute to the high attrition rate of biomarker candidates [1].
Table 1: Key Limitations of Single-Feature Biomarker Approaches
| Limitation | Underlying Cause | Consequence |
|---|---|---|
| Inadequate Biological Reflection | Inability to capture disease heterogeneity, compensatory pathways, and complex tumor microenvironments [2]. | Suboptimal patient stratification, failure to predict treatment efficacy accurately, and inability to anticipate resistance mechanisms. |
| Limited Analytical Performance | Dependence on a single analytical signal, making the result vulnerable to pre-analytical and analytical variability [3]. | Poor reproducibility and reliability across different laboratories and sample types, leading to inconsistent clinical decisions. |
| Susceptibility to Confounding | The single feature may be a correlative rather than a causative factor, or influenced by unrelated biological processes [4] [5]. | High false-positive and false-negative rates, as seen with C-reactive protein in cardiovascular disease where levels are affected by obesity and other conditions [4]. |
| Restricted Clinical Utility | Provides a binary (positive/negative) result that often fails to inform on prognosis, disease subtype, or optimal therapy sequencing [6]. | Limited value in guiding complex treatment decisions in adaptive trial designs and personalized medicine strategies [2]. |
{QUANTITATIVE EVIDENCE AND CASE STUDIES} Empirical data and historical case studies underscore the practical challenges outlined in Table 1. The high failure rate of biomarker development is a testament to these issues; most discovered biomarkers never achieve clinical adoption [1]. A systematic analysis of biomarker success identified that robust clinical validity and utility are the most significant predictors of translation, areas where single-feature approaches are inherently weak [1]. The following case studies illustrate these points.
Table 2: Case Studies Highlighting Single-Feature Biomarker Challenges
| Biomarker & Disease Context | Documented Challenge | Impact on Clinical Application |
|---|---|---|
| HER2 in Breast Cancer [3] | Ongoing debate regarding optimal assay methodology (IHC vs. FISH) and efficacy of targeted therapy in patients with low HER2 expression [3]. | Continuous refinement of testing guidelines and potential denial of effective therapy to a subset of patients. |
| EGFR in Colorectal & Lung Cancer [3] | EGFR protein expression by IHC fails to reliably predict response to EGFR inhibitors; other features (KRAS mutations, EGFR amplification) are critical. | Initial patient selection based on a single feature (EGFR IHC) was suboptimal, requiring subsequent incorporation of additional biomarkers. |
| C-Reactive Protein (CRP) in Cardiovascular Disease [4] | Disputed causal relationship; levels are confounded by factors like obesity and physical activity, complicating interpretation [4]. | Significant confusion regarding its role as a risk predictor versus a consequence of disease, limiting its standalone utility. |
{EXPERIMENTAL PROTOCOLS FOR EVALUATING BIOMARKER LIMITATIONS} To systematically evaluate the performance and limitations of a candidate single-feature biomarker, the following protocols provide a standardized methodological framework.
Protocol 1: Assessing Biomarker Specificity in a Heterogeneous Population
- Objective: To determine the false positive rate of a candidate biomarker by testing its presence in non-disease control populations and in tissues/cells with confounding conditions.
- Materials:
- Research Reagent Solutions: See Table 4 for essential materials.
- Sample Sets: Banked tissue sections, serum/plasma samples, or cell line lysates from (a) confirmed disease-positive patients, (b) healthy controls, and (c) patients with pathologically similar or confounding conditions (e.g., other cancer types, inflammatory diseases).
- Methodology:
- Sample Processing: Execute standardized protocols for nucleic acid extraction (for genomic biomarkers) or protein extraction (for proteomic biomarkers) from all sample sets.
- Assay Performance: Analyze all samples using the designated platform for the candidate biomarker (e.g., qPCR for DNA/RNA, immunohistochemistry for protein).
- Data Analysis: Calculate sensitivity, specificity, and positive predictive value. A high false positive rate in control groups (c) indicates low specificity and high susceptibility to confounding.
Protocol 2: Evaluating Dynamic Range and Quantitative Correlation
- Objective: To establish whether the biomarker's level quantitatively correlates with disease severity or drug response, moving beyond a binary positive/negative readout.
- Materials:
- Research Reagent Solutions: Refer to Table 4.
- Sample Sets: A longitudinal series of samples from the same patient (pre-treatment, on-treatment, progression) or a cohort with well-defined, graded disease severity.
- Methodology:
- Quantitative Assay: Employ a quantitative or semi-quantitative assay (e.g., quantitative RT-PCR, ELISA, RNA-Seq, targeted mass spectrometry).
- Standard Curve Generation: For analytical methods like ELISA, include a standard curve with known concentrations of the analyte to ensure accurate quantification.
- Correlation Analysis: Statistically correlate the quantitative level of the biomarker with clinical endpoints (e.g., tumor size, survival time, pathological grade). A weak correlation suggests limited prognostic or predictive power.
{VISUALIZING THE CONCEPTUAL SHIFT} The following diagrams, generated with Graphviz, illustrate the core conceptual limitations of the single-feature approach and the logical pathway for its evaluation.
Diagram 1: Single-feature versus multi-feature biomarker models.
Diagram 2: Tumor heterogeneity confounding single-feature assays.
Diagram 3: Logical workflow for evaluating single-feature biomarker limitations.
{THE SCIENTIST'S TOOLKIT: RESEARCH REAGENT SOLUTIONS} Successful execution of the experimental protocols requires standardized, high-quality reagents and platforms. The following table details essential materials for biomarker evaluation studies.
Table 4: Essential Research Reagents and Platforms for Biomarker Evaluation
| Reagent / Platform | Function | Application Example |
|---|---|---|
| Formalin-Fixed, Paraffin-Embedded (FFPE) Tissue Sections | Preserves tissue morphology and biomolecules for retrospective histological and molecular analysis. | Immunohistochemistry (IHC) for protein biomarker localization and semi-quantification [3]. |
| Validated Antibodies (Monoclonal/Polyclonal) | Highly specific binding to target antigen for detection and quantification. | HercepTest (anti-HER2 antibody) for IHC-based stratification for trastuzumab therapy [3]. |
| Fluorescence In Situ Hybridization (FISH) Probes | Labeled nucleic acid sequences for detecting specific gene loci or chromosomal abnormalities. | PathVysion HER2 DNA Probe Kit for determining HER2 gene amplification status [3]. |
| Next-Generation Sequencing (NGS) Panels | High-throughput, parallel sequencing of multiple genes or entire genomes/transcriptomes. | Identifying co-occurring mutations (e.g., KRAS, NRAS) in colorectal cancer to predict resistance to EGFR therapy [3] [7]. |
| Liquid Biopsy Collection Tubes | Stabilizes cell-free DNA and other analytes in blood samples for non-invasive biomarker analysis. | Isolation of circulating tumor DNA (ctDNA) for dynamic monitoring of tumor burden and resistance mutations [7]. |
| Digital Biomarker Discovery Pipelines (e.g., DBDP) | Open-source computational toolkits for standardized processing of digital health data (e.g., from wearables) [8]. | Extracting features like heart rate variability from ECG data as a digital biomarker for cardiovascular risk [8]. |
{CONCLUSION} The evidence demonstrates that traditional single-feature biomarker approaches are fundamentally constrained in their ability to navigate the complex biological networks underlying human disease. The protocols and visualizations provided herein offer a systematic pathway for researchers to empirically validate these limitations within their specific contexts. The consistent failure of such narrow approaches to achieve clinical translation [1] underscores the necessity for a paradigm shift. The future of biomarker discovery lies in integrated multi-omics data and machine learning models capable of identifying complex, multi-analyte signatures that more accurately reflect disease biology and power the next generation of personalized medicine [4] [2] [9].
{ARTICLE CONTENT END}
Biomarkers are defined characteristics measured as indicators of normal biological processes, pathogenic processes, or responses to an exposure or intervention [10]. In precision medicine, biomarkers facilitate accurate diagnosis, risk stratification, disease monitoring, and personalized treatment decisions by tailoring therapies to individual genetic, environmental, and lifestyle factors [11]. The joint FDA-NIH Biomarkers, EndpointS, and other Tools (BEST) resource establishes standardized definitions to ensure clarity across research and clinical practice [10]. This document delineates the core definitions and applications of diagnostic, prognostic, and predictive biomarkers, contextualized within modern machine learning-driven discovery frameworks.
Core Biomarker Definitions and Applications
Biomarkers are categorized based on their specific clinical applications. Understanding the distinctions between these categories is essential for appropriate use in both research and clinical decision-making [10] [12].
Table 1: Core Biomarker Types, Definitions, and Applications
| Biomarker Type | Definition | Primary Application | Representative Examples |
|---|---|---|---|
| Diagnostic | Detects or confirms the presence of a disease or condition of interest [10]. | Disease identification and classification [10]. | PSA for prostate cancer screening; Troponin for acute myocardial infarction [10] [12]. |
| Prognostic | Provides information on the overall disease outcome, including the risk of recurrence or progression, regardless of therapy [13] [14]. | Informing disease management strategies and patient counseling on likely disease course [14] [15]. | Oncotype DX and MammaPrint assays for estimating breast cancer recurrence risk [14] [12]. |
| Predictive | Identifies individuals who are more likely to experience a favorable or unfavorable effect from a specific therapeutic intervention [13] [14]. | Guiding treatment selection to optimize efficacy and avoid ineffective therapies [14] [12]. | HER2 overexpression predicting response to trastuzumab in breast cancer; EGFR mutations predicting response to gefitinib in lung cancer [13] [14] [12]. |
A critical conceptual distinction is that a prognostic biomarker informs on the aggressiveness of a disease, while a predictive biomarker informs on the effectiveness of a specific therapy [12]. A single biomarker can serve both prognostic and predictive roles, though evidence must be developed for each context of use [10] [14].
Experimental Protocols for Biomarker Validation
Analytical Validation
Before clinical utility can be assessed, a biomarker assay must undergo rigorous analytical validation to prove technical robustness [12]. This process is the focus of Clinical Laboratory Improvement Amendments (CLIA) regulations and involves evaluating several key parameters [12].
Table 2: Key Parameters for Biomarker Analytical Validation
| Parameter | Definition | Experimental Protocol |
|---|---|---|
| Accuracy | The degree to which the measured value reflects the true value [12]. | Compare results from the new assay against a gold-standard reference method using a panel of known positive and negative samples. Calculate percent agreement or correlation coefficients [12]. |
| Precision | The closeness of agreement between independent measurement results obtained under stipulated conditions [12]. | Run replicate measurements of the same sample across multiple days, by different operators, and using different instrument lots. Report results as coefficients of variation (CV) [12]. |
| Analytical Sensitivity | The lowest amount of the biomarker that can be reliably distinguished from zero [12]. | Perform serial dilutions of a sample with a known concentration of the biomarker. The limit of detection (LoD) is the lowest concentration consistently detected in ≥95% of replicates [12]. |
Clinical Validation and Statistical Assessment
Clinical validation provides proof that the biomarker is fit for its intended clinical purpose [12]. This requires testing the biomarker in a patient population entirely distinct from the discovery cohort to avoid overfitting [13] [12].
Key Statistical Considerations and Protocols:
- Study Power and Design: The intended use and target population must be defined early. For prognostic biomarkers, retrospective studies with prospectively collected biospecimens from a cohort representing the target population are often used. Predictive biomarkers, however, must be identified through secondary analyses of randomized clinical trials, testing for a statistically significant interaction between the treatment and the biomarker in a statistical model [13].
- Minimizing Bias: Implement randomization during specimen analysis to control for batch effects and non-biological experimental variations. Blinding should be used to keep laboratory personnel unaware of clinical outcomes during biomarker data generation [13].
- Performance Metrics: The analytical plan must be pre-specified prior to data analysis. Performance is quantitatively assessed using metrics tailored to the biomarker's purpose [13]:
- Sensitivity: Proportion of true cases correctly identified.
- Specificity: Proportion of true controls correctly identified.
- Receiver Operating Characteristic (ROC) Curve and Area Under the Curve (AUC): Plots sensitivity vs. (1-specificity) across all thresholds, with AUC providing a measure of overall discriminative ability [13].
- Positive/Negative Predictive Values (PPV/NPV): Proportion of test-positive/negative patients who truly have/do not have the disease or outcome, dependent on disease prevalence [13].
Machine Learning in Biomarker Discovery
Traditional single-feature biomarker discovery faces challenges with reproducibility and capturing disease complexity. Machine learning (ML) addresses these by integrating large, complex multi-omics datasets to identify reliable biomarkers [11].
ML Applications by Biomarker Type
Table 3: Machine Learning Applications for Biomarker Discovery
| Biomarker Type | ML Application | Exemplary Study |
|---|---|---|
| Diagnostic | Classifying disease status based on molecular profiles [11] [4]. | Using transcriptomic data from rheumatoid arthritis patients, an ML pipeline (including PCA and t-SNE for visualization) demonstrated clear separation between patients and controls [4]. |
| Prognostic | Forecasting disease progression and patient stratification [11] [15]. | In multiple myeloma, ML models integrate genetic, transcriptomic, and imaging data to identify high-risk patients, moving beyond traditional staging systems like R-ISS [15]. |
| Predictive | Estimating response to specific therapies [11] [16]. | A study predicting Large-Artery Atherosclerosis (LAA) integrated clinical factors and metabolite profiles. A logistic regression model achieved an AUC of 0.92, identifying predictive features like smoking status and lipid metabolites [16]. |
Standard ML Workflow Protocol
A typical ML workflow for biomarker discovery involves:
- Data Preprocessing: Handling missing data (e.g., mean imputation), label encoding, and participant grouping. Data is typically split into training/validation (e.g., 80%) and external testing (e.g., 20%) sets [16].
- Exploratory Data Analysis and Feature Selection: Using unsupervised learning techniques like Principal Component Analysis (PCA) and t-distributed Stochastic Neighbor Embedding (t-SNE) to visualize data structure, identify outliers, and understand group dynamics [4]. Recursive feature elimination is then used to identify the most informative biomarkers and reduce overfitting [16].
- Model Training and Validation: Training multiple supervised learning models (e.g., Logistic Regression, Support Vector Machines, Random Forests, XGBoost) on the training set using tenfold cross-validation. Model performance is evaluated on the held-out test set using metrics like AUC [16].
- Interpretation and Validation: Using explainable AI (XAI) techniques to interpret model predictions and identify features driving the classification. Biomarkers identified computationally must subsequently undergo rigorous wet-lab validation to ensure clinical reliability [11] [4].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Platforms for Biomarker Discovery
| Reagent/Platform | Function | Application Context |
|---|---|---|
| Absolute IDQ p180 Kit | A targeted metabolomics kit that quantifies 194 endogenous metabolites from 5 compound classes [16]. | Used in the LAA study for plasma metabolite profiling to identify biomarkers linked to aminoacyl-tRNA biosynthesis and lipid metabolism [16]. |
| Next-Generation Sequencing (NGS) | High-throughput technology for comprehensive genomic, transcriptomic, and epigenomic profiling [13] [17]. | Identifies mutations, gene rearrangements, and differential gene expression as candidate biomarkers in oncology and other diseases [13] [17]. |
| Liquid Biopsy Assays | Minimally invasive analysis of circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and other blood-based biomarkers [13] [17]. | Used for cancer diagnosis, monitoring therapeutic response, and detecting minimal residual disease via ctDNA analysis [13] [17]. |
| Waters Acquity Xevo TQ-S | Tandem mass spectrometry instrument for highly sensitive and specific quantification of small molecules [16]. | Coupled with the Biocrates kit for precise measurement of metabolite concentrations in biomarker discovery studies [16]. |
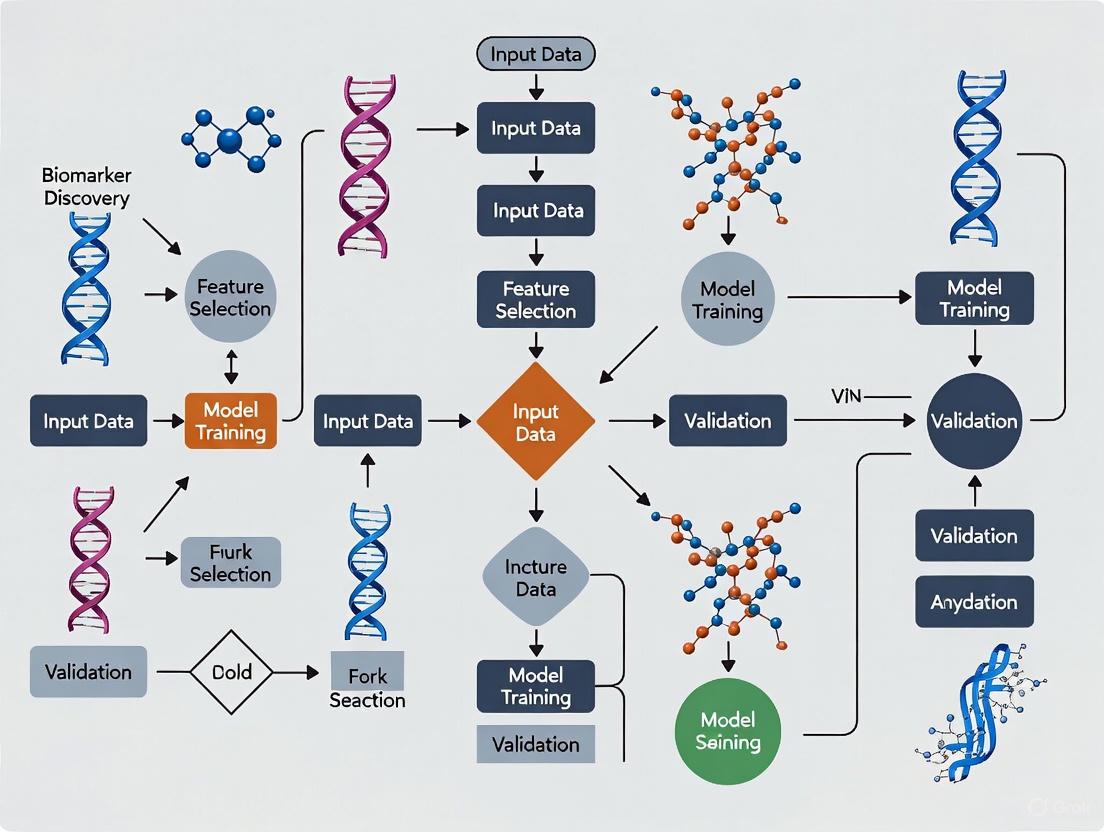
Workflow Visualization
Biomarker Development Pipeline
The journey from discovery to clinical application is long and requires multiple, rigorous stages [12] [17].
ML-Driven Discovery Workflow
Machine learning reshapes the initial discovery and validation phases, enabling integration of complex, high-dimensional data [11] [4] [16].
The Role of Machine Learning in Integrating Multi-Omics Data (Genomics, Proteomics, Metabolomics)
The complexity of biological systems necessitates moving beyond single-layer analyses to a more holistic approach. Multi-omics integrates data from various molecular levels—including genomics, transcriptomics, proteomics, epigenomics, and metabolomics—to provide a comprehensive view of biological processes and disease mechanisms [18] [19]. This approach is revolutionizing biomedical research by enabling the identification of comprehensive biomarker signatures and providing insights into disease etiology and potential treatment targets that would remain elusive with single-omics studies [19].
Machine learning (ML) has emerged as a critical enabler for multi-omics integration, addressing significant challenges inherent in these complex datasets. Traditional statistical models often struggle with the high dimensionality, heterogeneity, and noise characteristic of multi-omics data [20]. ML algorithms, particularly deep learning models, can effectively handle these challenges by identifying complex, non-linear patterns across different biological layers, thereby revealing hidden connections and improving disease prediction capabilities [9] [20]. This integration is especially valuable in precision medicine, where it supports disease diagnosis, prognosis, personalized treatments, and therapeutic monitoring [9].
Machine Learning Approaches for Multi-Omics Data Integration
Categories of Integration Strategies
Machine learning approaches for multi-omics integration can be categorized based on how and when the data fusion occurs during the analytical process. The selection of an appropriate integration strategy depends on the specific research objectives, data characteristics, and computational resources available [21].
Table 1: Machine Learning Integration Strategies for Multi-Omics Data
| Integration Strategy | Description | Advantages | Limitations | Common Algorithms |
|---|---|---|---|---|
| Early Integration | Concatenates all omics datasets into a single matrix before analysis [21]. | Simple to implement; captures cross-omics correlations immediately [21]. | High dimensionality and noise; ignores data structure differences [21]. | Support Vector Machines (SVM), Random Forests [22]. |
| Intermediate Integration | Learns joint representations from multiple omics datasets simultaneously [23] [21]. | Balances data specificity and integration; effectively captures inter-omics interactions [21]. | Requires robust pre-processing; complex model implementation [21]. | Multiple Kernel Learning, MOFA, Deep Learning Autoencoders [20]. |
| Late Integration | Analyzes each omics dataset separately and combines the results or predictions at the final stage [21]. | Avoids challenges of direct data fusion; utilizes domain-specific models [21]. | Does not directly capture inter-omics interactions [21]. | Ensemble Methods, Voting Classifiers [22]. |
| Network-Based Integration | Utilizes biological networks to contextualize and integrate multi-omics data [24]. | Incorporates prior biological knowledge; provides biological context for findings [24]. | Dependent on quality and completeness of network databases [24]. | Graph Neural Networks, Network Propagation [24]. |
Deep Learning Architectures for Multi-Omics
Deep learning has become increasingly prominent in multi-omics research due to its ability to model complex, non-linear relationships in high-dimensional data [20]. These models can be broadly divided into two categories:
Non-generative models include architectures such as feedforward neural networks (FFNs), graph convolutional networks (GCNs), and autoencoders, which are designed to extract features and perform classification directly from the input data [20]. For instance, convolutional neural networks (CNNs) have been applied to multi-omics classification tasks, while recurrent neural networks (RNNs) like CNN-BiLSTM can model sequential dependencies in omics data [25].
Generative models, including variational autoencoders (VAEs), generative adversarial networks (GANs), and generative pretrained transformers (GPTs), focus on creating adaptable representations that can be shared across multiple modalities [20]. These approaches are particularly valuable for handling missing data and dimensionality challenges, often outperforming traditional methods [20].
Computational Framework and Workflow
Implementing a successful machine learning pipeline for multi-omics data requires a systematic approach that addresses the unique characteristics of biological datasets. The following workflow outlines the key stages in this process.
Data Preprocessing and Quality Control
The initial preprocessing stage is critical for ensuring data quality and analytical robustness. Key steps include:
Normalization and Batch Effect Correction: Technical variations across different sequencing platforms, laboratory conditions, or sample processing batches can introduce significant artifacts. Methods such as Harmony analysis are employed to mitigate batch effects and ensure that biological signals rather than technical variations drive the analytical results [26]. Normalization techniques must be appropriately selected for each omics layer to account for differences in data distribution and scale [21].
Missing Value Imputation: Omics datasets frequently contain missing values due to various technical and biological reasons. specialized imputation processes are required to infer these missing values before statistical analyses can be applied [21]. Techniques range from simple mean/median imputation to more sophisticated K-nearest neighbors (KNN) or matrix factorization methods, with the choice dependent on the missing data mechanism and proportion.
Dimensionality Reduction and Feature Selection: The "high-dimension low sample size" (HDLSS) problem, where variables significantly outnumber samples, can cause ML algorithms to overfit, reducing their generalizability [21]. Feature selection methods (e.g., variance filtering, LASSO) and dimensionality reduction techniques (e.g., PCA, UMAP) help address this challenge by focusing on the most biologically relevant features [26].
Machine Learning Model Training and Validation
Following data preprocessing, the ML model development phase involves:
Model Selection and Training: The choice of algorithm depends on the research objective, data characteristics, and sample size. For example, in a schizophrenia study comparing 17 machine learning models, LightGBMXT achieved superior performance for multi-omics classification with an AUC of 0.9727, outperforming other models including CNN-BiLSTM [25]. Ensemble methods often demonstrate strong performance in multi-omics applications.
Validation and Generalizability Assessment: Rigorous validation is essential to ensure model robustness. This includes internal validation through techniques such as k-fold cross-validation and external validation on independent datasets [9]. Performance metrics should be selected based on the specific application—AUC-ROC for classification tasks, C-index for survival analysis, or mean squared error for continuous outcomes.
Experimental Protocols for Multi-Omics Studies
Protocol 1: Multi-Omics Biomarker Discovery for Disease Classification
This protocol outlines the procedure for identifying integrative biomarkers for disease classification, adapted from a study on schizophrenia [25].
Sample Preparation and Data Generation:
- Cohort Selection: Recruit a well-characterized cohort of case and control participants (e.g., 104 individuals total) with matched clinical phenotypes [25].
- Sample Collection: Collect peripheral blood samples in EDTA tubes and isolate plasma through centrifugation at 2,000 × g for 10 minutes at 4°C.
- Multi-Omics Data Generation:
- Proteomics: Process plasma samples using liquid chromatography-mass spectrometry (LC-MS/MS) with isobaric labeling (TMT or iTRAQ) for protein quantification. Include post-translational modification (PTM) analysis through enrichment protocols.
- Metabolomics: Perform untargeted metabolomic profiling using LC-MS in both positive and negative ionization modes.
Data Preprocessing:
- Proteomics Data: Normalize protein abundances using quantile normalization, impute missing values with KNN imputation, and log2-transform the data.
- Metabolomics Data: Perform peak alignment, retention time correction, and compound identification using reference standards. Normalize to total ion count.
- Data Integration: Merge proteomics, PTM, and metabolomics datasets using shared sample identifiers, ensuring proper alignment of samples across platforms.
Machine Learning Analysis:
- Feature Pre-selection: Apply false discovery rate (FDR) correction (e.g., FDR < 0.05) and retain features with significant differential abundance between cases and controls.
- Model Training: Implement multiple machine learning algorithms (e.g., LightGBMXT, Random Forest, SVM, CNN-BiLSTM) using a standardized framework. Utilize automated machine learning (AutoML) to optimize hyperparameters.
- Model Validation: Perform 100 iterations of 5-fold cross-validation, evaluating performance using AUC-ROC, precision, recall, and F1-score.
- Biomarker Interpretation: Apply feature importance analysis (e.g., SHAP values) to identify top discriminative features. Conduct functional enrichment analysis on prioritized biomarkers using databases like GO, KEGG, and Reactome.
Protocol 2: Network-Based Multi-Omics Integration for Drug Target Identification
This protocol utilizes network biology approaches to identify novel drug targets from multi-omics data, based on methodologies from network-based multi-omics integration studies [24].
Data Collection and Processing:
- Multi-Omics Data Acquisition: Collect genomic (DNA sequencing), transcriptomic (RNA-seq), and proteomic (LC-MS/MS) data from patient samples and public repositories (e.g., TCGA, CPTAC) [24] [26].
- Molecular Network Construction:
- Download protein-protein interaction (PPI) networks from curated databases (e.g., STRING, BioGRID).
- Construct gene co-expression networks using WGCNA on transcriptomics data.
- Integrate pathway information from KEGG, Reactome, and WikiPathways.
Network-Based Integration:
- Multi-Layer Network Construction: Create an integrated network with nodes representing biomolecules (genes, proteins) and edges representing interactions from different omics layers and databases.
- Network Propagation: Apply network propagation algorithms (e.g., Random Walk with Restart) to diffuse molecular alterations (e.g., mutations, expression changes) through the integrated network.
- Module Detection: Identify densely connected network modules exhibiting significant alterations across multiple omics layers using community detection algorithms (e.g., Louvain method).
Target Prioritization and Validation:
- Target Scoring: Develop a multi-parametric scoring system incorporating network centrality, cross-omics alteration frequency, functional essentiality, and druggability predictions.
- Experimental Validation: Select top-ranked targets for functional validation using CRISPR knockdown, organoid models, or high-content screening assays.
- Therapeutic Response Prediction: Integrate drug-target interaction networks with multi-omics profiles to predict drug response and identify potential repurposing opportunities [24].
The Scientist's Toolkit: Essential Research Reagents and Computational Tools
Successful implementation of multi-omics studies with machine learning integration requires both wet-lab reagents and computational resources.
Table 2: Essential Research Reagents and Computational Tools for Multi-Omics Studies
| Category | Specific Tools/Reagents | Function/Application | Key Features |
|---|---|---|---|
| Wet-Lab Reagents | DNA polymerases, dNTPs, oligonucleotide primers [19] | Genomics, epigenomics, and transcriptomics analyses | Fundamental components for PCR-based amplification |
| Reverse transcriptases, cDNA synthesis kits [19] | Transcriptomics: conversion of RNA to cDNA | Enable gene expression analysis via RT-PCR and qPCR | |
| Methylation-sensitive restriction enzymes [19] | Epigenomics: DNA methylation studies | Detect and analyze reversible DNA modifications | |
| Mass spectrometry kits and reagents [19] | Proteomics and metabolomics profiling | Identify and quantify proteins and metabolites | |
| Computational Tools | Python/R ML libraries (scikit-learn, TensorFlow) [9] | Implementation of machine learning models | Provide algorithms for classification, regression, clustering |
| Multi-omics integration tools (MOFA, mixOmics) [23] | Integration of multiple omics datasets | Specialized methods for combining different data types | |
| Biological network analysis (Cytoscape, NetworkX) [24] | Construction and analysis of molecular networks | Visualize and analyze complex biological interactions | |
| Single-cell analysis tools (Seurat, Scanpy) [26] | Analysis of single-cell RNA sequencing data | Process and interpret single-cell resolution data |
Case Study: Schizophrenia Biomarker Discovery Through Multi-Omics Integration
A recent study demonstrated the power of AI-driven multi-omics integration for identifying peripheral biomarkers for schizophrenia risk stratification [25]. The research utilized an open-access dataset comprising plasma proteomics, post-translational modifications (PTMs), and metabolomics data from 104 individuals.
Experimental Workflow and Key Findings: The researchers applied a comprehensive machine learning framework with 17 different algorithms, finding that multi-omics integration significantly enhanced classification performance compared to single-omics approaches. The best-performing model (LightGBMXT) achieved an AUC of 0.9727, outperforming models using proteomics data alone [25].
Interpretable feature prioritization identified specific molecular events as key discriminators, including:
- Carbamylation at immunoglobulin-constant region sites IGKCK20 and IGHG1K8
- Oxidation of coagulation factor F10 at residue M8 [25]
Functional analyses revealed significantly enriched pathways including complement activation, platelet signaling, and gut microbiota-associated metabolism. Protein interaction networks further implicated coagulation factors (F2, F10, PLG) and complement regulators (CFI, C9) as central molecular hubs [25].
Biological Implications and Clinical Relevance: The study revealed an immune-thrombotic dysregulation as a critical component of schizophrenia pathology, with PTMs of immune proteins serving as quantifiable disease indicators [25]. This integrative approach delineated a robust computational strategy for incorporating multi-omics data into psychiatric research, providing biomarker candidates for future diagnostic and therapeutic applications.
Visualization of Molecular Interactions and Pathways
Understanding the complex interactions between identified biomarkers and their functional pathways is essential for biological interpretation. The following diagram illustrates a representative immune-coagulation network identified in the schizophrenia multi-omics study [25].
Challenges and Future Directions
Despite significant advancements, several challenges remain in the application of machine learning to multi-omics integration. Key limitations include:
Data Quality and Heterogeneity: The inherent heterogeneity of omics data comprising varied datasets with different distributions and types presents significant integration challenges [21]. Additionally, issues of missing data and batch effects require specialized preprocessing approaches that can impact downstream analyses [20] [21].
Model Interpretability and Biological Validation: Many advanced machine learning models, particularly deep learning approaches, function as "black boxes" with limited interpretability [9]. The development of explainable AI (XAI) methods is crucial for translating computational findings into biologically meaningful insights [9] [23]. Furthermore, computational predictions require experimental validation through techniques such as knockdown experiments, organoid models, or clinical correlation studies [22].
Regulatory and Ethical Considerations: The clinical implementation of AI-driven multi-omics approaches requires careful attention to regulatory requirements and ethical considerations, particularly regarding patient data privacy and algorithmic bias [9]. Establishing standards for trustworthy AI in biomedical research is essential for clinical adoption [9].
Future developments in the field will likely focus on incorporating temporal and spatial dynamics through technologies such as single-cell sequencing and spatial transcriptomics [26], improving model interpretability through explainable AI techniques, and establishing standardized evaluation frameworks for comparing different integration methods [24]. As these technologies mature, machine learning-powered multi-omics integration will play an increasingly central role in precision medicine, biomarker discovery, and therapeutic development.
Performance Benchmarks of ML-Driven Biomarker Discovery
Table 1: Performance Metrics of ML Models for Biomarker Discovery Across Diseases
| Disease Area | ML Model(s) Used | Biomarker Type / Purpose | Key Performance Metrics | Reference / Context |
|---|---|---|---|---|
| Oncology | Random Forest, XGBoost | Predictive biomarkers for targeted cancer therapeutics | LOOCV Accuracy: 0.7 - 0.96 | [27] |
| Ovarian Cancer | Ensemble Methods (RF, XGBoost) | Diagnostic biomarkers (e.g., CA-125, HE4 panels) | AUC > 0.90; Accuracy up to 99.82% | [28] |
| Alzheimer's Disease (AD) | Random Forest | Digital plasma spectra for AD vs. Healthy Controls | AUC: 0.92, Sensitivity: 88.2%, Specificity: 84.1% | [29] |
| Mild Cognitive Impairment (MCI) | Random Forest | Digital plasma spectra for MCI vs. Healthy Controls | AUC: 0.89, Sensitivity: 88.8%, Specificity: 86.4% | [29] |
| Infectious Diseases | Explainable AI, Ensemble Learning | Surveillance, diagnosis, and prognosis | High accuracy in prediction (Specific metrics vary by study) | [30] |
Detailed Experimental Protocols
Protocol for Predictive Biomarker Discovery in Oncology
This protocol outlines the process for using machine learning to identify protein-based predictive biomarkers for targeted cancer therapies, based on the MarkerPredict framework [27].
1. Data Acquisition and Network Construction
- Signaling Networks: Obtain protein-protein interaction data from dedicated signaling networks. The MarkerPredict study used the Human Cancer Signaling Network (CSN), SIGNOR, and ReactomeFI [27].
- Protein Disorder Data: Compile intrinsic disorder predictions for proteins using databases like DisProt and prediction tools such as IUPred and AlphaFold (using pLDDT scores) [27].
- Biomarker Annotation: Gather known biomarker data from text-mining databases like CIViCmine to create labeled training data [27].
2. Training Set Construction
- Positive Controls: Create a set of protein pairs where one protein is a known predictive biomarker for a drug targeting the other protein in the pair [27].
- Negative Controls: Create a set of protein pairs where the neighbor protein is not listed as a predictive biomarker in the annotation database [27].
3. Feature Extraction For each target-neighbor protein pair, extract the following features for ML model training:
- Network Topological Features: Calculate properties related to the protein's position and role within the signaling network (e.g., motif characteristics, centrality measures) [27].
- Motif Participation: Identify if the protein pair participates in specific three-nodal network motifs (triangles), which indicate close regulatory connections [27].
- Protein Disorder: Integrate metrics on intrinsic protein disorder for the neighbor protein [27].
4. Machine Learning Model Training and Validation
- Algorithm Selection: Employ tree-based ensemble algorithms such as Random Forest and XGBoost, which offer a balance between performance and interpretability [27].
- Model Validation: Perform rigorous validation using Leave-One-Out-Cross-Validation (LOOCV) and k-fold cross-validation to assess model accuracy and prevent overfitting [27].
- Biomarker Probability Score (BPS): Define a normalized score that aggregates the results from multiple models to rank potential predictive biomarkers [27].
5. Downstream Validation
- Experimental Validation: Prioritize high-ranking biomarker candidates for validation in wet-lab experiments using cell lines, organoids, or patient-derived samples [2] [27].
- Clinical Correlation: Investigate the correlation of candidate biomarkers with treatment response and patient outcomes in clinical datasets or trials [27].
Protocol for Digital Biomarker Discovery in Neurodegenerative Diseases
This protocol details a methodology for developing low-cost, machine learning-based digital biomarkers from blood plasma for Alzheimer's Disease (AD) and mild cognitive impairment (MCI), adapted from a 2025 validation study [29].
1. Participant Recruitment and Cohort Definition
- Recruit well-characterized participants across multiple cohorts: Amyloid-beta positive AD patients, patients with MCI, patients with other neurodegenerative diseases (e.g., DLB, FTD, PSP) for differential diagnosis, and healthy controls (HCs) [29].
- Conduct neuropsychological assessments (e.g., MMSE, MoCA) and confirm AD pathology via CSF analysis or PiB-PET imaging where feasible [29].
2. Sample Collection and Spectral Data Acquisition
- Collect plasma samples from all participants using standardized, minimally invasive venipuncture procedures [29].
- Spectral Analysis: Analyze plasma samples using Attenuated Total Reflectance-Fourier Transform Infrared (ATR-FTIR) spectroscopy to generate distinct spectral fingerprints. This technique examines functional groups and molecular conformations associated with proteins, lipids, and nucleic acids [29].
- (Optional) Measure traditional plasma biomarkers (e.g., p-tau217, GFAP, Aβ42) using technologies like Single Molecule Immune Detection (SMID) for subsequent correlation analysis [29].
3. Data Preprocessing and Feature Selection
- Preprocess spectral data to correct for baseline effects and normalize across samples [29].
- Digital Biomarker Selection: Use a Random Forest classifier in conjunction with feature selection procedures to identify the most informative spectral features (wavenumbers or peaks) that serve as digital biomarkers for distinguishing patient groups [29].
4. Machine Learning Model Development
- Train the Random Forest model using the selected digital biomarker panel to perform binary classifications (e.g., AD vs. HC, AD vs. DLB) [29].
- Validate model performance on independent validation cohorts to ensure generalizability. Report standard metrics including Area Under the Curve (AUC), sensitivity, and specificity [29].
5. Model Interpretation and Biological Correlation
- Analyze the correlation between the identified spectral digital biomarkers and concentrations of established pathological plasma biomarkers (e.g., p-tau217, GFAP) to provide a biological interpretation for the ML model's decisions [29].
Protocol for Biomarker Discovery in Infectious Disease Management
This protocol provides a general workflow for applying ML to identify biomarkers for infectious disease surveillance, diagnosis, and prognosis, synthesized from a 2025 scoping review [30].
1. Problem Definition and Data Source Identification
- Define the specific clinical objective: surveillance (outbreak prediction), diagnosis (pathogen or disease identification), or prognosis (predicting disease severity or outcome) [30].
- Identify and gather relevant multimodal data sources. These can include:
- Clinical Data: Electronic Health Records (EHRs), vital signs, laboratory results [30].
- Omics Data: Genomic, transcriptomic, or proteomic data from host or pathogen [30].
- Epidemiological Data: Public health reports, web surveillance data, phylogenetic trees [30].
- Other Data: Medical imaging (e.g., chest X-rays) or biomarker test results [30].
2. Data Preprocessing and Feature Engineering
- Clean the data by handling missing values and normalizing or standardizing features.
- Perform feature engineering to create informative inputs for the models. For heterogeneous data, dimensionality reduction techniques (e.g., PCA) may be necessary [30].
3. Model Selection and Training
- Select appropriate ML algorithms based on the data type and clinical question. The review suggests Explainable AI (XAI) and Ensemble Learning models are broadly applicable and achieve high accuracy [30].
- Model Candidates:
- Train the models on a dedicated training set, using techniques like cross-validation to tune hyperparameters [30].
4. Model Validation and Implementation
- Rigorous Validation: Test the final model on a held-out test set and, crucially, on independent external cohorts to assess generalizability and avoid biases present in the training data [30].
- Clinical Workflow Integration: Develop an actionable workflow for integrating the model into clinical practice to complement and augment clinical decision-making [30].
Workflow Visualization
Predictive Biomarker Discovery in Oncology
Digital Biomarker Workflow for Neurodegenerative Diseases
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for ML-Driven Biomarker Discovery
| Tool / Resource | Function / Application | Specific Examples / Notes |
|---|---|---|
| SomaScan Platform | High-throughput proteomic discovery; measures thousands of proteins simultaneously in biofluids. | Used by the Global Neurodegeneration Proteomics Consortium (GNPC) on ~35,000 samples [31]. |
| Olink & Mass Spectrometry | Complementary proteomic platforms for biomarker verification and validation. | Used by GNPC for cross-platform comparison and validation of SomaScan findings [31]. |
| ATR-FTIR Spectroscopy | Label-free biosensor generating digital spectral fingerprints from plasma/serum. | Identifies molecular-level changes for digital biomarker creation in neurodegenerative diseases [29]. |
| Spatial Biology Platforms | Enables in-situ analysis of biomarker distribution and cell interactions within tissue context. | Critical for characterizing the tumor microenvironment (TME) in oncology [2]. |
| Organoids & Humanized Models | Advanced disease models that recapitulate human biology for functional biomarker validation. | Used for screening functional biomarkers and studying therapy response in immunooncology [2]. |
| CIViCmine Database | Text-mined knowledgebase of clinical evidence for cancer biomarkers. | Provides curated data for training and validating ML models in oncology [27]. |
| DisProt / IUPred / AlphaFold | Databases and tools for analyzing intrinsic protein disorder, a feature for predictive biomarkers. | Used as features in ML models like MarkerPredict to identify cancer biomarkers [27]. |
| Cloud Data Environments | Secure, scalable platforms for collaborative analysis of large, harmonized datasets. | Alzheimer's Disease Data Initiative's AD Workbench used by GNPC to manage data access and analysis [31]. |
The field of biomarker discovery is undergoing a fundamental transformation, shifting from traditional single-analyte approaches toward integrative, data-intensive strategies powered by machine learning (ML). This evolution is critical for addressing the biological complexity underlying disease mechanisms, particularly for heterogeneous conditions like cancer, neurological disorders, and metabolic diseases. Where conventional methods often identified correlative biomarkers with limited clinical utility, modern ML approaches now enable researchers to uncover functional biomarkers—molecules and molecular signatures with direct roles in pathological processes—thus bridging the gap between correlation and causation.
The limitations of traditional biomarker discovery are becoming increasingly apparent. Methods focusing on single molecular features face significant challenges with reproducibility, high false-positive rates, and inadequate predictive accuracy due to the inherent biological heterogeneity of complex diseases [11]. These approaches often fail to capture the multifaceted biological networks underpinning disease mechanisms. In contrast, machine learning and deep learning methodologies represent a substantial shift by handling vast and complex biological datasets, known collectively as multi-omics data, which integrate genomics, transcriptomics, proteomics, metabolomics, imaging, and clinical records [11]. This comprehensive profiling facilitates the identification of highly predictive biomarkers and provides unprecedented insights into functional disease mechanisms.
The application of these advanced computational techniques has expanded beyond conventional diagnostic and prognostic biomarkers to include functional biomarkers like biosynthetic gene clusters (BGCs)—groups of genes encoding enzymatic machinery for producing specialized metabolites with therapeutic potential [11]. This represents a novel dimension in biomarker discovery, directly linking genomic capabilities to functional outcomes. This article explores the transformative role of machine learning in uncovering functional biomarkers, detailing experimental protocols, analytical frameworks, and their applications in precision medicine.
Machine Learning Approaches for Functional Biomarker Discovery
Methodological Frameworks and Algorithms
Machine learning applications in biomarker discovery encompass diverse methodologies tailored to different data structures and biological questions. Supervised learning approaches train predictive models on labeled datasets to classify disease status or predict clinical outcomes. Commonly used techniques include Support Vector Machines (SVM), which identify optimal hyperplanes for separating classes in high-dimensional omics data; Random Forests, ensemble models that aggregate multiple decision trees for robustness against noise; and gradient boosting algorithms (e.g., XGBoost, LightGBM), which iteratively correct previous prediction errors for superior accuracy [11]. For feature selection, Least Absolute Shrinkage and Selection Operator (LASSO) regression effectively identifies the most relevant molecular features from high-dimensional datasets [32].
In contrast, unsupervised learning explores unlabeled datasets to discover inherent structures or novel subgroupings without predefined outcomes. These methods are invaluable for endotyping—classifying diseases based on underlying biological mechanisms rather than purely clinical symptoms [11]. Techniques include clustering methods (k-means, hierarchical clustering) and dimensionality reduction approaches (principal component analysis).
Deep learning architectures represent a more advanced frontier, with convolutional neural networks (CNNs) excelling at spatial pattern recognition in imaging and histopathology data, and recurrent neural networks (RNNs) capturing temporal dynamics in longitudinal biomedical data [11] [32]. The emerging integration of large language models and transformers further enhances the ability to extract insights from complex clinical narratives and molecular sequences [11].
Table 1: Machine Learning Algorithms for Different Data Types in Biomarker Discovery
| Omics Data Type | ML Techniques | Typical Applications |
|---|---|---|
| Transcriptomics | Feature selection (e.g., LASSO); SVM; Random Forests | Identifying differential gene expression signatures; Disease classification |
| Proteomics | CNN; LASSO; SVM-RFE | Pattern recognition in protein arrays; Biomarker signature identification |
| Metagenomics | Random Forests; CNN; Feature selection | Identifying microbial signatures; Predicting functional traits like BGCs |
| Imaging Data | Convolutional Neural Networks (CNN); Deep Learning | Extracting prognostic features from histopathology; Quantitative imaging biomarkers |
| Multi-omics Integration | Multi-layer perceptrons; Ensemble methods; Stacked generalization | Developing comprehensive biomarker panels; Disease endotyping |
Workflow for Identifying Functional Biomarkers
The discovery of functional biomarkers follows a structured computational and experimental workflow. The process begins with data acquisition and preprocessing from diverse sources, including public repositories like the Gene Expression Omnibus (GEO) and in-house experimental data. For transcriptomic analyses, the "limma" R package is commonly employed to identify differentially expressed genes (DEGs) using criteria such as |logFold Change (logFC)| > 0.585 and adjusted p-value < 0.05 [32].
Following differential expression analysis, Weighted Gene Co-expression Network Analysis (WGCNA) identifies gene modules associated with specific traits or diseases by constructing a biologically meaningful network through selection of an appropriate soft-threshold power (β) [33] [32]. This approach transforms adjacency matrices into topological overlap matrices (TOM) and identifies gene modules using hierarchical clustering and dynamic tree cutting. Key modules are selected based on correlations between module eigengenes and clinical traits.
Integration of multiple machine learning algorithms significantly enhances the robustness of biomarker identification. Studies often employ 101 unique combinations of 10 machine learning algorithms to identify the most significant interacting genes between related conditions [33]. For instance, the glmBoost+RF combination has demonstrated superior performance in identifying biomarkers linking diabetes and kidney stones [33]. Similarly, integration of LASSO, Random Forest, Boruta, and SVM-RFE has proven effective in heart failure biomarker discovery [32].
Functional validation of computational predictions involves protein-protein interaction (PPI) network construction using databases like STRING (with a composite score > 0.4 considered significant) and functional enrichment analysis using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses via the "clusterProfiler" R package [32]. These analyses elucidate biological processes, molecular functions, and signaling pathways associated with candidate biomarkers.
Diagram 1: Computational Workflow for Functional Biomarker Discovery. The process integrates multiple data analysis steps from acquisition to experimental validation.
Application Notes: Case Studies in Functional Biomarker Discovery
Case Study 1: Bridging Diabetes and Nephrolithiasis Through Programmed Cell Death Pathways
Our first case study demonstrates the power of integrative bioinformatics and machine learning to uncover shared mechanisms between metabolic and urinary system disorders. Research has revealed an increased prevalence of kidney stones among diabetic patients, suggesting potential underlying mechanistic links [33]. To investigate these connections, researchers conducted bulk transcriptome differential analysis using sequencing data combined with the AS dataset (GSE231569) after eliminating batch effects [33].
The investigation focused on programmed cell death (PCD) pathways—including apoptosis, autophagy, pyroptosis, ferroptosis, and necroptosis—given their established roles in both diabetic complications and kidney stone formation. Differential expression analysis of PCD-related genes was conducted using the limma R package with criteria of adjusted P.Val < 0.05 and |logFC| > 0.25 [33]. This was complemented by WGCNA to identify gene modules associated with both conditions.
Through the application of 10 machine learning algorithms generating 101 unique combinations, three key biomarkers emerged as the most significant interacting genes: S100A4, ARPC1B, and CEBPD [33]. These genes were validated in both training and test datasets, demonstrating strong diagnostic potential. Western blot analysis confirmed protein-level expression changes, providing orthogonal validation of the computational findings.
The functional significance of these biomarkers was further elucidated through enrichment analyses, which revealed their involvement in immune regulation and inflammatory processes—key mechanisms linking diabetes and nephrolithiasis. This case exemplifies how machine learning can unravel complex relationships between seemingly distinct conditions, revealing shared pathological mechanisms and potential therapeutic targets.
Case Study 2: Deep Learning for Heart Failure Biomarkers and Therapeutic Targets
Our second case study explores a comprehensive approach to heart failure biomarker discovery, culminating in the development of a deep learning diagnostic model. The study utilized gene expression data from GEO datasets (GSE17800, GSE57338, and GSE29819), applying the ComBat algorithm to remove batch effects before analysis [32].
The research employed four machine learning methods—LASSO, Random Forest, Boruta, and SVM-RFE—to identify potential genes linked to heart failure [32]. This multi-algorithm approach identified four essential genes: ITIH5, ISLR, ASPN, and FNDC1. The study then developed a novel diagnostic model using a deep learning convolutional neural network (CNN), which demonstrated strong performance in validation against public datasets [32].
Single-cell RNA sequencing analysis of dataset GSE145154 provided unprecedented resolution, revealing stable up-regulation patterns of these genes across various cardiomyocyte types in HF patients [32]. This single-cell validation at the cellular level strengthened the case for the functional relevance of these biomarkers.
Beyond biomarker discovery, the study explored drug-protein interactions, revealing two potential therapeutic drugs targeting the identified key genes [32]. Molecular docking simulations provided feasible pathways for these interactions, demonstrating how functional biomarker discovery can directly inform therapeutic development. This end-to-end pipeline—from computational biomarker identification to therapeutic candidate prediction—showcases the transformative potential of machine learning in cardiovascular precision medicine.
Table 2: Key Biomarkers Identified Through ML Approaches in Recent Studies
| Disease Context | Identified Biomarkers | ML Methods Used | Functional Significance |
|---|---|---|---|
| Diabetes & Nephrolithiasis | S100A4, ARPC1B, CEBPD | 10 algorithms with 101 combinations; glmBoost+RF | Role in programmed cell death pathways linking metabolic and urinary diseases |
| Heart Failure | ITIH5, ISLR, ASPN, FNDC1 | LASSO, Random Forest, Boruta, SVM-RFE | Extracellular matrix organization; cardiac remodeling |
| Psychiatric Disorders | Resting-state Functional Connectivity patterns | Ensemble sparse classifiers | Altered brain network connectivity in MDD, SCZ, and ASD |
Experimental Protocols
Protocol 1: Transcriptomic Biomarker Discovery with Integrated Machine Learning
Sample Preparation and Data Acquisition
- Tissue Collection: Obtain tissue samples (e.g., renal papilla, cardiac tissue) from both disease models and controls. For animal studies, ensure compliance with institutional animal care guidelines (e.g., NIH guidelines) [33].
- RNA Extraction: Use TRIzol reagent for total RNA extraction. Quantity RNA using NanoDrop 2000, ensuring 260/280 ratios between 1.8-2.0 [33].
- Library Preparation and Sequencing: Perform reverse transcription using kits such as ToloScript All-in-one RT EasyMix. Conduct RNA sequencing using appropriate platforms (e.g., Illumina) with minimum depth of 30 million reads per sample [33].
- Public Data Sourcing: Download complementary datasets from GEO database (e.g., GSE231569, GSE73680) for validation cohorts [33].
Computational Analysis
- Data Preprocessing: Normalize data using preprocessCore R package. Remove batch effects using ComBat algorithm when integrating multiple datasets [32].
- Differential Expression Analysis: Use limma R package with cutoff criteria of adjusted P.Val < 0.05 and |logFC| > 0.25-0.585 [33] [32]. Generate volcano plots and heatmaps using "pheatmap" package.
- Weighted Gene Co-expression Network Analysis (WGCNA):
- Select top 50% of genes with greatest variance for network construction.
- Determine soft-threshold power (β) based on scale-free topology criterion.
- Construct topological overlap matrix (TOM) and identify gene modules using dynamic tree cutting.
- Calculate gene significance (GS) and module membership (MM) for trait associations [33] [32].
- Machine Learning Integration: Apply multiple ML algorithms (LASSO, Random Forest, SVM-RFE, Boruta) with 10-fold cross-validation. Intersect results from different methods to identify robust biomarker candidates [32].
Functional Validation
- Protein-Protein Interaction Networks: Construct PPI networks using STRING database (confidence score > 0.4) and visualize with Cytoscape [33] [32].
- Functional Enrichment: Perform GO and KEGG pathway analyses using "clusterProfiler" R package. Set statistical significance threshold at p < 0.05 [33] [32].
- Transcription Factor Network Analysis: Predict upstream regulators using RegNetwork database and construct TF-gene interaction networks [33].
Protocol 2: Spatial Biomarker Validation Using Advanced Imaging Technologies
Sample Preparation and Multiplex Imaging
- Tissue Sectioning: Prepare fresh-frozen or FFPE tissue sections at 4-5μm thickness using a cryostat or microtome.
- Multiplex Immunohistochemistry/Optical Coherence Tomography:
- Perform antigen retrieval using appropriate buffers (e.g., citrate buffer for FFPE tissues).
- Implement sequential staining with antibody panels including 10-40 markers.
- Use tyramide signal amplification (TSA) for signal enhancement with careful antibody stripping between rounds.
- For OCT, capture cross-sectional retinal images with micron-level resolution [34].
Image Analysis and Biomarker Quantification
- Image Preprocessing: Apply flat-field correction, background subtraction, and compensation for spectral overlap.
- Cell Segmentation: Use machine learning-based segmentation (e.g., CellProfiler, Ilastik) to identify individual cells and subcellular compartments.
- Spatial Analysis: Quantify biomarker expression patterns relative to tissue structures and cellular neighborhoods. Calculate cell-to-cell distances and interaction frequencies [2].
- Biomarker Validation: Correlate spatial expression patterns with clinical outcomes using appropriate statistical models.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Research Reagent Solutions for Functional Biomarker Discovery
| Reagent/Platform | Function | Application Context |
|---|---|---|
| TRIzol Reagent | RNA isolation from tissues and cells | Preserves RNA integrity for transcriptomic studies [33] |
| RIPA Lysis Buffer | Protein extraction from tissues | Western blot validation of candidate biomarkers [33] |
| Primary Antibodies | Target protein detection | Validation of ARPC1B, S100A4, CEBPD and other biomarkers [33] |
| Seurat R Package | Single-cell RNA sequencing analysis | Cell type identification and differential expression [33] |
| STRING Database | Protein-protein interaction network analysis | Understanding functional relationships between biomarker candidates [33] [32] |
| Omni LH 96 Homogenizer | Automated sample homogenization | Standardized sample preparation for multi-omics studies [7] |
| Optical Coherence Tomography | Non-invasive retinal imaging | Measuring RNFL and GCIPL thickness as structural biomarkers [34] |
Discussion and Future Perspectives
The integration of machine learning with multi-omics data represents a paradigm shift in biomarker discovery, enabling the transition from correlative to functional biomarkers. However, several challenges remain in the clinical implementation of these approaches. Data quality issues, including limited sample sizes, noise, batch effects, and biological heterogeneity, can severely impact model performance, leading to overfitting and reduced generalizability [11]. The interpretability of ML models remains a significant hurdle, as many advanced algorithms function as "black boxes," making it difficult to elucidate specific prediction mechanisms [11].
Future advancements will likely focus on several key areas. First, the development of explainable AI (XAI) methods will be crucial for clinical adoption, where transparency and trust in predictive models are essential [11]. Second, rigorous external validation using independent cohorts and experimental methods must become standard practice to ensure reproducibility and clinical reliability [11]. Third, the integration of temporal dynamics through longitudinal data collection and analysis will enhance our understanding of disease progression and biomarker evolution.
The ethical and regulatory considerations surrounding ML-derived biomarkers also warrant careful attention. Biomarkers used for patient stratification, therapeutic decision-making, or disease prognosis must comply with rigorous standards set by regulatory bodies such as the FDA [11]. The dynamic nature of ML-driven biomarker discovery, where models continuously evolve with new data, presents particular challenges for regulatory oversight and demands adaptive yet strict validation frameworks.
Emerging technologies like spatial biology and liquid biopsy are further expanding the frontiers of biomarker discovery [2] [7]. Spatial techniques enable researchers to understand biomarker organization within tissue architecture, providing critical context for functional interpretation [2]. Liquid biopsy approaches offer non-invasive methods for biomarker detection and monitoring, potentially revolutionizing patient follow-up and treatment response assessment [7].
As these technologies mature and computational methods advance, functional biomarker discovery will increasingly enable disease endotyping—classifying subtypes based on shared molecular mechanisms rather than solely clinical symptoms [11]. This mechanistic approach supports more precise patient stratification, therapy selection, and understanding of disease heterogeneity, ultimately fulfilling the promise of precision medicine across diverse therapeutic areas.
Diagram 2: Evolution from Correlative to Functional Biomarkers. The field is transitioning through integration of multi-omics data and machine learning toward functionally validated biomarkers with direct therapeutic relevance.
A Practical Guide to ML Algorithms and Their Biomedical Applications
The advent of high-throughput technologies has enabled the comprehensive profiling of biological systems across multiple molecular layers, generating vast amounts of high-dimensional omics data. A fundamental challenge in analyzing these data is the "curse of dimensionality," where the number of features (e.g., genes, proteins, metabolites) vastly exceeds the number of samples, creating a high-dimensional, low-sample-size (HDLSS) scenario [35] [36]. This imbalance poses significant risks of overfitting and poor model generalization, ultimately compromising the reliability of identified biomarkers and biological insights. Feature selection techniques have thus become indispensable tools for navigating this complexity, serving to identify the most informative molecular features while discarding irrelevant or redundant variables [37].
The challenges are particularly pronounced in multi-omics studies, where datasets integrate various molecular layers such as genomics, transcriptomics, proteomics, and metabolomics. These data types exhibit heterogeneous structures, varying scales, and different noise characteristics, creating unique analytical hurdles [38] [39]. Furthermore, omics datasets frequently suffer from class imbalance, where certain biological or clinical outcomes are underrepresented, potentially biasing predictive models [40]. Effective feature selection must therefore not only reduce dimensionality but also account for the complementary information embedded across omics modalities while maintaining biological relevance.
Feature Selection Methodologies and Comparative Performance
Categories of Feature Selection Approaches
Feature selection methods can be broadly categorized into three main types based on their integration with the modeling process. Filter methods evaluate the relevance of features based on statistical properties independent of any machine learning algorithm. Common examples include minimum Redundancy Maximum Relevance (mRMR), which selects features that have high mutual information with the target class but low mutual information with other features [37]. Embedded methods incorporate feature selection as part of the model training process; typical examples include Least Absolute Shrinkage and Selection Operator (Lasso), which performs regularization and variable selection simultaneously, and permutation importance from Random Forests (RF-VI) [37]. Wrapper methods use the performance of a predictive model to evaluate feature subsets, such as Recursive Feature Elimination (RFE) and Genetic Algorithms (GA), though these approaches tend to be computationally intensive [37].
Recent advancements have introduced ensemble and hybrid approaches that combine multiple selection strategies to enhance robustness. For instance, MCC-REFS employs an ensemble of eight machine learning classifiers and uses the Matthews Correlation Coefficient as a selection criterion, which is particularly effective for imbalanced datasets [40]. Similarly, Deep Learning-based feature selection methods, such as those incorporating transformer architectures, have shown promise in capturing complex, non-linear relationships in multi-omics data [41].
Benchmarking Studies and Performance Insights
Large-scale benchmarking studies provide critical insights into the relative performance of feature selection methods in omics contexts. A comprehensive evaluation using 15 cancer multi-omics datasets from The Cancer Genome Atlas revealed that mRMR, Random Forest permutation importance (RF-VI), and Lasso consistently outperformed other methods in predicting binary outcomes [37]. Notably, mRMR and RF-VI achieved strong predictive performance even with small feature subsets (e.g., 10-100 features), while other methods required larger feature sets to comparable performance [37].
Table 1: Performance Comparison of Feature Selection Methods on Multi-omics Data
| Method | Type | Key Strengths | Performance Notes | Computational Cost |
|---|---|---|---|---|
| mRMR | Filter | Selects non-redundant, informative features | High performance with small feature sets; best overall in multiple benchmarks | Moderate |
| RF-VI | Embedded | Robust to noise and non-linear relationships | Strong performance with few features; handles complex interactions | Low to Moderate |
| Lasso | Embedded | Simultaneous feature selection and regularization | Requires more features than mRMR/RF-VI; excellent predictive accuracy | Low |
| SVM-RFE | Wrapper | Model-guided feature elimination | Performance varies with classifier; can be effective with SVM | High |
| ReliefF | Filter | Sensitive to feature interactions | Lower performance with small feature sets | Moderate |
| Genetic Algorithm | Wrapper | Comprehensive search of feature space | Often selects too many features; computationally intensive | Very High |
The integration strategy—whether features are selected separately per omics type or concurrently across all omics—showed minimal impact on predictive performance for most methods. However, concurrent selection generally required more computation time [37]. This suggests that the choice between separate and concurrent integration may depend more on practical considerations than on performance gains for standard predictive tasks.
Practical Implementation Protocols
Automated Machine Learning Pipeline for Biomarker Discovery
The BioDiscML platform exemplifies an integrated approach to biomarker discovery, implementing a comprehensive pipeline that automates key machine learning steps [35]. The protocol begins with data preprocessing, where input datasets are merged (if multiple sources are provided) and split into training and test sets (typically 2/3 for training, 1/3 for testing). A feature ranking algorithm then sorts all features based on their predictive power, retaining only the top-ranked features (default: 1,000) to reduce dimensionality [35].
The core feature selection process employs two main strategies: top-k feature selection, which simply selects the best k elements from the ordered feature set, and stepwise selection, where features are sequentially added or removed based on performance improvement. For each candidate feature subset, the pipeline trains a model and evaluates performance using 10-fold cross-validation. This process is repeated across multiple machine learning algorithms, ultimately generating thousands of potential models [35]. The final output includes optimized feature signatures with associated performance metrics, providing researchers with actionable biomarker candidates.
Multi-omics Integration Framework for Survival Analysis
For complex endpoints such as survival outcomes, advanced integration frameworks are required. One such approach for breast cancer survival analysis employs genetic programming to adaptively select and integrate features across omics modalities [39]. The protocol begins with data preprocessing to handle missing values, normalize distributions, and align samples across omics platforms. The core integration phase uses genetic programming to evolve optimal combinations of molecular features, evaluating each candidate feature set based on its ability to predict survival outcomes using the concordance index (C-index) as the fitness metric [39].
The final model development phase constructs a survival model using the selected multi-omics features, typically employing Cox proportional hazards models or random survival forests. This approach has demonstrated robust performance in breast cancer survival prediction, achieving a C-index of 78.31 during cross-validation and 67.94 on independent test sets [39]. The adaptive nature of genetic programming allows the framework to identify complex, non-linear relationships between different molecular layers and clinical outcomes, often revealing biologically insightful interactions that might be missed by conventional methods.
Transformer-Based Deep Learning for Multi-omics Feature Selection
Recent advances in deep learning have introduced transformer-based architectures for multi-omics feature selection. In a study focused on hepatocellular carcinoma (HCC), researchers developed a novel approach combining recursive feature selection with transformer models as estimators [41]. The protocol begins with data preparation from multiple mass spectrometry-based platforms, including metabolomics, lipidomics, and proteomics. Following data normalization and batch effect correction, the transformer model is trained to classify samples (e.g., HCC vs. cirrhosis) while simultaneously learning feature importance [41].
The key innovation lies in using the self-attention mechanisms of transformers to weight the importance of different molecular features across omics layers. Features are then recursively eliminated based on their attention scores, with the process repeating until an optimal feature subset is identified. This approach has demonstrated superior performance compared to sequential deep learning methods, particularly for integrating multi-omics data with limited sample sizes [41]. The selected features can subsequently be validated through pathway analysis tools to establish biological relevance and potential mechanistic insights.
Table 2: Research Reagent Solutions for Multi-omics Feature Selection
| Reagent/Resource | Function | Application Context |
|---|---|---|
| BioDiscML | Automated biomarker discovery platform | General omics biomarker discovery [35] |
| MCC-REFS | Ensemble feature selection with MCC criterion | Imbalanced class datasets [40] |
| SMOPCA | Spatial multi-omics dimension reduction | Spatial domain detection in tissue samples [42] |
| MOFA+ | Bayesian group factor analysis | Multi-omics data integration [39] |
| Transformer-SVM | Deep learning feature selection | HCC biomarker discovery [41] |
| Genetic Programming Framework | Adaptive multi-omics integration | Survival analysis in breast cancer [39] |
Advanced Integration Strategies and Emerging Directions
Spatial Multi-omics Integration
The emergence of spatial transcriptomics and proteomics technologies has created new challenges and opportunities for feature selection. Traditional methods often fail to account for spatial dependencies between cellular measurements, potentially discarding biologically meaningful patterns. SMOPCA (Spatial Multi-Omics Principal Component Analysis) addresses this limitation by performing joint dimension reduction while explicitly preserving spatial relationships [42]. The method incorporates spatial location information through multivariate normal priors on latent factors, enabling the learned representations to maintain neighborhood similarity while integrating information across omics modalities [42].
The SMOPCA workflow begins with spatial coordinate processing, where spatial relationships between measurement locations (e.g., tissue spots) are encoded into covariance matrices. These spatial constraints are then integrated with multi-omics measurements (e.g., transcriptomics, proteomics) through a factor analysis model that learns joint latent representations reflecting both molecular profiles and spatial organization [42]. The resulting embeddings significantly improve spatial domain detection accuracy compared to non-spatial methods, enabling more precise identification of tissue regions with distinct molecular signatures.
Dimensionality Reduction-Guided Feature Selection
Another promising approach leverages intrinsic dimension analysis to guide the feature selection process. Rather than applying uniform dimensionality reduction across all omics types, this method first estimates the intrinsic dimensionality of each omics dataset separately, assessing the curse-of-dimensionality impact on each view [43]. For views significantly affected by high dimensionality, a two-step reduction strategy is applied, combining feature selection with feature extraction in a tailored manner [43].
This adaptive approach recognizes that different omics data types possess varying levels of intrinsic redundancy and noise. By customizing the reduction strategy for each data type based on its specific characteristics, the method achieves more biologically meaningful feature subsets compared to one-size-fits-all reduction pipelines [43]. The protocol involves first estimating intrinsic dimensionality using techniques such as nearest neighbor distances or eigenvalue analysis, then applying appropriate reduction techniques (filter methods, embedded methods, or matrix factorization) based on the estimated complexity of each omics layer.
Feature selection remains a critical component in the analysis of high-dimensional omics data, enabling robust biomarker discovery and enhancing biological interpretation. The current landscape offers a diverse arsenal of methods, from statistically principled filter approaches to sophisticated deep learning architectures, each with distinct strengths and optimal application contexts. As omics technologies continue to evolve, generating increasingly complex and multimodal datasets, feature selection methodologies must correspondingly advance to address new challenges.
Future directions in the field point toward adaptive integration frameworks that automatically tailor selection strategies to data characteristics, spatially aware methods that incorporate topological relationships, and foundation models pre-trained on large-scale omics corpora that can be fine-tuned for specific biomarker discovery tasks [38] [39]. The integration of prior biological knowledge through pathway databases and molecular networks represents another promising avenue for constraining feature selection and enhancing biological plausibility. As these methodologies mature, they will increasingly empower researchers to distill meaningful biological signals from high-dimensional omics data, ultimately accelerating discoveries in basic biology and translational medicine.
The advent of high-throughput technologies in genomics and proteomics has generated vast, complex biological datasets, creating an pressing need for advanced analytical tools in biomarker discovery. Supervised machine learning (ML) algorithms have emerged as powerful tools for identifying robust, clinically relevant biomarkers from these multi-omics datasets. Among the diverse ML landscape, Support Vector Machines (SVM), Random Forest (RF), and eXtreme Gradient Boosting (XGBoost) have demonstrated particular utility in handling the high-dimensionality, noise, and complex interactions inherent to biological data [9]. These algorithms can integrate diverse data streams to identify diagnostic, prognostic, and predictive biomarkers, thereby accelerating the development of personalized treatment strategies in oncology, neurological disorders, and other disease areas [9].
This article provides a structured comparison of SVM, Random Forest, and XGBoost within the context of biomarker discovery research. We present quantitative performance comparisons, detailed experimental protocols for implementing these algorithms in biomarker identification pipelines, and visualizations of key workflows. The guidance aims to equip researchers and drug development professionals with practical knowledge for selecting, implementing, and interpreting these machine learning techniques in their translational research.
Theoretical Foundations and Comparative Mechanics
Understanding the fundamental operational principles of each algorithm is crucial for their appropriate application in biomarker discovery.
Support Vector Machines (SVM) operate on the principle of identifying an optimal hyperplane that maximizes the margin between different classes in a high-dimensional feature space. For non-linearly separable data, SVM utilizes kernel functions to transform the input space, allowing for effective separation. This characteristic makes SVM particularly effective for datasets where the relationship between features and outcomes is complex but not necessarily hierarchical.
Random Forest is an ensemble learning method that constructs a multitude of decision trees during training and outputs the mode of their classes (classification) or mean prediction (regression) [44]. The algorithm introduces randomness through bagging (bootstrap aggregating) and random feature selection when splitting nodes, which enhances diversity among the trees and reduces overfitting compared to single decision trees. This makes RF robust to noise and capable of handling high-dimensional data with mixed data types, which are common in genomics and proteomics [44].
XGBoost (eXtreme Gradient Boosting) is an advanced implementation of gradient boosted decision trees designed for speed and performance [44]. Unlike Random Forest, which builds trees independently, XGBoost builds trees sequentially, with each new tree correcting errors made by the previous ones. It minimizes a regularized (L1 and L2) objective function, which helps control model complexity and reduces overfitting [45]. XGBoost's efficiency with large datasets, handling of missing values, and ability to capture complex nonlinear relationships and feature interactions have made it particularly popular in recent biomarker discovery research [46] [9].
Performance Comparison in Biomedical Applications
Quantitative Performance Metrics
Multiple studies across different biomedical domains have evaluated the comparative performance of SVM, Random Forest, and XGBoost. Their performance varies depending on the data characteristics, application domain, and implementation specifics.
Table 1: Comparative Performance Metrics Across Domains
| Application Domain | Algorithm | Reported Performance | Reference |
|---|---|---|---|
| Facies Classification | CatBoost | 95.4% CV Accuracy | [47] |
| Facies Classification | XGBoost | 93.7% CV Accuracy | [47] |
| Facies Classification | Random Forest | 89.5% Test Accuracy | [47] |
| Facies Classification | SVM | 85.6% Test Accuracy | [47] |
| Predictive Biomarker Classification (MarkerPredict) | XGBoost | 0.7-0.96 LOOCV Accuracy | [27] |
| Predictive Biomarker Classification (MarkerPredict) | Random Forest | Marginal underperformance vs. XGBoost | [27] |
| Cancer Classification (XGB-BIF) | XGBoost | >90% Accuracy, Kappa: 0.80-0.99 | [46] |
Qualitative Comparative Analysis
Each algorithm presents distinct strengths and limitations for biomarker discovery:
Support Vector Machines
- Strengths: Effective in high-dimensional spaces, memory efficient due to use of support vectors, versatile through kernel functions [44].
- Limitations: Less effective with noisy data or overlapping classes, probability estimates not native, computational cost increases with dataset size [44].
Random Forest
- Strengths: High accuracy for many scenarios, resistance to overfitting, robust to outliers and missing data, provides native feature importance metrics [44].
- Limitations: "Black box" nature complicates interpretability, computationally intensive with large datasets, not suitable for extrapolation beyond training data range [44].
XGBoost
- Strengths: High predictive performance, built-in regularization prevents overfitting, handles missing values natively, efficient with large datasets, provides feature importance scores [46] [45].
- Limitations: Parameter tuning can be complex, potential overfitting without proper regularization, less interpretable than simpler models [45].
Experimental Protocols for Biomarker Discovery
General Workflow for Biomarker Discovery
The following diagram illustrates the end-to-end workflow for biomarker discovery using supervised machine learning:
Protocol 1: Biomarker Discovery Using Random Forest
Objective: Identify predictive biomarkers from genomic or proteomic data using Random Forest.
Materials and Reagents:
- Genomic or proteomic dataset with clinical annotations
- Computing environment with Python/R and necessary libraries
Procedure:
- Data Preparation:
- Compile multi-omics data (e.g., gene expression, protein levels) with clinical outcomes
- Perform missing value imputation using appropriate methods (e.g., k-nearest neighbors)
- Split data into training (70-80%) and hold-out test sets (20-30%)
Feature Selection:
- Apply variance-based filtering to remove low-variance features
- Conduct preliminary Random Forest run to assess initial feature importance
- Select top-k features based on mean decrease in Gini impurity
Model Training:
- Implement Random Forest using scikit-learn or XGBoost's RF implementation
- Set critical parameters: nestimators=100-500, maxfeatures='sqrt', max_depth=5-15
- Enable out-of-bag (OOB) scoring for internal validation
Model Validation:
- Perform k-fold cross-validation (k=5-10) to assess stability
- Evaluate on hold-out test set using accuracy, AUC-ROC, precision, recall
- Compute permutation importance to confirm biomarker significance
Biomarker Interpretation:
- Generate feature importance plots using mean decrease in accuracy
- Conduct functional enrichment analysis (GO, KEGG) on top biomarkers
- Validate identified biomarkers in external datasets if available
Troubleshooting Tips:
- If model performance is poor, increase n_estimators progressively
- For overfitting, reduce maxdepth or increase minsamples_split
- For computational constraints, use subsampling or feature reduction
Protocol 2: Predictive Biomarker Identification with XGBoost
Objective: Implement XGBoost for high-accuracy predictive biomarker discovery, following approaches like the MarkerPredict framework [27].
Materials and Reagents:
- Curated positive and negative biomarker training sets (e.g., from CIViCmine database)
- Network topological data (e.g., signaling pathways from Reactome, SIGNOR)
- Protein disorder information (e.g., from DisProt, IUPred)
Procedure:
- Training Set Construction:
- Compile known predictive biomarker-target pairs from literature and databases
- Create negative controls from proteins not annotated as biomarkers
- Integrate network topological features and protein disorder metrics
Model Configuration:
- Implement XGBoost with tree booster
- Set key parameters: learningrate=0.1, maxdepth=6, n_estimators=100, subsample=0.8
- Enable regularization: reglambda=1, regalpha=0.1, gamma=0
- For Random Forest mode in XGBoost: set numparalleltree=100, subsample=0.8, colsamplebynode=0.8, learningrate=1 [48]
Model Training and Validation:
- Employ Leave-One-Out-Cross-Validation (LOOCV) or repeated k-fold CV
- Compute Biomarker Probability Score (BPS) as normalized summative rank across models [27]
- Validate on external datasets when available
Biomarker Prioritization:
- Rank candidate biomarkers by BPS or probability scores
- Apply SHAP (SHapley Additive exPlanations) for interpretable feature importance
- Conduct survival analysis (Cox regression, Kaplan-Meier) for clinical relevance
Troubleshooting Tips:
- For class imbalance, adjust scaleposweight parameter
- If overfitting occurs, increase regularization parameters or reduce model complexity
- For large datasets, utilize GPU acceleration (treemethod='gpuhist')
Protocol 3: SVM for Biomarker Classification
Objective: Utilize SVM for biomarker classification tasks, particularly with high-dimensional omics data.
Procedure:
- Data Preprocessing:
- Apply standardization (z-score normalization) to all features
- Address class imbalance through SMOTE or weighted classes
Kernel Selection:
- Test linear kernel for high-dimensional data
- Consider RBF kernel for non-linear relationships
- Use polynomial kernel for specific domain knowledge
Model Training:
- Implement SVM with chosen kernel
- Optimize C parameter (regularization) and kernel-specific parameters
- Use cross-validation for parameter tuning
Model Evaluation:
- Assess performance using standard classification metrics
- Generate ROC curves and precision-recall plots
- Compare against baseline models
Table 2: Key Resources for Machine Learning in Biomarker Discovery
| Resource Category | Specific Tools/Databases | Function in Biomarker Discovery |
|---|---|---|
| Biomarker Databases | CIViCmine, DisProt | Provide annotated biomarker data for training and validation [27] |
| Protein Databases | DisProt, AlphaFold, IUPred | Offer protein disorder and structural features [27] |
| Signaling Networks | ReactomeFI, SIGNOR, Human Cancer Signaling Network | Supply network topological features [27] |
| Machine Learning Frameworks | Scikit-learn, XGBoost, SHAP, LIME | Enable model implementation and interpretation [46] [44] |
| Validation Tools | Cross-validation, External Datasets, Survival Analysis | Assess clinical relevance and model generalizability [46] |
Algorithm Configuration Guidelines
Parameter Optimization Strategies
Random Forest Critical Parameters:
- n_estimators: Number of trees (100-500 typically sufficient)
- max_features: Features considered for split ('sqrt' or 'log2' for high-dimensional data)
- max_depth: Tree depth control to prevent overfitting
- minsamplessplit: Minimum samples required to split a node
- minsamplesleaf: Minimum samples required at a leaf node
XGBoost Critical Parameters:
- learning_rate: Step size shrinkage (0.01-0.3)
- max_depth: Maximum tree depth (3-10)
- subsample: Instance subsampling ratio (0.5-0.8)
- colsample_bytree: Feature subsampling ratio (0.5-0.8)
- reg_alpha: L1 regularization (0-1)
- reg_lambda: L2 regularization (0.1-1)
- gamma: Minimum loss reduction for split (0-0.5)
SVM Critical Parameters:
- C: Regularization parameter (0.1-100)
- kernel: Kernel type (linear, rbf, poly)
- gamma: Kernel coefficient for rbf/poly ('scale' or 'auto')
Implementation Considerations for Biomarker Data
The following diagram illustrates the decision process for selecting the appropriate algorithm based on biomarker discovery project characteristics:
Validation and Interpretation Frameworks
Robust Validation Strategies
Rigorous validation is essential for translational biomarker research. Recommended approaches include:
- Nested Cross-Validation: Use inner loops for parameter optimization and outer loops for performance estimation to prevent optimistic bias
- External Validation: Test models on completely independent datasets from different sources or populations
- Clinical Validation: Assess biomarker utility through survival analysis, treatment response prediction, or correlation with clinical outcomes
- Biological Validation: Conduct functional enrichment analysis and pathway mapping to establish biological plausibility
Interpretation Techniques
Model interpretability is crucial for biomarker discovery:
- Feature Importance: Use native importance metrics (Gini for RF, Gain for XGBoost) complemented by permutation importance
- SHAP Analysis: Employ SHapley Additive exPlanations for consistent, theoretically grounded feature attribution [46]
- LIME: Utilize Local Interpretable Model-agnostic Explanations for instance-level explanations [44]
- Partial Dependence Plots: Visualize relationship between feature values and predicted outcomes
SVM, Random Forest, and XGBoost each offer distinct advantages for biomarker discovery applications. Random Forest provides robust performance and native interpretability, making it suitable for initial exploration. XGBoost typically delivers superior predictive accuracy, particularly with large, complex datasets, at the cost of increased computational requirements and parameter sensitivity. SVM performs well with high-dimensional data and clear separation margins. The selection among these algorithms should be guided by project-specific considerations including dataset characteristics, interpretability requirements, and computational resources. As biomarker discovery continues to evolve, the integration of these machine learning approaches with multi-omics data and clinical validation will be essential for advancing precision medicine.
The discovery of robust biomarkers is critical for precision medicine, supporting disease diagnosis, prognosis, and personalized treatment decisions [11]. Traditional biomarker discovery methods, which often focus on single molecular features, face significant challenges including limited reproducibility, high false-positive rates, and an inability to capture the complex, multifaceted biological networks that underpin disease mechanisms [11]. Deep learning, a subset of machine learning employing artificial neural networks, addresses these limitations by analyzing large, complex datasets to identify patterns and interactions previously unrecognized by conventional approaches [11] [49].
This application note focuses on two pivotal deep learning architectures: Convolutional Neural Networks (CNNs) for imaging and spatial data, and Recurrent Neural Networks (RNNs) for sequential and temporal data. We detail their specific applications, experimental protocols, and performance in biomarker discovery research, providing a practical framework for researchers and drug development professionals.
CNN Applications: Imaging and Spatial Biomarker Discovery
CNNs utilize convolutional layers and pooling operations to identify spatial hierarchies of features from data, making them exceptionally well-suited for analyzing image-based and spatially structured biological data [11] [50].
Key Applications and Performance
CNNs have demonstrated remarkable success across various biomarker discovery domains. The following table summarizes quantitative performances from key studies.
Table 1: Performance of CNN-based Models in Biomarker Discovery
| Application Domain | Data Type | Key Performance Metric | Reported Result | Citation |
|---|---|---|---|---|
| TNBC Subtyping | Transcriptomics (Microarray, RNA-seq) | Identification of 21-gene signature for stratification | Two subtypes with distinct overall survival (HR: 1.94, 95% CI: 1.25–3.01; P=0.0032) | [51] |
| Nuclei Analysis for Prognostication | Histopathology Whole Slide Images (WSI) | Prediction of long-term survival and pathologic complete response (pCR) | Accurate stratification of survival and pCR in patient cohorts | [50] |
| Ki67 Quantification | Histopathology Stained Slides | Inter-pathologist consistency | Substantial improvement in consistency among pathologists | [50] |
| Tumor Cellularity Assessment | Histopathology WSI | Accuracy of cellularity assessment | Improved accuracy with end-to-end DL systems | [50] |
Experimental Protocol: CNN-Based Biomarker Discovery from Histopathology Images
Objective: To discover novel prognostic biomarkers from breast cancer histopathology Whole Slide Images (WSIs) using a CNN.
Workflow: The following diagram illustrates the end-to-end protocol for processing WSIs to extract biomarker-related insights.
Materials and Reagents:
- Primary Data: Formalin-Fixed Paraffin-Embedded (FFPE) tissue sections from a retrospectively collected, clinically annotated cohort [50].
- Staining: Hematoxylin and Eosin (H&E) staining following standard clinical protocols [50].
- Equipment: Whole-slide scanner for digitizing H&E slides at 40x magnification.
- Computational Infrastructure: High-performance computing cluster with modern Graphics Processing Units (GPUs) for efficient training of complex CNN architectures [50].
Step-by-Step Procedure:
- WSI Tiling: Divide each high-resolution WSI into smaller, manageable patches (e.g., 256x256 or 512x512 pixels) to accommodate CNN input size constraints [50].
- Preprocessing: Apply color normalization to standardize stain appearance across patches from different slides and correct for technical variations [50].
- Model Training:
- Architecture: Employ a pre-trained CNN (e.g., ResNet, Inception) using transfer learning.
- Input: Processed image patches.
- Output: A predefined clinical endpoint (e.g., recurrence score, survival status, molecular subtype).
- Process: Train the CNN to learn hierarchical features—from low-level edges and textures to high-level morphological structures—that are predictive of the clinical outcome [50].
- Biomarker Extraction & Interpretation:
- Use saliency maps or Class Activation Mapping (CAM) techniques to highlight the regions within the input image that were most influential for the model's prediction, thereby identifying potential morphological biomarkers [51] [50].
- Extract second-order features from segmented nuclei (e.g., chromatin texture, nuclear envelope features) learned by the CNN for association with genomics or recurrence [50].
RNN Applications: Temporal Biomarker Discovery
RNNs are specialized for sequential data due to their internal memory, which maintains information from previous inputs. This makes them ideal for analyzing temporal biomedical data [11].
Key Applications
- Disease Progression Forecasting: Modeling trajectories of chronic diseases (e.g., neurodegenerative disorders) from sequential electronic health record (EHR) data to identify prognostic biomarkers [11].
- Treatment Response Monitoring: Analyzing longitudinal biomarker data (e.g., serial circulating tumor DNA measurements) to predict response to therapy and identify early pharmacodynamic biomarkers of resistance [11] [52].
- Time-Series Omics Analysis: Interpreting data from longitudinal transcriptomic or proteomic studies to uncover dynamic biomarkers associated with disease flare-ups or recovery [11].
Experimental Protocol: RNN for Forecasting Disease Progression
Objective: To prognosticate disease progression and discover temporal biomarkers from longitudinal clinical and omics data.
Workflow: The protocol below outlines the process of modeling sequential patient data to forecast outcomes.
Materials and Reagents:
- Primary Data: Longitudinal datasets from cohort studies, such as serial blood-based biomarker measurements (e.g., cystatin C, glycated hemoglobin) and linked clinical outcomes from repositories like the China Health and Retirement Longitudinal Study (CHARLS) [53].
- Data Curation Tools: Software for clinical data harmonization (e.g., conversion to OMOP or CDISC standards) and handling of missing values [54].
Step-by-Step Procedure:
- Data Curation and Sequencing:
- Extract and harmonize longitudinal patient data from EHRs or cohort studies, ensuring consistent formatting and units across time points [54].
- Handle missing data through imputation methods or use algorithms tolerant to missing values [54].
- Structure the data into sequential time steps for each patient.
- Model Training and Validation:
- Architecture: Implement a Long Short-Term Memory (LSTM) or Gated Recurrent Unit (GRU) network, which are RNN variants designed to mitigate the vanishing gradient problem in long sequences.
- Input: Sequential data of patient metrics over time.
- Output: A future clinical event (e.g., frailty status, disease progression) [53].
- Process: Train the RNN to recognize temporal patterns and dependencies in the data that precede the outcome of interest. Use a held-out validation set for performance evaluation.
- Temporal Biomarker Identification:
- Apply Explainable AI (XAI) techniques such as SHapley Additive exPlanations (SHAP) to the trained model [53]. SHAP analysis can quantify the contribution of each biomarker at different time points to the final prediction, revealing not only which biomarkers are important but also when they become predictive [53].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for Deep Learning-Driven Biomarker Discovery
| Item / Solution | Function / Application | Examples / Notes |
|---|---|---|
| Next-Generation Sequencing (NGS) | Enables comprehensive genomic and transcriptomic profiling for molecular biomarker discovery. | Used to identify genetic mutations (e.g., in NSCLC) and gene expression signatures [11] [55] [52]. |
| Whole-Slide Scanners | Digitizes histopathology glass slides for computational analysis. | Essential for creating the high-resolution image data used in CNN models [50]. |
| Mass Spectrometry | For large-scale identification and quantification of proteins (proteomics) and metabolites (metabolomics). | Identifies protein biomarkers and functional biomarkers like biosynthetic gene clusters (BGCs) [11] [52]. |
| Biobanks with Linked Clinical Data | Provides annotated biospecimens for model training and validation. | Cohorts like The Cancer Genome Atlas (TCGA) and CHARLS are indispensable public resources [51] [53]. |
| High-Performance Computing (GPU) | Accelerates the training of complex deep learning models. | Modern GPUs are crucial for efficient implementation of CNNs and RNNs at scale [50]. |
| Explainable AI (XAI) Tools | Interprets model predictions to identify driving features and build trust. | SHAP and saliency maps are critical for translating model outputs into biologically intelligible biomarkers [51] [53]. |
CNNs and RNNs offer a powerful, complementary toolkit for unlocking next-generation biomarkers from the spatial and temporal dimensions of complex biological data. By leveraging CNNs on histopathology images, researchers can uncover novel morphological biomarkers and genomic associations. Simultaneously, applying RNNs to longitudinal data streams allows for the discovery of dynamic, temporal biomarkers that forecast disease progression and treatment response. The integration of these technologies, guided by rigorous experimental protocols and explainable AI, holds the promise of significantly accelerating biomarker discovery and the development of personalized medicine.
The advancement of high-throughput technologies has led to an explosion of multi-modal datasets in biomedical research, spanning genomics, transcriptomics, proteomics, metabolomics, medical imaging, and clinical records [56]. Each modality provides a unique perspective on biological systems, yet their true potential lies in integration. Multi-modal data fusion enables the combination of orthogonal information, allowing different data types to complement one another and augment the overall information content beyond what a single modality can provide [56]. This is particularly relevant in biomarker discovery research, where comprehensive molecular profiles can reveal complex disease mechanisms and therapeutic targets that remain invisible when examining individual data layers in isolation [57].
The convergence of these diverse data types into integrated multi-omics approaches represents one of the most significant advances in biomarker discovery [57]. However, the integration of such heterogeneous data presents substantial challenges, including data heterogeneity, high dimensionality, small sample sizes, missing data, and batch effects [57]. To address these challenges, three primary integration strategies have emerged: early (data-level), intermediate (feature-level), and late (decision-level) fusion. Each approach offers distinct advantages and limitations, making them suitable for different research scenarios and data characteristics [57].
Biological systems operate as interconnected networks where changes at one molecular level ripple across multiple layers [57]. This systems biology perspective underpins the rationale for multi-modal integration, as disease mechanisms often involve coordinated changes across genomic, transcriptomic, proteomic, and metabolomic scales. Machine learning and deep learning methods have proven particularly effective for analyzing these complex, high-dimensional datasets and identifying reliable biomarkers that capture disease complexity with remarkable precision and predictive power [11].
Integration Methodologies
Early Integration (Data-Level Fusion)
Early integration, also known as data-level fusion, combines raw data from different omics platforms before statistical analysis or model training [57]. This approach involves merging diverse data types into a single, unified feature matrix for subsequent analysis. The advantage of early integration lies in its ability to discover novel cross-omics patterns that might be lost in separate analyses, as it preserves the maximum amount of information from all modalities [57].
Experimental Protocol for Early Integration:
- Data Collection: Gather raw data from all available modalities (e.g., genomic variants, gene expression, protein measurements, clinical variables).
- Normalization: Apply platform-specific normalization to each data type to address technical variations. Common methods include quantile normalization for gene expression data and z-score standardization for proteomic measurements [57].
- Concatenation: Merge normalized datasets into a unified feature matrix using sample identifiers as the common key.
- Dimensionality Reduction: Apply principal component analysis (PCA) or canonical correlation analysis (CCA) to reduce the high-dimensional feature space and mitigate the curse of dimensionality [57].
- Model Training: Implement machine learning algorithms (e.g., random forests, gradient boosting, regularized regression) on the integrated dataset for biomarker discovery or predictive modeling.
Early integration demands substantial computational resources and sophisticated preprocessing methods to handle data heterogeneity effectively [57]. It is particularly challenging in scenarios with high dimensionality and small sample sizes, as it increases the risk of overfitting without appropriate regularization [58].
Intermediate Integration (Feature-Level Fusion)
Intermediate integration represents a balanced approach that first identifies important features or patterns within each omics layer, then combines these refined signatures for joint analysis [57]. This strategy reduces computational complexity while maintaining cross-omics interactions, making it particularly suitable for large-scale studies where early integration might be computationally prohibitive.
Experimental Protocol for Intermediate Integration:
- Modality-Specific Feature Extraction: For each data modality, apply specialized feature selection or extraction techniques. This may include:
- Feature Alignment: Combine the extracted features from each modality into a consolidated feature set, ensuring biological relevance across platforms.
- Cross-Modal Integration: Apply integration algorithms such as MOFA (Multi-Omics Factor Analysis) or network-based integration to identify relationships across the different feature sets [57].
- Predictive Modeling: Train ensemble models or graph neural networks on the integrated feature representation to identify multi-modal biomarker signatures.
Intermediate integration allows researchers to incorporate domain knowledge about biological pathways and molecular interactions, potentially enhancing the biological interpretability of discovered biomarkers [57]. This approach balances information retention with computational feasibility, making it one of the most successful strategies for multi-omics studies [57].
Late Integration (Decision-Level Fusion)
Late integration, also known as decision-level fusion, performs separate analyses within each omics layer, then combines the resulting predictions or classifications using ensemble methods [57]. This approach offers maximum flexibility and interpretability, as researchers can examine contributions from each omics layer independently before making final predictions.
Experimental Protocol for Late Integration:
- Modality-Specific Modeling: Train separate machine learning models for each data modality using algorithms optimized for each data type:
- Prediction Generation: Obtain predictions or probability scores from each modality-specific model.
- Decision Fusion: Combine predictions using meta-learning approaches, weighted voting schemes, or stacking ensembles [57]. Weights can be optimized based on each modality's predictive performance or reliability.
- Consensus Biomarker Identification: Compare feature importance across models to identify robust biomarkers that are consistently informative across multiple modalities.
While late integration might miss subtle cross-omics interactions, it provides robustness against noise in individual omics layers and allows for modular analysis workflows [57]. This approach has demonstrated particular success in settings with high dimensionality and small sample sizes, as it reduces overfitting by building separate models for each modality [58].
Comparative Analysis of Integration Strategies
Table 1: Comparative characteristics of multi-modal data fusion strategies
| Characteristic | Early Integration | Intermediate Integration | Late Integration |
|---|---|---|---|
| Integration Level | Data-level | Feature-level | Decision-level |
| Technical Approach | Concatenation of raw data | Joint dimensionality reduction; Pattern recognition | Ensemble methods; Weighted voting |
| Computational Demand | High | Moderate | Low to Moderate |
| Interpretability | Challenging | Moderate | High |
| Robustness to Noise | Low | Moderate | High |
| Handling Data Heterogeneity | Poor | Good | Excellent |
| Preservation of Cross-Modal Interactions | High | Moderate | Low |
| Ideal Use Case | Large sample sizes; Few modalities | Moderate sample sizes; Multiple modalities | Small sample sizes; Highly heterogeneous data |
Table 2: Performance comparison of fusion strategies in cancer biomarker discovery
| Application Context | Optimal Fusion Strategy | Reported Advantage | Key Considerations |
|---|---|---|---|
| TCGA Pan-Cancer Survival Prediction [58] | Late Fusion | Consistently outperformed single-modality approaches; Higher accuracy and robustness | Particularly effective with high dimensionality and small sample sizes |
| Cancer Subtype Classification [57] | Intermediate Integration | Superior classification accuracy across multiple cancer types | Balances comprehensive information retention with computational efficiency |
| Multi-omics Biomarker Signatures [57] | Early and Intermediate Fusion | Captures complementary biological information | Requires careful normalization and handling of batch effects |
| Parkinson's Disease Detection [59] | Intermediate Fusion with Attention | High diagnostic accuracy (96.74% test accuracy) | Multi-head attention mechanism enables dynamic inter-modal weight allocation |
Experimental Protocols for Biomarker Discovery
Protocol 1: Late Fusion for Survival Prediction in Oncology
This protocol outlines the methodology for applying late fusion to predict overall survival in cancer patients, based on the AstraZeneca–artificial intelligence (AZ-AI) multimodal pipeline described in the literature [58].
Research Reagent Solutions: Table 3: Essential research reagents and computational tools for late fusion survival analysis
| Item | Function/Application | Implementation Example |
|---|---|---|
| TCGA Dataset | Provides multi-omics and clinical data for various cancer types | Genomics, transcriptomics, proteomics, clinical data |
| Python Scikit-survival | Survival analysis with machine learning models | Cox PH models, Random Survival Forests |
| Feature Selection Algorithms | Identify predictive features from high-dimensional data | Pearson/Spearman correlation, LASSO |
| Ensemble Methods | Combine predictions from modality-specific models | Weighted averaging, stacking |
Methodology:
- Data Preprocessing:
- Obtain multi-omics data (transcripts, proteins, metabolites) and clinical factors from TCGA.
- Perform modality-specific normalization: quantile normalization for gene expression, z-score standardization for proteomic data, and imputation for missing clinical values [58].
- Apply quality control measures to remove low-quality samples and features.
Modality-Specific Feature Selection:
- For each data modality, apply supervised feature selection methods such as Pearson or Spearman correlation with survival outcome [58].
- Select top-ranked features from each modality based on their association with overall survival.
- Regularize feature sets to avoid overfitting, particularly for high-dimensional data.
Individual Survival Model Training:
- Train separate survival models for each preprocessed and feature-selected modality.
- Implement a variety of algorithms including Cox Proportional Hazards models, random survival forests, and gradient boosting machines [58].
- Optimize hyperparameters for each modality-specific model using cross-validation.
Late Fusion Implementation:
- Generate predicted risk scores from each modality-specific model.
- Combine risk scores using weighted averaging based on the predictive performance (C-index) of each individual model [58].
- Alternatively, use stacking ensembles with a meta-learner to optimally combine predictions.
Validation and Interpretation:
- Evaluate fused model performance using time-dependent C-index and integrated Brier score via repeated cross-validation.
- Compare performance against unimodal benchmarks to quantify integration benefits.
- Analyze feature importance across modalities to identify key biomarkers driving predictions.
Protocol 2: Intermediate Fusion with Deep Learning for Disease Diagnosis
This protocol describes intermediate fusion for diagnostic biomarker discovery using deep learning architectures, exemplified by MultiParkNet for Parkinson's disease detection [59].
Research Reagent Solutions: Table 4: Essential research reagents and computational tools for intermediate fusion with deep learning
| Item | Function/Application | Implementation Example |
|---|---|---|
| Multi-modal Datasets | Source of heterogeneous biomedical data | MDVR-KCL (speech), Handwriting, MRI, ECG |
| Deep Learning Frameworks | Implement complex neural architectures | TensorFlow, PyTorch |
| Specialized Neural Architectures | Process modality-specific data | CNN-LSTM (audio), 3D CNN (neuroimaging) |
| Attention Mechanisms | Enable dynamic feature integration | Multi-head attention |
Methodology:
- Modality-Specific Data Processing:
- Process each data type through specialized pipelines:
- Audio signals: extract mel-frequency cepstral coefficients and apply noise reduction.
- Handwriting/drawing tasks: digitize and normalize spatial coordinates.
- Neuroimaging: apply skull stripping, spatial normalization, and intensity correction for MRI/DaTSCAN.
- Cardiovascular signals: filter noise and segment relevant waveforms from ECG.
- Process each data type through specialized pipelines:
Modality-Specific Feature Extraction:
- Implement dedicated neural network architectures for each data type:
- CNN-LSTM hybrid models for speech processing to capture spatial and temporal patterns [59].
- Dual-branch CNNs for motor skill evaluation from drawing tasks.
- 3D CNNs for volumetric neuroimaging data analysis.
- Dilated convolutional networks for cardiovascular signal interpretation.
- Implement dedicated neural network architectures for each data type:
Intermediate Feature Fusion:
- Extract high-level feature representations from the penultimate layers of each modality-specific network.
- Implement multi-head attention mechanisms to dynamically weight the importance of features across modalities [59].
- Concatenate attended features into a unified representation.
Joint Classification Model:
- Build a fully connected classification network on the fused feature representation.
- Incorporate Monte Carlo Dropout during inference to estimate prediction uncertainty [59].
- Apply confidence-weighted decision-making based on uncertainty estimates.
Validation and Clinical Translation:
- Evaluate using stratified cross-validation to account for dataset heterogeneity.
- Assess model robustness across different demographic subgroups when metadata is available.
- Plan clinical deployment pathway including integration with electronic health record systems.
Workflow Visualization
Diagram 1: Multi-modal data fusion workflow strategies
Diagram 2: Decision framework for fusion strategy selection
The integration of multi-modal data through early, intermediate, and late fusion strategies represents a powerful paradigm for biomarker discovery research. Each approach offers distinct advantages and is suited to different experimental contexts based on sample size, data heterogeneity, and research objectives. Late fusion has demonstrated particular effectiveness in scenarios with high-dimensional data and limited samples, consistently outperforming single-modality approaches in cancer survival prediction [58]. Intermediate integration provides a balanced solution that maintains cross-modal interactions while managing computational complexity, making it widely applicable across various biomarker discovery contexts [57]. Early integration preserves the maximum biological information but requires substantial computational resources and careful data handling.
The choice of integration strategy should be guided by both technical considerations and biological context. As multimodal technologies continue to advance, particularly in spatial biology and single-cell omics, the development of more sophisticated fusion methodologies will be essential [2]. Future directions should focus on adaptive fusion strategies that can dynamically weight modality importance, as well as methods that enhance interpretability to facilitate clinical translation. By strategically selecting and implementing appropriate data fusion approaches, researchers can unlock the full potential of multi-modal data to discover robust, clinically actionable biomarkers that advance precision medicine.
Application Note
Biomarkers are objectively measurable indicators of biological processes, pathological states, or responses to therapeutic interventions, playing a critical role in disease diagnosis, prognosis, and personalized treatment decisions [60]. The integration of machine learning (ML) with multi-modal data is transforming biomarker discovery from traditional single-molecule approaches to integrative, data-intensive strategies that can capture the complex biological networks underpaging diseases [11]. This application note presents two detailed case studies demonstrating successful implementation of ML-driven biomarker discovery for Alzheimer's disease (AD) and large-artery atherosclerosis (LAA), providing researchers with validated frameworks, performance metrics, and methodological protocols.
Case Study 1: Multimodal AI Framework for Alzheimer's Disease Biomarkers
Background and Clinical Need
Alzheimer's disease is biologically defined by the accumulation of amyloid beta (Aβ) plaques and neurofibrillary tau (τ) tangles, which typically require positron emission tomography (PET) imaging for assessment [61]. While accurate, PET imaging is expensive and not widely accessible, limiting its utility in routine clinical practice and creating a need for more accessible screening methods [61]. This case study demonstrates how a multimodal computational framework can estimate individual PET profiles using more readily available neurological assessments.
Experimental Framework and Performance
Researchers developed a transformer-based ML framework that integrated data from seven distinct cohorts comprising 12,185 participants to predict Aβ and τ status [61]. The model was designed to accommodate missing data, reflecting practical challenges of real-world datasets, and employed a multi-label prediction strategy to capture the interdependent roles of Aβ and τ pathology in disease progression [61].
Table 1: Performance Metrics for AD Biomarker Prediction
| Prediction Target | AUROC | Average Precision | Dataset Characteristics | Key Predictive Features |
|---|---|---|---|---|
| Amyloid Beta (Aβ) status | 0.79 | 0.78 | 12,185 participants across 7 cohorts | Neuropsychological testing, MRI volumes, APOE-ϵ4 status |
| Tau (τ) meta-temporal status | 0.84 | 0.60 | Multimodal clinical data | MRI volumes, neuropsychological battery scores |
| Regional Tau burden | 0.71-0.84 (by region) | 0.42 (macro-average) | 7 distinct brain regions | Regional brain volumes aligned with known tau deposition patterns |
The framework demonstrated robust performance even with limited feature availability, maintaining accuracy when tested on external datasets with 54-72% fewer features than the original training set [61]. Model predictions were consistent with various biomarker profiles and postmortem pathology, validating its biological relevance [61].
Incremental Value of Feature Modalities
The study quantified the incremental value of different clinical feature categories by successively adding feature groups following typical neurological work-up protocols [61]. For Aβ prediction, AUROC improved from 0.59 (demographics and medical history only) to 0.79 (all features included), while τ prediction improved from 0.53 to 0.84 [61]. The addition of MRI data led to a substantial improvement in meta-τ AUROC from 0.53 to 0.74, highlighting the particular importance of neuroimaging for tau pathology assessment [61].
Case Study 2: Machine Learning for Large-Artery Atherosclerosis Biomarkers
Background and Clinical Need
Large-artery atherosclerosis (LAA) is a leading cause of cerebrovascular disease, but diagnosis is costly and requires professional identification [62]. Traditional risk assessment tools use a limited number of predictors and discard large amounts of data contained in electronic health records (EHRs), missing the phenotypic spectrum of coronary artery disease that exists on a continuum rather than as a binary classification [63].
Experimental Framework and Performance
Researchers developed a machine learning-based in-silico score for coronary artery disease (ISCAD) derived from EHR data in two large biobanks (BioMe Biobank and UK Biobank) comprising 95,935 participants [63]. Unlike conventional binary classification approaches, ISCAD captures coronary artery disease as a quantitative spectrum representing an individual's combination of risk factors and pathogenic processes [63].
Table 2: Performance Metrics for LAA Biomarker Prediction
| Model Characteristics | Performance Metrics | Validation Approach | Key Identified Biomarkers |
|---|---|---|---|
| Logistic Regression with feature selection | AUROC: 0.92 (external validation) | 6 ML models compared; recursive feature elimination with cross-validation | Body mass index, smoking status, medications for diabetes/hypertension/hyperlipidemia |
| ISCAD score from EHR ML model | Stepwise increase in coronary stenosis, all-cause death, and recurrent MI with ascending ISCAD | Training on 35,749 participants, external testing on 60,186 participants | Multimodal EHR data: diagnoses, lab results, medications, vitals |
| Reduced feature model (27 shared features) | AUROC: 0.93 | Identification of features present across multiple models | Metabolites involved in aminoacyl-tRNA biosynthesis and lipid metabolism |
The ISCAD score demonstrated stronger associations with coronary artery disease outcomes than conventional risk scores like pooled cohort equations and polygenic risk scores [63]. The model identified participants with high ISCAD scores but no coronary artery disease diagnosis, with nearly 50% having clinical evidence of underdiagnosed disease upon manual chart review [63].
Experimental Protocols
Protocol 1: Multimodal Transformer Framework for AD Biomarker Prediction
Study Design and Cohort Description
This protocol outlines the methodology for developing and validating the transformer-based ML framework for predicting Aβ and τ status in Alzheimer's disease.
Table 3: Research Reagent Solutions for AD Biomarker Discovery
| Reagent/Resource | Specification | Functional Role | Example Sources |
|---|---|---|---|
| Multimodal clinical datasets | 7 cohorts, 12,185 participants | Training and validation data | ADNI, HABS, NACC |
| Demographic variables | Age, gender, education, medical history | Baseline risk assessment | Standardized questionnaires |
| Neuropsychological battery | Cognitive assessment scores | Functional impairment measurement | Standardized neuropsychological tests |
| Structural MRI data | Regional brain volumes | Neurodegeneration assessment | 3T MRI scanners |
| Genetic data | APOE-ϵ4 status | Genetic risk stratification | DNA extraction and genotyping |
| Plasma biomarkers | Aβ42/40 ratio | Peripheral amyloid assessment | Immunoassays |
| PET imaging data | Aβ and τ PET scans | Ground truth labels | Amyloid and tau PET tracers |
Phase 1: Data Collection and Preprocessing
- Collect multimodal data from participating cohorts, including demographic information, medical history, neuropsychological assessments, genetic markers (APOE-ϵ4), structural MRI scans, and plasma biomarkers [61]
- Process neuroimaging data to extract regional brain volumes, with particular focus on medial and neocortical temporal regions relevant to tau pathology [61]
- Implement data harmonization protocols to address variability across different cohort data collection procedures
Phase 2: Model Architecture and Training
- Implement a transformer-based neural network architecture designed to handle missing data through random feature masking during training [61]
- Configure the model for multi-label prediction of both global Aβ and meta-τ status to capture synergistic relationships between pathologies [61]
- Train the model using cross-validation techniques, optimizing hyperparameters for balanced performance across both prediction targets
Phase 3: Validation and Interpretation
- Validate model performance on external datasets with different feature availability profiles to test robustness [61]
- Perform Shapley value analysis to determine feature importance and model interpretability [61]
- Correlate model predictions with postmortem pathology data when available to establish biological validity [61]
Protocol 2: Integrated ML Framework for LAA Biomarker Discovery
Study Design and Cohort Description
This protocol details the methodology for developing and validating machine learning models for large-artery atherosclerosis biomarker discovery.
Table 4: Research Reagent Solutions for LAA Biomarker Discovery
| Reagent/Resource | Specification | Functional Role | Example Sources |
|---|---|---|---|
| Biobank datasets | BioMe Biobank, UK Biobank (95,935 participants) | Training and validation data | Institutional biobanks |
| EHR data extraction | Diagnoses, laboratory results, medications, vitals | Multimodal feature extraction | Electronic health record systems |
| Metabolomic profiling | Mass spectrometry platforms | Metabolic biomarker identification | Targeted metabolomics |
| Angiography data | Coronary stenosis measurements | Ground truth validation | Coronary angiography |
| Genetic data | Polygenic risk scores | Genetic risk assessment | Genome-wide genotyping |
Phase 1: Data Extraction and Feature Engineering
- Extract longitudinal EHR data including diagnoses, laboratory test results, medications, and vital signs from participating biobanks [63]
- Calculate conventional risk scores (pooled cohort equations) for benchmark comparisons [63]
- Process metabolomic data to identify metabolites involved in aminoacyl-tRNA biosynthesis and lipid metabolism pathways [62]
Phase 2: Model Development and Feature Selection
- Train multiple machine learning models (logistic regression, random forests, gradient boosting) for comparison [62]
- Implement recursive feature elimination with cross-validation to identify optimal feature sets [62]
- Develop the ISCAD model as a quantitative spectrum of disease probability rather than binary classification [63]
Phase 3: Validation and Clinical Utility Assessment
- Validate model performance on external cohorts to assess generalizability [63]
- Correlate ISCAD scores with angiography-measured coronary stenosis, all-cause mortality, and recurrent myocardial infarction [63]
- Identify underdiagnosed cases by flagging participants with high ISCAD scores but no clinical diagnosis of coronary artery disease [63]
The Scientist's Toolkit
Essential Research Reagent Solutions
Table 5: Essential Research Reagents for ML-Driven Biomarker Discovery
| Category | Specific Resources | Functional Application | Quality Control Considerations |
|---|---|---|---|
| Biobanks & Cohorts | ADNI, NACC, HABS, BioMe Biobank, UK Biobank | Multimodal data source for model training | Data harmonization across sites, ethical approvals |
| Omics Technologies | Genotyping arrays, RNA sequencing, Mass spectrometry proteomics/metabolomics | Molecular biomarker discovery | Batch effect correction, normalization protocols |
| Neuroimaging Platforms | 3T MRI, Amyloid and Tau PET | Neurodegeneration assessment | Standardized acquisition protocols, phantom testing |
| AI/ML Frameworks | Transformer architectures, Logistic Regression, Random Forests | Model development | Cross-validation, hyperparameter optimization |
| Bioinformatics Tools | Shapley value analysis, Recursive feature elimination | Model interpretation | Multiple testing correction, biological validation |
| Clinical Validation Resources | Postmortem pathology, Angiography data, Mortality records | Ground truth verification | Blinded assessment, standardized criteria |
These case studies demonstrate that machine learning approaches can successfully identify clinically relevant biomarkers for complex diseases like Alzheimer's disease and large-artery atherosclerosis by integrating multimodal data sources. The AD framework provides a cost-effective pre-screening tool for identifying candidates for anti-amyloid therapies, while the LAA model offers a quantitative spectrum-based approach that captures disease severity more effectively than binary classifications. Both protocols highlight the importance of robust validation, biological interpretability, and clinical utility assessment in ML-driven biomarker discovery.
Navigating the Challenges: From Data Quality to Clinical Translation
Ensuring Data Quality and Standardization in Multi-Source Datasets
In the field of machine learning (ML) for biomarker discovery, the integration of multi-source datasets has become a fundamental practice. The ability to combine diverse data types—from genomics and transcriptomics to clinical records and medical imaging—enables researchers to uncover complex biological patterns that would remain hidden in isolated data silos [11]. However, this integrative approach introduces significant challenges in ensuring data quality and standardization across disparate sources.
The quality of input data directly determines the reliability, reproducibility, and clinical applicability of ML-derived biomarkers. As noted in recent literature, "Many biomedical datasets derived from non-targeted molecular profiling or high-throughput imaging approaches are affected by multiple sources of noise and bias, and clinical datasets are often not harmonized across different patient cohorts" [54]. This reality underscores the critical importance of robust quality assurance protocols throughout the data lifecycle.
This document provides detailed application notes and protocols for ensuring data quality and standardization when working with multi-source datasets in biomarker discovery research. We present standardized evaluation frameworks, practical implementation workflows, and essential computational tools to support researchers in building reliable, clinically translatable ML models for precision medicine.
Data Quality Evaluation Framework
Multi-dimensional Quality Assessment
A comprehensive quality evaluation framework for multi-source datasets encompasses multiple dimensions, each addressing distinct aspects of data integrity. The table below summarizes key quality indicators and their evaluation methodologies:
Table 1: Data Quality Assessment Framework for Multi-Source Biomarker Datasets
| Quality Dimension | Key Evaluation Indicators | Recommended Methods | Quality Thresholds |
|---|---|---|---|
| Completeness | Proportion of missing values; Patterns of missingness | Null value analysis; MCAR/MAR/MNAR testing | <10% missing values for retained features [54] |
| Accuracy | Technical replicates consistency; Spike-in control recovery | Correlation analysis; Coefficient of variation | CV <15% for technical replicates [54] |
| Consistency | Cross-platform concordance; Unit standardization | Bland-Altman plots; Cohen's kappa | >90% concordance for overlapping measurements |
| Representativeness | Sample characteristics vs. target population; Batch effects | PCA visualization; ANOVA testing for batch effects | p > 0.05 for batch association |
| Usability | Metadata completeness; Data structure standardization | Categorical encoding checks; Schema validation | 100% required metadata fields present |
Domain-Specific Quality Metrics
Different data types require specialized quality assessment protocols. For transcriptomics data generated through next-generation sequencing, quality metrics include read quality scores, mapping rates, and genomic coverage uniformity [54]. Proteomics and metabolomics data quality is assessed through metrics such as peak intensity distribution, retention time stability, and internal standard recovery rates [54]. Clinical data quality evaluation focuses on value range adherence (e.g., biologically plausible ranges for laboratory values), temporal consistency, and coding standard compliance (e.g., ICD-10, SNOMED CT) [54].
Data Standardization Protocols
Standardization Across Data Types
Effective integration of multi-source datasets requires rigorous standardization procedures to ensure comparability and interoperability:
Table 2: Data Standardization Protocols for Multi-Omics Data Integration
| Data Type | Standardization Methods | Common Formats | Reference Databases |
|---|---|---|---|
| Genomics/Transcriptomics | FPKM/TPM normalization; Log2 transformation; Batch effect correction (ComBat) | FASTQ, BAM, GCT | GENCODE, RefSeq, Ensembl [64] |
| Epigenomics (Methylation) | Beta-value calculation; Median-centering normalization; Probe filtering | IDAT, TXT | Illumina HM450K/EPIC manifest [64] |
| Proteomics/Metabolomics | Median normalization; Probabilistic quotient normalization; Variance stabilizing transformation | mzML, mzXML | HMDB, CheBI, UniProt [54] |
| Clinical Data | Unit conversion; Categorical encoding; Temporal alignment | OMOP CDM, CDISC | ICD-10, SNOMED CT, LOINC [54] |
| Medical Imaging | Voxel size standardization; Intensity normalization; Anatomical alignment | DICOM, NIfTI | BIDS, DICOM standards [65] |
Schema Harmonization and Metadata Standards
Schema drift—where data structures evolve over time—poses significant challenges for reproducible analysis. Implement automated schema validation checks to detect additions, deletions, or modifications to data fields [66]. Maintain comprehensive data dictionaries that define each variable, its format, allowable values, and relationships to other data elements.
Adhere to established metadata standards for different data types: MIAME for microarray experiments, MINSEQE for sequencing experiments, and MIAPE for proteomics experiments [54]. For clinical data, implement the OMOP Common Data Model or CDISC standards to enable cross-institutional data sharing and analysis [54].
Implementation Workflow
The following diagram illustrates the complete workflow for ensuring data quality and standardization in multi-source biomarker datasets:
Data Quality and Standardization Workflow
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Computational Tools for Data Quality and Standardization
| Tool/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Quality Control Packages | fastQC/FQC, arrayQualityMetrics, pseudoQC, MeTaQuaC, Normalyzer | Data type-specific quality metrics calculation | NGS data, microarray data, proteomics/metabolomics data [54] |
| Normalization Tools | edgeR, DESeq2, limma, Combat | Between-sample normalization; Batch effect correction | Transcriptomics, epigenomics data preprocessing [64] |
| Data Transformation | scikit-learn, SWAN (methylation), VST (variance stabilizing) | Data scaling; Transformation; Feature engineering | Preparing data for machine learning [16] |
| Workflow Management | Snakemake, Nextflow, Airbyte | Pipeline orchestration; Connector management | Automated data processing workflows [67] |
| Metadata Standards | MIAME, MINSEQE, MIAPE, CDISC, OMOP | Metadata annotation; Schema standardization | Supporting reproducible research [54] |
Implementation Protocols
Protocol for Multi-Omics Data Quality Control
Purpose: To ensure quality and consistency across genomics, transcriptomics, epigenomics, and proteomics datasets prior to integration for biomarker discovery.
Materials:
- Raw multi-omics data files (FASTQ, IDAT, mzML, etc.)
- Quality control tools (see Table 3)
- High-performance computing environment
Procedure:
- Data Inventory: Document all available datasets, including sample sizes, platforms, and processing versions [66].
- Completeness Check: Remove features with >10% missing values across samples [54].
- Platform-Specific QC:
- For NGS data: Run FastQC to assess read quality, adapter contamination, and GC content.
- For microarray data: Use arrayQualityMetrics to evaluate intensity distributions and spatial artifacts.
- For proteomics data: Apply MeTaQuaC to monitor peak intensity stability and retention time consistency.
- Batch Effect Assessment: Perform PCA to visualize sample clustering by processing batch [64].
- Technical Validation: Calculate correlation between technical replicates (target: R² > 0.95).
- Quality Reporting: Generate comprehensive QC reports documenting all metrics and exclusion criteria.
Troubleshooting:
- If strong batch effects are detected, apply ComBat or similar batch correction methods.
- If sample mix-ups are suspected, perform genotype concordance checking when possible.
- If specific samples consistently fail QC metrics, exclude them from downstream analysis.
Protocol for Clinical Data Harmonization
Purpose: To standardize clinical data from multiple sources into a consistent format suitable for machine learning.
Materials:
- Source clinical data (EHR extracts, case report forms, registries)
- Terminology standards (ICD-10, SNOMED CT, LOINC)
- Data transformation tools (Python/R scripts)
Procedure:
- Variable Mapping: Create crosswalk between source variables and target data model (e.g., OMOP CDM) [54].
- Unit Standardization: Convert all measurements to consistent units (e.g., mmHg for blood pressure).
- Categorical Encoding: Map categorical values to standard terminologies (e.g., ICD-10 for diagnoses).
- Temporal Alignment: Define index date and align all temporal measurements relative to this date.
- Range Validation: Implement value range checks based on clinical plausibility (e.g., adult systolic BP 70-250 mmHg).
- Derived Variable Calculation: Compute clinically relevant scores (e.g., Charlson Comorbidity Index).
Validation:
- Cross-validate a subset of transformed data against original source documents.
- Assess consistency of derived variables across different calculation methods.
- Perform sensitivity analyses to evaluate impact of transformation decisions.
Machine Learning Integration
Data Preparation for ML
The transition from standardized data to ML-ready datasets requires additional considerations. Feature selection becomes crucial to manage the high dimensionality typical of multi-omics data. Apply recursive feature elimination with cross-validation or model-based importance ranking to identify the most informative features [16]. For multi-modal data integration, consider early, intermediate, or late integration strategies depending on the specific ML approach and biological question [54].
Implement rigorous train-test splits that account for potential data leakage, especially when multiple samples come from the same patient or institution. Consider grouped splitting strategies to prevent overly optimistic performance estimates [16].
Quality-Aware Machine Learning
Incorporate data quality metrics directly into ML workflows through quality-weighted models or uncertainty-aware algorithms. For example, assign lower weights to samples with poorer quality metrics or use quality indicators as additional input features where appropriate.
The following diagram illustrates the integration of quality control processes with machine learning workflows:
Quality-Aware ML Integration
Ensuring data quality and standardization in multi-source datasets is not merely a preliminary step but a continuous process that underpins the entire biomarker discovery pipeline. By implementing the protocols and methodologies outlined in this document, researchers can significantly enhance the reliability, reproducibility, and clinical translatability of ML-derived biomarkers.
The integration of comprehensive quality assessment, rigorous standardization procedures, and quality-aware machine learning creates a robust foundation for discovering meaningful biological insights from complex, multi-modal data. As the field advances, continued development of automated quality monitoring systems and adaptive standardization frameworks will further accelerate the translation of computational discoveries into clinical practice.
Adherence to these principles is particularly crucial in precision medicine, where biomarker-driven decisions directly impact patient care and treatment outcomes. Through conscientious attention to data quality and standardization, researchers can fully leverage the potential of multi-source data integration to advance biomarker discovery and personalized therapeutics.
Combatting Overfitting in Small Sample Size, High-Dimensional Settings
In the field of biomarker discovery, researchers increasingly face the challenge of developing predictive models from datasets where the number of features (p) vastly exceeds the number of samples (n)—a scenario known as the "high-dimensional, low sample size" (HDLSS) problem [68]. This imbalance creates a perfect environment for overfitting, where models appear to perform excellently on training data but fail to generalize to new, unseen data [68] [69]. The consequences are particularly severe in biomedical research, where overfitted models can lead to spurious biomarker identification, wasted resources, and ultimately, unreliable clinical decisions [70] [69]. This application note provides detailed protocols and frameworks specifically designed to combat overfitting in small sample size, high-dimensional settings, with direct application to biomarker discovery research.
Quantitative Evidence: Assessing the Overfitting Problem
The table below summarizes key evidence from studies that have quantified overfitting risks and performance of mitigation strategies in high-dimensional biological data settings.
Table 1: Quantitative Evidence of Overfitting and Mitigation Performance in High-Dimensional Settings
| Study Context | Key Findings on Overfitting | Performance Metrics | Citation |
|---|---|---|---|
| General HDLSS Settings | Overfitting occurs even with p < n; 10:1 sample-to-predictor ratio insufficient to prevent overfitting | Test set accuracy: ~50% (null case) vs. training accuracy: up to 100% | [68] |
| Biomarker Risk Prediction Models | Models with large biomarker panels prone to overfitting; small p-values misleading without improved prediction | High odds ratios (e.g., 36.0) needed for clinical predictive value | [70] |
| HiFIT Framework Simulation | HFS outperformed Lasso, PC, HSIC, and MIC in high-dimensional nonlinear scenarios (p=10,000) | Identified largest number of causal features; robust to high dimensions | [71] |
| LAA Biomarker Discovery | ML with feature selection improved AUC from 0.89 to 0.92; 27 shared features achieved AUC=0.93 | AUC: 0.92-0.93 with feature selection; Accuracy: Improved with RFE-CV | [16] |
| AD Biomarker Discovery | Random forest model with robust feature selection on high-dimensional proteomics data | AUC: 0.84 (±0.03) | [72] |
Experimental Protocols
Protocol 1: Hybrid Feature Screening (HFS) for Biomarker Pre-screening
Purpose: To reduce feature dimensionality prior to model building by combining multiple dependency metrics, minimizing the risk of missing important biomarkers that might be overlooked by single-metric approaches [71].
Materials:
- High-dimensional dataset (e.g., omics data) with sample size n and feature number p (where p ≫ n)
- Computing environment with R and HiFIT package (https://github.com/BZou-lab/HiFIT)
Procedure:
- Calculate Multiple Association Metrics: For each feature, compute multiple marginal association measures with the outcome variable:
- Linear associations: Pearson correlation
- Monotonic nonlinear associations: Spearman correlation
- Complex nonlinear associations: Maximal Information Coefficient (MIC), Hilbert-Schmidt Independence Criterion (HSIC) [71]
- Normalize and Combine Scores: Normalize each metric to a common scale and compute the HFS score as an ensemble of these normalized metrics
- Determine Data-Driven Cutoff: Apply isolation forest algorithm to the HFS scores to identify an optimal cutoff distinguishing important features from noise [71]
- Generate Candidate Feature Set: Retain features with HFS scores above the determined cutoff for downstream analysis
Validation:
- Compare HFS performance against individual screening methods (Lasso, PC, SPC, MIC, HSIC) through simulation studies
- Evaluate using rank of causal features relative to all features under varying dimensionalities (p = 500, 1000, 10000) [71]
Protocol 2: Permutation-Based Feature Importance Test (PermFIT) for Model Refinement
Purpose: To evaluate feature importance scores while adjusting for confounding effects under complex association settings, providing a computationally efficient refinement of pre-screened features [71].
Materials:
- Pre-screened feature set from HFS protocol
- Machine learning model (e.g., DNN, RF, SVM, XGBoost)
- Computing environment with PermFIT implementation [71]
Procedure:
- Train Initial Model: Using the pre-screened features from HFS, train a machine learning model to predict the outcome
- Establish Baseline Performance: Calculate the model's performance (e.g., AUC, accuracy) on a validation set
- Permute Feature Values: For each feature individually, randomly permute its values across samples to break its association with the outcome
- Re-evaluate Performance: Recalculate model performance after each feature permutation
- Calculate Importance Scores: Compute feature importance as the difference between baseline performance and performance after permutation
- Statistical Testing: Repeat permutation process multiple times to generate a null distribution and calculate p-values for each feature's importance
Validation:
- Apply to real-world datasets (e.g., weight loss after bariatric surgery, TCGA kidney cancer RNA-seq data)
- Compare prediction accuracy of final HiFIT model against other methods [71]
Protocol 3: Cross-Validation and External Validation Framework
Purpose: To provide realistic performance estimates and ensure model generalizability through rigorous validation protocols [70].
Materials:
- Entire dataset with samples from the target population
- Computing environment with scikit-learn (Python) or equivalent toolkit
Procedure:
- Data Splitting:
- Internal Validation:
- Perform hyperparameter tuning using nested cross-validation within training set only
- Apply multiple resampling techniques (bootstrapping, cross-validation) to assess model stability [70]
- External Validation:
- Performance Reporting:
Visualizing Workflows and Relationships
HiFIT Framework Workflow
Model Validation Strategy
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for Combatting Overfitting
| Tool/Reagent | Function | Application Context | Key Features |
|---|---|---|---|
| HiFIT R Package | Hybrid feature screening and permutation importance testing | High-dimensional omics data integration | Combines multiple dependency metrics; Data-driven cutoff determination [71] |
| Scikit-learn | Machine learning library with regularization and cross-validation | General biomarker discovery pipelines | L1/L2 regularization; k-fold CV; Feature selection methods [16] [69] |
| TensorFlow/PyTorch | Deep learning frameworks with built-in regularization | Complex nonlinear biomarker relationships | Dropout layers; Early stopping; Custom loss functions [69] |
| Bioconductor | Bioinformatics-specific preprocessing and analysis | Genomic and transcriptomic data | Specialized methods for high-dimensional biological data [69] |
| SMOTE | Synthetic minority over-sampling technique | Handling class imbalance in small datasets | Generates synthetic samples to balance classes [72] |
| Absolute IDQ p180 Kit | Targeted metabolomics quantification | Metabolic biomarker discovery | Quantifies 194 endogenous metabolites from 5 compound classes [16] |
| Tandem Mass Tag (TMT) | Multiplexed proteomics quantification | High-dimensional proteomic biomarker discovery | Enables parallel multiplexing for relative protein abundance [72] |
Discussion and Implementation Guidelines
The protocols presented herein address the critical challenge of overfitting through a multi-layered approach. The Hybrid Feature Screening method specifically tackles the dimensionality problem by leveraging an ensemble of association metrics, overcoming limitations of individual methods that may miss important biomarkers with complex relationship patterns [71]. Subsequent refinement using PermFIT enables accurate feature importance assessment while accounting for complex interactions and confounding effects [71].
For implementation in biomarker discovery pipelines, researchers should prioritize external validation using completely independent datasets, as this remains the most rigorous approach for establishing generalizability [70]. Additionally, the choice of performance metrics should align with the clinical or biological context, with AUC, sensitivity, specificity, and calibration all providing complementary information about model utility [13] [70].
Emerging approaches including explainable AI and federated learning show promise for further enhancing model robustness and interpretability in high-dimensional settings [73] [69]. By adopting the frameworks and protocols outlined in this application note, biomarker researchers can significantly improve the reliability and reproducibility of their predictive models, accelerating the translation of discoveries to clinical applications.
The integration of Artificial Intelligence (AI) into biomarker discovery presents a paradigm shift for precision medicine, yet the "black-box" nature of complex machine learning (ML) models often hinders their clinical adoption [11]. Explainable AI (XAI) has substantial transformative potential to bridge this gap by ensuring that AI-driven decisions are not only accurate but also transparent, fair, and reasonable [74]. In high-stakes biomedical domains, the ability to understand and trust an AI's prediction is not merely an academic exercise; it is a prerequisite for building trust among researchers, clinicians, and patients, and for ensuring that models learn meaningful biological patterns rather than spurious correlations [75] [4]. This Application Note provides a detailed framework and practical protocols for the implementation of XAI strategies within biomarker research workflows, aiming to move beyond pure prediction toward actionable biological insight.
XAI Taxonomy and Core Techniques
Explainable AI approaches can be broadly categorized into interpretable models and explainable models [74]. Interpretable models, such as linear regression or decision trees, are inherently transparent by design. In contrast, complex models like neural networks or ensemble methods require post-hoc explainability techniques to elucidate their inner workings [74] [76]. The following table summarizes the primary XAI techniques relevant to biomarker discovery.
Table 1: Taxonomy of Core Explainable AI (XAI) Techniques
| Category | Method | Core Function | Best-Suited Model Types |
|---|---|---|---|
| Interpretable Models | Logistic Regression | Models with direct, transparent parameters for risk scoring and planning [74] [16]. | Generalized Linear Models |
| Decision Trees | Tree-based logic flows for classification and patient segmentation [74] [77]. | Single Tree Structures | |
| Model-Agnostic Methods | SHAP (SHapley Additive exPlanations) | Uses game theory to assign feature importance based on marginal contribution to the prediction [74] [77]. | Any black-box model (e.g., Tree-based, Neural Networks) |
| LIME (Local Interpretable Model-agnostic Explanations) | Approximates black-box predictions locally with a simple, interpretable model [74] [77]. | Any black-box classifier or regressor | |
| Counterfactual Explanations | Shows how small changes to specific input features would alter the model's decision [74]. | Any black-box model | |
| Model-Specific Methods | Feature Importance (e.g., Permutation) | Measures the decrease in model performance when a feature is randomly shuffled [74]. | Tree-based ensembles (Random Forest, XGBoost) |
| Attention Weights | Highlights input components (e.g., words in text, regions in genomics) most attended to by the model [74]. | Transformer models, NLP tasks | |
| Activation Analysis | Examines neuron activation patterns in neural networks to interpret outputs [74]. | Deep Neural Networks (CNNs, RNNs) |
Application Note: An XAI Protocol for Biomarker Discovery
This section outlines a standardized, end-to-end protocol for integrating XAI into a typical biomarker discovery pipeline, using a transcriptomic case study as a reference.
Experimental Workflow and Visualization
The following diagram illustrates the core workflow for an XAI-driven biomarker discovery project, from data preparation to model interpretation.
Detailed Experimental Protocol
Objective: To identify a robust panel of transcriptomic biomarkers for disease endotyping and build a transparent predictive model.
Step 1: Data Preparation and Preprocessing
- Data Input: Collect and integrate multi-omics data (e.g., RNA-seq from public repositories like TCGA or GEO) and corresponding clinical metadata [4].
- Quality Control (QC): Perform rigorous QC. Use unsupervised learning methods like Principal Component Analysis (PCA) or t-SNE to visualize data structure, identify batch effects, and detect potential outliers [4].
- Data Preprocessing: Impute missing values using appropriate methods (e.g., mean imputation for low missingness) [16]. Normalize data to correct for technical variation (e.g., TPM for RNA-seq, followed by log2 transformation). Encode categorical clinical variables.
Step 2: Model Training and Validation
- Model Selection: Choose a set of candidate models. It is critical to include at least one inherently interpretable model (e.g., Logistic Regression) as a benchmark against more complex, potentially higher-performing black-box models (e.g., Random Forest, XGBoost) [74] [16].
- Training: Implement a tenfold cross-validation scheme on the training set to tune hyperparameters and avoid overfitting [16].
- Evaluation: Hold out a separate test set (e.g., 20% of data) for final, unbiased evaluation. Report standard performance metrics: Area Under the Receiver Operating Characteristic Curve (AUC), accuracy, precision, and recall [16].
Step 3: Global Explanation and Biomarker Candidate Identification
- Technique: Apply SHAP or permutation-based feature importance to the trained model [74] [77].
- Procedure: Calculate SHAP values for the entire test set. Generate a SHAP summary plot, which combines feature importance with the impact of each feature on the model output.
- Output: A ranked list of features (e.g., genes) based on their mean absolute SHAP values, representing their overall contribution to the model's predictions. This list forms the primary source for biomarker candidates.
Step 4: Local Explanation and Case Analysis
- Technique: Use LIME or SHAP force plots to explain individual predictions [77].
- Procedure: Select specific instances of interest from the test set (e.g., misclassified samples, high-risk patients). For each instance, run LIME to create a local surrogate model that approximates the black-box model's behavior in the vicinity of that instance.
- Output: A visualization and simplified coefficients showing which features drove the prediction for that specific patient, aiding in clinical interpretation and hypothesis generation.
Step 5: Biological Validation and Reporting
- Functional Enrichment: Input the top-ranked biomarker candidates from Step 3 into enrichment analysis tools (e.g., DAVID, Enrichr) to identify over-represented biological pathways (e.g., "aminoacyl-tRNA biosynthesis" or "lipid metabolism" as found in LAA studies) [16].
- Causal Reasoning: Critically evaluate whether the identified biomarkers are likely to be causally involved in the disease or are merely correlated. This may involve literature mining or designing follow-up experimental studies [4].
- Reporting: Document the final model, its performance, the top biomarker candidates with their XAI-derived importance scores, and the associated biological pathways.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagent Solutions for XAI in Biomarker Discovery
| Tool/Reagent | Category | Primary Function in XAI Workflow |
|---|---|---|
| SHAP Library [77] | Software Library | A unified framework for calculating and visualizing feature attributions for any model. |
| LIME Package [77] | Software Library | Generates local, model-agnostic explanations for individual predictions. |
| scikit-learn [16] | Software Library | Provides a wide array of machine learning models (interpretable and black-box) and data preprocessing utilities. |
| Captum [75] | Software Library | A PyTorch library for model interpretability, including gradient-based attribution methods. |
| Absolute IDQ p180 Kit [16] | Biomarker Assay Kit | Targeted metabolomics kit for quantifying plasma metabolites; example of high-throughput omics data generation. |
| TCGA, GEO, ENCODE [4] | Data Repository | Publicly available databases providing large-scale, multi-omics datasets for training and validating models. |
Critical Considerations for Deployment
- Performance-Interpretability Trade-off: Acknowledge and document the trade-off. While a complex model like XGBoost might achieve a higher AUC (e.g., 0.92 [16]), a well-regularized logistic regression model offers inherent transparency, which may be preferable in critically assessed clinical settings [74].
- Human Factors and Appropriate Reliance: XAI does not guarantee improved human decision-making. Studies show variability in how clinicians respond to explanations; some may perform worse, and increased confidence does not always correlate with accuracy [78]. It is crucial to define and aim for appropriate reliance—where users rely on the model when it is correct and ignore it when it is wrong [78].
- Context-Dependent Explanations: Tailor explanations to the end-user. The explanatory needs of a data scientist debugging a model differ from those of a clinician making a treatment decision [75]. Future XAI systems should strive for context- and user-dependent explanations [75].
- From Correlation to Causation: Use XAI outputs as powerful starting points for forming hypotheses. True biomarker validation requires rigorous experimental follow-up to establish causal mechanistic links, moving beyond computationally identified correlations [4].
Addressing Data Heterogeneity, Batch Effects, and Technical Noise
In the field of machine learning (ML) for biomarker discovery, data heterogeneity and technical noise present significant obstacles to developing robust, clinically applicable models. Batch effects—systematic technical variations introduced when data are collected in different batches, times, or using different protocols—can confound biological signals and lead to misleading conclusions [79] [80]. As multi-omics technologies generate increasingly complex datasets at genomic, transcriptomic, proteomic, and metabolomic levels, the need for effective strategies to address these technical artifacts has become paramount for research reproducibility and clinical translation [81] [11]. The integration of machine learning with high-throughput biological data further amplifies these challenges, as models may inadvertently learn technical artifacts rather than genuine biological signals, compromising their predictive power and generalizability [11]. This application note provides a structured framework for identifying, correcting, and mitigating these issues within ML-driven biomarker research, with specific protocols and tools for maintaining data integrity throughout the discovery pipeline.
Understanding Batch Effects and Technical Variation
Batch effects originate from multiple technical sources throughout the experimental workflow. In sequencing-based approaches, these include variations in reagent lots, personnel, equipment calibration, sequencing platforms, and library preparation protocols [80]. These technical factors introduce systematic variations that can obscure true biological signals, particularly in sensitive single-cell and spatial omics technologies [79] [2]. The impact extends across the biomarker development pipeline, affecting cell type identification, clustering analyses, differential expression testing, and ultimately, the validation of candidate biomarkers [79].
In the context of ML for biomarker discovery, batch effects pose particular challenges. Models trained on confounded data may demonstrate excellent performance on training datasets but fail to generalize to independent cohorts or different experimental conditions [11]. This limitation severely impacts the translational potential of discovered biomarkers, as clinical implementation requires consistent performance across diverse patient populations and healthcare settings [60] [17].
Computational Methods for Batch Effect Correction
Comparative Analysis of Correction Methods
Table 1: Comparison of Single-Cell RNA Sequencing Batch Correction Methods
| Method | Input Data Type | Correction Approach | Key Advantages | Performance Notes |
|---|---|---|---|---|
| Harmony | Normalized count matrix | Soft k-means clustering with linear correction in embedded space | Fast runtime; preserves biological variation; handles multiple batches | Consistently high performance across multiple benchmarks; recommended as first choice [79] [82] |
| LIGER | Normalized count matrix | Integrative non-negative matrix factorization with quantile alignment | Separates technical and biological variation; identifies shared factors | Good performance but may alter data considerably in some tests [79] [82] |
| Seurat | Normalized count matrix | Canonical Correlation Analysis (CCA) and mutual nearest neighbors | Identches integration "anchors"; widely adopted in community | Good performance in benchmarks; may introduce detectable artifacts [79] [80] [82] |
| ComBat-seq | Raw count matrix | Empirical Bayes with negative binomial model | Directly models count data; improves on original ComBat | Introduces artifacts in some testing scenarios [79] [83] |
| BBKNN | k-NN graph | Graph-based correction on neighborhood graph | Computationally efficient; preserves local structures | Limited to graph-based analyses; may overcorrect in some cases [79] |
| SCVI | Raw count matrix | Variational autoencoder modeling | Probabilistic framework; handles complex batch effects | Alters data considerably in benchmark tests [79] |
Benchmarking Insights and Performance
Comprehensive benchmarking studies evaluating batch correction methods have identified key performance differences under various scenarios. In a 2020 benchmark assessing 14 methods across ten datasets, Harmony, LIGER, and Seurat 3 demonstrated the strongest performance for batch integration while maintaining cell type separation [82]. Due to its significantly shorter runtime, Harmony was recommended as the initial method to try in analytical pipelines [82]. A 2025 study further emphasized that many methods create measurable artifacts during correction, with Harmony being the only method that consistently performed well across all tests without substantially altering the underlying biological signal [79].
Performance varies considerably across different data scenarios. For datasets with identical cell types across different sequencing technologies, methods like Harmony and Seurat 3 effectively integrate batches while preserving cell type purity. In more challenging scenarios with partially overlapping cell types or significant compositional differences, methods that can distinguish between technical and biological variation, such as LIGER, may provide advantages [79] [82].
Table 2: Method Recommendations for Different Data Scenarios
| Data Scenario | Recommended Methods | Considerations |
|---|---|---|
| Identical cell types, different technologies | Harmony, Seurat 3 | Focus on batch mixing metrics while monitoring biological signal preservation |
| Non-identical cell types | LIGER, Harmony | Methods must distinguish technical artifacts from true biological differences |
| Multiple batches (>5) | Harmony, ComBat-seq | Computational efficiency becomes critical with large batch numbers |
| Large datasets (>100,000 cells) | BBKNN, Harmony | Memory usage and scalability are primary concerns |
| Downstream differential expression | ComBat-seq, Harmony | Preservation of biological variation for DEG detection is essential |
Experimental Protocols for Batch Effect Management
Proactive Experimental Design
Effective management of batch effects begins with proactive experimental design rather than relying solely on computational correction [80]. The following protocols should be implemented during study planning:
- Sample Randomization: Distribute biological conditions of interest (e.g., case/control) across batches, sequencing runs, and processing dates to avoid confounding biological and technical effects.
- Reference Standards: Include common reference samples or cell lines in each batch to monitor technical variation and assess correction efficacy.
- Balanced Processing: Process samples in a balanced manner across technical variables (reagent lots, instruments, personnel) whenever possible.
- Metadata Documentation: Systematically record all technical variables (processing date, reagent lot numbers, instrument IDs, operator) to enable downstream modeling of these factors.
Computational Correction Protocol
The following step-by-step protocol provides a standardized workflow for batch effect correction in biomarker discovery studies:
Protocol: Batch Effect Correction for scRNA-seq Data
Data Preprocessing
- Perform standard quality control (mitochondrial gene percentage, unique molecular identifier counts)
- Normalize using method appropriate for technology (SCTransform for 10x Genomics data)
- Select highly variable genes for downstream integration
Batch Effect Assessment
- Visualize uncorrected data using UMAP/t-SNE, colored by batch and cell type
- Calculate batch mixing metrics (kBET, LISI) before correction
- Assess degree of batch confounding using clustering metrics (ARI)
Method Selection and Application
- Start with Harmony as default method due to strong benchmark performance
- For complex batch structures or when distinguishing technical/biological variation is crucial, test LIGER as alternative
- Run selected method with default parameters initially
Quality Control and Validation
- Visualize corrected data using UMAP/t-SNE, colored by batch and cell type
- Recalculate batch mixing metrics (kBET, LISI) to assess improvement
- Verify biological signal preservation using cell type clustering metrics (ASW, ARI)
- Check for overcorrection (merging of distinct cell types) or undercorrection (batch-specific clusters)
Downstream Analysis
- Proceed with cell type identification, differential expression, and trajectory analysis on corrected data
- For methods correcting embeddings rather than counts (Harmony, BBKNN), use corrected embeddings for clustering and visualization
- For methods correcting count matrices (ComBat-seq), use corrected counts for differential expression
Integration with Machine Learning Pipelines
Strategic Considerations for ML Workflows
When incorporating batch correction into ML pipelines for biomarker discovery, several strategic considerations emerge:
- Pre-correction vs. Model Integration: Determine whether to correct data before model training or include batch as a covariate in the model. For deep learning approaches, batch information can be incorporated directly into the model architecture [11].
- Validation Strategy: Implement rigorous validation using independent datasets processed in different batches to assess model generalizability.
- Multi-omics Integration: For integrated analysis of genomics, transcriptomics, proteomics, and metabolomics data, apply appropriate batch correction methods to each data layer before integration [81].
- Temporal Stability: For longitudinal studies, ensure batch correction methods maintain temporal relationships and biological trajectories.
ML-Specific Validation Protocols
Beyond standard batch correction validation, ML pipelines require additional checks:
- Batch-Aware Cross-Validation: Implement batch-stratified cross-validation to ensure each fold contains representative samples from all batches.
- Batch Effect Metrics in Model Performance: Monitor whether model performance differs across batches, indicating residual technical effects.
- Ablation Studies: Train models with and without batch correction to quantify its impact on predictive performance.
- Feature Importance Analysis: Examine whether technical factors disproportionately influence feature importance in the model.
Table 3: Research Reagent Solutions for Batch Effect Management
| Resource Category | Specific Tools/Reagents | Function in Batch Effect Management |
|---|---|---|
| Reference Materials | Commercial reference cell lines (e.g., 10x Genomics cell multiplexing); Synthetic RNA spike-ins | Normalization standards across batches; Technical variation monitoring |
| Standardized Kits | Fixed-lot reagent kits; Integrated sample preparation systems | Reduce technical variability from reagent lots and protocol deviations |
| Quality Control Assays | Bioanalyzer/TapeStation; qPCR quantification kits; Viability assays | Pre-sequencing quality assessment; Exclusion of technically compromised samples |
| Computational Tools | Harmony, LIGER, Seurat, Scanny; kBET, LISI metric implementations | Batch effect correction; Correction efficacy quantification |
| Data Management | Laboratory Information Management Systems (LIMS); Electronic lab notebooks | Comprehensive metadata tracking; Sample provenance documentation |
Effective management of data heterogeneity, batch effects, and technical noise is not merely a preprocessing step but a fundamental component of rigorous biomarker discovery. The integration of proactive experimental design with computational correction methods—selected appropriately for specific data scenarios—forms the foundation for robust, reproducible ML models in biomarker research. As the field advances toward increasingly complex multi-omics integration and spatial profiling technologies, continued development and benchmarking of batch effect management strategies will remain essential for translating computational discoveries into clinically meaningful biomarkers.
Ethical, Regulatory, and Data Privacy Considerations for Clinical Adoption
The integration of machine learning (ML) into biomarker discovery represents a paradigm shift in precision medicine, enabling the identification of novel diagnostic, prognostic, and predictive biomarkers from complex multi-omics datasets [11]. However, the translation of these research findings into clinically adopted tools presents significant ethical, regulatory, and data privacy challenges that researchers must navigate. ML technologies can derive new insights from healthcare data and learn from real-world experience to improve performance, but these capabilities also introduce unique considerations across the product lifecycle [84]. This application note provides a structured framework for addressing these considerations, ensuring that ML-driven biomarkers can be safely, effectively, and ethically integrated into clinical practice and drug development pipelines.
Ethical Considerations in ML-Driven Biomarker Research
Core Ethical Principles and Operationalization
The ethical development and deployment of ML-based biomarkers should be guided by four core principles: autonomy, justice, non-maleficence, and beneficence [85]. These principles must be operationalized throughout the research lifecycle through specific assessment dimensions and mitigation strategies.
Table 1: Ethical Framework for ML Biomarker Research
| Ethical Principle | Definition | Operationalization in ML Biomarker Research | Common Risk Scenarios |
|---|---|---|---|
| Autonomy | Respect for individual self-determination and decision-making | Informed consent processes for data use; explainable AI for clinician comprehension; patient override mechanisms for AI recommendations | Inadequate consent for secondary data uses; black-box algorithms undermining clinical understanding |
| Justice | Fairness in distribution of benefits and burdens; avoidance of discrimination | Representative training datasets; bias detection and mitigation protocols; equitable access across populations | Algorithmic bias against underrepresented racial, ethnic, or socioeconomic groups in training data |
| Non-maleficence | Avoidance of harm to patients and stakeholders | Rigorous validation against clinical outcomes; cybersecurity measures; continuous safety monitoring | Patient harm from inaccurate predictions; data breaches exposing sensitive health information |
| Beneficence | Promotion of patient and societal welfare | Clinical utility assessments; improvement of diagnostic accuracy; efficiency gains in drug development | Deployment of tools with marginal clinical benefit; diversion of resources from proven interventions |
Addressing Algorithmic Bias and Fairness
A primary ethical challenge in ML biomarker development is algorithmic bias, which can perpetuate and amplify healthcare disparities. Bias can originate from multiple sources throughout the ML pipeline, requiring comprehensive mitigation strategies.
Table 2: Sources and Mitigation Strategies for Algorithmic Bias
| Bias Source | Description | Impact on Biomarker Performance | Mitigation Strategies |
|---|---|---|---|
| Training Data Bias | Underrepresentation of certain demographic groups in training datasets | Reduced accuracy and predictive performance for underrepresented populations | Intentional cohort recruitment; data augmentation techniques; synthetic data generation |
| Label Bias | Inaccurate or inconsistently applied diagnostic labels in reference standards | Propagation of historical diagnostic inaccuracies into predictive models | Multi-adjudicator consensus panels; standardized labeling protocols; periodic label audits |
| Measurement Bias | Systemic differences in data collection methods across sites or populations | Spurious correlations that fail to generalize across care settings | Data harmonization protocols; cross-site calibration studies; algorithmic fairness constraints |
| Feature Selection Bias | Omission of clinically relevant variables that differentially affect populations | Model reliance on proxies for protected attributes leading to discrimination | Multidisciplinary feature selection; causal reasoning frameworks; fairness-aware feature selection |
The following diagram illustrates the ethical evaluation framework for ML-based biomarker development across the research lifecycle:
Regulatory Frameworks for AI/ML-Enabled Biomarkers
FDA Regulatory Pathways for AI/ML-Enabled Devices
Biomarkers intended for clinical use are typically regulated as medical devices by the U.S. Food and Drug Administration (FDA). The FDA has established specific frameworks for artificial intelligence and machine learning-enabled medical devices, recognizing their unique characteristics, including the ability to learn and adapt over time [84]. The regulatory approach depends on the device's risk classification and intended use.
Table 3: FDA Regulatory Pathways for AI/ML-Enabled Biomarkers
| Pathway | Risk Classification | When Used | Key Requirements | Examples for ML Biomarkers |
|---|---|---|---|---|
| 510(k) Clearance | Class II (Moderate Risk) | Device is substantially equivalent to a legally marketed predicate device | Performance comparison to predicate; analytical validation; computational modeling | ML algorithms for laboratory data analysis with existing non-ML counterparts |
| De Novo Classification | Class I or II (Low to Moderate Risk) | No predicate exists; novel device with low-to-moderate risk | Comprehensive performance data; risk analysis; clinical validation | First-of-its-kind diagnostic algorithm for specific disease subtyping |
| Premarket Approval (PMA) | Class III (High Risk) | Devices that support or sustain human life or present potential unreasonable risk | Extensive clinical trials; manufacturing information; post-approval studies | ML-based biomarkers for cancer diagnosis or treatment selection |
The FDA's approach emphasizes a Total Product Lifecycle (TPLC) framework, which assesses devices across their entire lifespan from design through deployment and post-market monitoring [86]. For AI/ML-enabled devices, the FDA has also developed Good Machine Learning Practice (GMLP) principles, emphasizing transparency, data quality, and ongoing model maintenance [86]. A significant development is the requirement for a Predetermined Change Control Plan (PCCP), which allows manufacturers to pre-specify planned modifications to AI/ML models while maintaining regulatory compliance [84].
Global Regulatory Landscape
Regulatory approaches to AI/ML-enabled biomarkers vary globally, presenting challenges for multi-national research and deployment efforts. The European Union's AI Act classifies many healthcare AI systems as "high-risk," imposing additional requirements on top of existing medical device regulations [87]. Other regions are developing their own frameworks, with efforts underway through bodies like the International Medical Device Regulators Forum (IMDRF) to align approaches and reduce regulatory fragmentation [86].
Data Privacy and Security Protocols
Global Data Protection Frameworks
ML biomarker research typically involves processing sensitive health information, requiring compliance with diverse data protection regulations. These frameworks establish standards for data collection, processing, and sharing, with significant implications for multi-site research collaborations.
Table 4: Key Data Protection Frameworks for Health Research
| Regulatory Framework | Geographic Scope | Key Requirements | Implications for ML Biomarker Research |
|---|---|---|---|
| HIPAA (Health Insurance Portability and Accountability Act) | United States | Safeguards for protected health information (PHI); breach notification; limited uses and disclosures | Requirements for de-identification; data use agreements; security safeguards for multi-site research |
| GDPR (General Data Protection Regulation) | European Union | Lawful basis for processing; data minimization; purpose limitation; individual rights | Explicit consent requirements; documentation of processing activities; cross-border transfer restrictions |
| CCPA (California Consumer Privacy Act) | California, USA | Consumer rights regarding personal information; transparency requirements; opt-out mechanisms | Compliance obligations for researchers accessing California resident data, even outside California |
| MHMD (My Health My Data Act) | Washington State, USA | Extra protections for consumer health data; broad definitions; private right of action | Expansive definition of health data may encompass information not traditionally considered health-related |
Technical Safeguards for Privacy-Preserving Analytics
Implementing appropriate technical safeguards is essential for protecting sensitive health data used in ML biomarker research while maintaining data utility. Emerging technologies offer promising approaches to balance data access with privacy protection.
De-identification and Anonymization: Advanced de-identification techniques beyond simple identifier removal, including masking, generalization, and perturbation methods that preserve statistical utility while minimizing re-identification risk [88].
Federated Learning: A distributed ML approach where model training occurs across multiple decentralized devices or servers holding local data samples, without exchanging the data itself. This approach is particularly valuable for multi-institutional biomarker research while maintaining data locality [88].
Differential Privacy: A mathematical framework that provides formal privacy guarantees by adding carefully calibrated noise to query results or during model training, ensuring that individual records cannot be distinguished while maintaining aggregate accuracy [88].
Homomorphic Encryption: Encryption techniques that allow computation on ciphertexts, generating encrypted results that, when decrypted, match the results of operations performed on the plaintext. This enables analysis of sensitive health data without decryption [88].
Blockchain for Data Integrity: Distributed ledger technology can create immutable audit trails for data access and usage, enhancing transparency and accountability in biomarker research data sharing [88].
The following workflow diagram illustrates a privacy-preserving data analysis pipeline for multi-site ML biomarker research:
Experimental Protocols for Ethical and Regulatory Compliance
Protocol: Multi-Site Data Sharing for Biomarker Discovery
Purpose: To establish a framework for secure and compliant sharing of health data across institutions for ML biomarker development while addressing ethical and regulatory requirements.
Materials and Reagents:
- De-identification Software: Tools such as ARX or Cornell Anonymization Toolkit for structured data de-identification
- Secure Transfer Platform: Encrypted file transfer solutions (e.g., SFTP, secure cloud storage)
- Data Use Agreements: Legally binding documents outlining permitted uses and protections
- Differential Privacy Tools: Libraries such as Google Differential Privacy or IBM Differential Privacy Library
Procedure:
- Regulatory Assessment Phase (Weeks 1-2):
- Identify all applicable regulations based on data source locations (HIPAA, GDPR, etc.)
- Determine the lawful basis for processing (consent, research exemption, etc.)
- Document compliance requirements for each jurisdiction
Data Preparation Phase (Weeks 3-6):
- Apply appropriate de-identification techniques based on regulatory requirements
- Implement data harmonization protocols to standardize formats across sites
- Create comprehensive data dictionaries and metadata documentation
Secure Transfer and Storage Phase (Weeks 7-8):
- Encrypt data using approved encryption standards (AES-256)
- Transfer via secure protocols with access logging
- Store in secured environments with access controls and audit trails
Validation Phase (Weeks 9-10):
- Verify de-identification effectiveness through re-identification risk assessment
- Confirm data utility for planned analyses
- Document all procedures for regulatory compliance
Validation Metrics:
- Re-identification risk score <0.1 using standardized risk assessment tools
- Data completeness >95% for critical variables
- Successful audit demonstrating compliance with all applicable regulations
Protocol: Bias Detection and Mitigation in ML Biomarkers
Purpose: To identify and address potential algorithmic bias in ML biomarker models across different demographic groups.
Materials and Reagents:
- Fairness Assessment Tools: Libraries such as AI Fairness 360, Fairlearn, or Aequitas
- Representative Datasets: Data encompassing diverse demographic groups
- Statistical Analysis Software: R, Python with appropriate fairness packages
Procedure:
- Bias Assessment Design (Week 1):
- Identify protected attributes for assessment (race, ethnicity, sex, age, socioeconomic status)
- Define fairness metrics appropriate for the clinical context (demographic parity, equalized odds, predictive parity)
- Establish acceptable fairness thresholds based on clinical impact
Model Performance Evaluation (Weeks 2-4):
- Evaluate model performance stratified by protected attributes
- Calculate fairness metrics across all subgroups
- Identify performance disparities exceeding established thresholds
Bias Mitigation Implementation (Weeks 5-8):
- Apply appropriate mitigation techniques (pre-processing, in-processing, or post-processing)
- Retrain models with fairness constraints where necessary
- Validate mitigated models on holdout datasets
Documentation and Reporting (Weeks 9-10):
- Document all detected biases and mitigation approaches
- Report final model performance across subgroups
- Include fairness assessment in model documentation for regulatory submissions
Validation Metrics:
- Performance difference <5% across demographic subgroups for key metrics (AUC, sensitivity, specificity)
- Fairness metrics within established thresholds for clinical context
- Successful external validation on independent datasets
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Resources for Ethical ML Biomarker Research
| Resource Category | Specific Tools/Solutions | Primary Function | Application Context |
|---|---|---|---|
| Data Privacy & Security | ARX De-identification Toolkit; IBM Security Guardium; Homomorphic Encryption Libraries (Microsoft SEAL) | Data protection; access control; encrypted computation | Multi-center research; sensitive health data analysis; regulatory compliance |
| Algorithmic Fairness | AI Fairness 360 (IBM); Fairlearn (Microsoft); Aequitas (University of Chicago) | Bias detection; fairness metrics; mitigation algorithms | Pre-deployment validation; regulatory documentation; equitable model development |
| Regulatory Compliance | FDA Digital Health Center of Excellence Resources; IMDRF Guidance Documents; Clinical Evaluation Templates | Regulatory pathway navigation; submission preparation; standards compliance | Premarket applications; quality management systems; international deployments |
| Multi-omics Integration | Biocrates AbsoluteIDQ p180 Kit; Targeted RNA-seq Platforms; Proteomic Profiling Kits | Metabolite quantification; gene expression analysis; protein biomarker measurement | Biomarker discovery; molecular signature validation; multi-analyte profiling |
| ML Model Development | Scikit-learn; TensorFlow; PyTorch; XGBoost | Model training; feature selection; performance evaluation | Predictive model development; biomarker validation; algorithm optimization |
| Explainable AI | SHAP; LIME; Captum; InterpretML | Model interpretation; feature importance; decision transparency | Regulatory submissions; clinical trust-building; model debugging |
The successful clinical adoption of ML-driven biomarkers requires careful attention to ethical, regulatory, and data privacy considerations throughout the research and development lifecycle. By implementing the frameworks, protocols, and tools outlined in this application note, researchers can navigate this complex landscape while maintaining scientific rigor and protecting patient rights. A proactive approach that integrates these considerations from the earliest stages of research design will accelerate the translation of promising ML biomarkers into clinically valuable tools that improve patient care and advance precision medicine. Future developments in regulatory science, privacy-preserving analytics, and fairness-aware machine learning will continue to shape this rapidly evolving field, requiring ongoing vigilance and adaptation from the research community.
Ensuring Robustness: Validation Frameworks and Technique Comparison
Best Practices for Rigorous Internal and External Validation
The application of machine learning (ML) to biomarker discovery represents a paradigm shift in precision medicine, enabling the identification of complex, multi-modal signatures from high-dimensional biological data. However, the translational potential of these discoveries is critically dependent on the rigor of validation strategies employed. A significant gap persists between the number of ML-discovered biomarkers and those successfully adopted in clinical practice, often due to inadequate validation and poor generalizability. This document outlines a comprehensive framework for internal and external validation, providing researchers and drug development professionals with actionable protocols to ensure that ML-derived biomarkers are robust, reliable, and ready for clinical integration.
Core Principles and Critical Challenges
Before detailing specific protocols, it is essential to understand the foundational principles and common pitfalls in ML-based biomarker validation.
- Principle 1: Rigor Over Novelty. Algorithmic complexity should not come at the cost of interpretability and validation robustness. Complex models like deep learning can exacerbate problems of overfitting without providing substantial performance gains in typical clinical datasets [89].
- Principle 2: Generalizability as a Goal. A model's performance is not proven until it is validated on data that was not used in any part of the training process, particularly from external cohorts and different clinical settings.
- Principle 3: Interpretability and Trust. For biomarkers to inform clinical decision-making, the rationale behind model predictions must be transparent. Explainable AI (XAI) techniques are thus integral to the validation workflow [53].
The most frequent challenges include small sample sizes, batch effects, data leakage during preprocessing, and insufficient external validation, all of which can lead to models that fail in real-world applications [89] [90].
Internal Validation Protocols
Internal validation assesses the stability and performance of an ML model using data derived from the same source population. Its goal is to provide an initial, unbiased estimate of model performance before proceeding to external testing.
Data Preparation and Partitioning
A critical first step is the rigorous partitioning of data to prevent data leakage, which artificially inflates performance metrics.
Table 1: Data Partitioning Strategies for Internal Validation
| Partitioning Strategy | Key Protocol | Best Use-Case Scenario |
|---|---|---|
| Train-Validation-Test Split | Randomly split data into training (~70%), validation (~15%), and a held-out test set (~15%). The test set is used only once for final evaluation. | Large datasets (n > 10,000) with homogeneous sources. |
| k-Fold Cross-Validation (CV) | Partition data into k equal folds. Iteratively use k-1 folds for training and the remaining fold for validation. Average performance across all k iterations. | Medium-sized datasets to maximize data use for training and validation. |
| Stratified k-Fold CV | Same as k-fold CV, but folds are made by preserving the percentage of samples for each class (for classification tasks). | Imbalanced datasets where the event of interest is rare. |
| Nested Cross-Validation | An outer loop for performance estimation (e.g., 5-fold) and an inner loop for hyperparameter tuning. This provides an almost unbiased estimate of the true performance. | Small to medium datasets where both hyperparameter tuning and robust performance estimation are needed. |
Experimental Protocol:
- Preprocessing: Conduct feature scaling and normalization. Critical: All parameters for these transformations (e.g., mean, standard deviation) must be derived only from the training set and then applied to the validation and test sets.
- Partitioning: Apply a stratified split based on the outcome variable to maintain class distribution across sets.
- Handling Missing Data: Impute missing values (e.g., with mean/median) using parameters from the training set only.
Model Training and Tuning
Experimental Protocol:
- Algorithm Selection: Begin with simpler, more interpretable models (e.g., Logistic Regression, Random Forest) as baselines before progressing to complex ensembles or deep learning [89] [53].
- Hyperparameter Optimization: Use the validation set (or inner CV loop in nested CV) to tune hyperparameters. Common methods include Grid Search or Random Search.
- Performance Benchmarking: Evaluate the tuned model on the held-out test set. The performance on this set serves as the primary internal validation metric.
Performance Metrics and Interpretation
Table 2: Key Performance Metrics for Internal Validation
| Metric | Formula/Description | Interpretation |
|---|---|---|
| Area Under the Curve (AUC) | Plots True Positive Rate vs. False Positive Rate across thresholds. | Measures overall discriminative ability. AUC > 0.9 is considered excellent. |
| Accuracy | (TP + TN) / (TP + TN + FP + FN) | Proportion of total correct predictions. Can be misleading for imbalanced data. |
| Precision | TP / (TP + FP) | Of all predicted positives, how many are true positives. |
| Recall (Sensitivity) | TP / (TP + FN) | Of all actual positives, how many are correctly identified. |
| F1-Score | 2 * (Precision * Recall) / (Precision + Recall) | Harmonic mean of precision and recall. Useful for imbalanced datasets. |
| Mean Absolute Error (MAE) | Mean of absolute differences between predicted and actual values. | For regression tasks (e.g., Biological Age prediction). Lower is better [53]. |
External Validation Protocols
External validation is the definitive test of a model's generalizability and clinical utility, evaluating its performance on data collected from different populations, sites, or under different protocols.
Types of External Validation
- Temporal Validation: Applying the model to new data collected from the same institution but at a later time.
- Geographical Validation: Using data from a different location or country.
- Domain Validation: Testing the model on data from a different type of clinical setting (e.g., primary care vs. tertiary hospital).
Experimental Protocol:
- Cohort Acquisition: Secure one or more fully independent external validation cohorts. The study protocol for this validation should be pre-registered.
- Model Application: Apply the fully locked model—including the final algorithm, features, and all preprocessing parameters saved from the training phase—to the new external data. No retraining or recalibration should be done at this stage.
- Performance Assessment: Calculate the same performance metrics used in internal validation. A significant drop in performance (e.g., AUC decrease > 0.1) indicates poor generalizability.
Analysis of Model Generalizability and Robustness
Experimental Protocol:
- Subgroup Analysis: Evaluate model performance across key demographic and clinical subgroups (e.g., by sex, ethnicity, disease severity, comorbidities) to identify performance disparities [90].
- Stability Analysis: Assess the impact of batch effects or different processing protocols on the model's predictions.
- Calibration Assessment: Use calibration plots to check if the predicted probabilities of an outcome match the observed frequencies. A well-calibrated model is essential for clinical risk stratification.
The Explainable AI (XAI) Protocol for Biomarker Interpretation
Validation is not complete without understanding why a model makes its predictions. XAI is crucial for biomarker discovery and building clinical trust [53].
Experimental Protocol:
- Model-Agnostic Interpretation: Employ techniques like SHapley Additive exPlanations (SHAP) to quantify the contribution of each feature to individual predictions [53].
- Global Feature Importance: Use SHAP summary plots or permutation feature importance to identify the top biomarkers driving the model's overall predictions.
- Biological Plausibility: Interpret the results in the context of known biological pathways. The identification of cystatin C as a primary contributor in both biological age and frailty models, for instance, strengthens the biological credibility of the ML framework [53].
The following diagram illustrates the integrated workflow, from data preparation to clinical translation, incorporating the core validation and XAI steps detailed in the protocols.
Diagram Title: ML Biomarker Validation and Translation Workflow
This section details key reagents, software, and data resources required to implement the described validation protocols.
Table 3: Research Reagent Solutions for Biomarker Validation
| Category / Item | Function and Role in Validation | Example Tools / Sources |
|---|---|---|
| Biobanked Cohorts | Provides clinically annotated samples for discovery and internal validation. Essential for initial model building. | CHARLS [53], UK Biobank, The Cancer Genome Atlas (TCGA). |
| Independent Validation Cohorts | Serves as the gold standard for external validation to test model generalizability. | Disease-specific consortia, multi-center trial data, public repositories (e.g., GEO, PRIDE). |
| High-Throughput Assays | Generate the multi-omics data used as features for ML models. | Mass Spectrometry (Proteomics) [89], RNA-seq (Transcriptomics) [11], LC–MS/MS (Metabolomics) [90]. |
| ML & Statistical Software | Platforms for implementing data preprocessing, model training, and validation protocols. | Python (scikit-learn, XGBoost, CatBoost [53]), R (caret, mlr). |
| Explainable AI (XAI) Libraries | Tools for interpreting ML models and identifying key biomarker contributors. | SHAP [53], LIME, ELI5. |
| Automated Testing Suites | Software for continuous monitoring of model performance and data integrity in deployed settings. | AllAccessible (for compliance) [91], custom monitoring dashboards. |
The path from a computationally discovered biomarker to a clinically actionable tool is fraught with challenges that can only be overcome through meticulous and rigorous validation. By adhering to the structured protocols for internal and external validation outlined herein—and by integrating explainable AI to ensure interpretability—researchers can significantly enhance the reliability, generalizability, and ultimately, the translational success of their machine learning models in biomarker discovery.
Evaluating Predictive Performance and Clinical Utility via AUC and Other Metrics
In machine learning (ML)-driven biomarker discovery, a rigorous evaluation of a model's predictive performance is paramount before assessing its potential for clinical adoption. A biomarker's value in precision medicine is determined by its ability to reliably indicate a biological process, pathological state, or response to a therapeutic intervention [11]. The evaluation process moves from establishing generic predictive performance using statistical metrics to demonstrating clinical utility, which is the measure of whether using the biomarker actually improves patient outcomes [92].
This document outlines a standardized protocol for this critical evaluation process. We begin with the foundational statistical metrics, most notably the Area Under the Receiver Operating Characteristic Curve (AUC), and then advance to more nuanced measures of clinical impact, such as reclassification. This phased approach ensures that only biomarkers with robust predictive performance graduate to costly and complex clinical impact studies [92].
Quantitative Interpretation of Predictive Performance
The ROC Curve and AUC Metric
The Receiver Operating Characteristic (ROC) curve is a fundamental tool for evaluating the performance of a binary classifier across all possible classification thresholds [93] [94]. It graphically represents the trade-off between the True Positive Rate (TPR), or sensitivity, and the False Positive Rate (FPR), which is 1-specificity [93] [95] [94].
The Area Under the ROC Curve (AUC) is a single numerical value that summarizes the curve's information. The AUC represents the probability that the model will rank a randomly chosen positive instance higher than a randomly chosen negative instance [93] [95]. Its value ranges from 0.5 to 1.0:
- AUC = 0.5: Indicates a model with no discriminative ability, equivalent to random guessing. The ROC curve is a diagonal line.
- AUC = 1.0: Indicates a perfect model with perfect discrimination at some threshold. The ROC curve reaches the top-left corner [93] [95] [94].
Table 1: Standard Interpretations of AUC Values for Diagnostic Tests [95]
| AUC Value | Interpretation Suggestion |
|---|---|
| 0.9 ≤ AUC | Excellent |
| 0.8 ≤ AUC < 0.9 | Considerable |
| 0.7 ≤ AUC < 0.8 | Fair |
| 0.6 ≤ AUC < 0.7 | Poor |
| 0.5 ≤ AUC < 0.6 | Fail |
In practice, an AUC above 0.8 is generally considered clinically useful, while values below 0.8 indicate limited clinical utility, even if they are statistically significant [95]. For instance, a study predicting cognitive metrics in "SuperAgers" using blood biomarkers reported a predictive model accuracy of 76%, which typically corresponds to an AUC value in the "fair" to "considerable" range [96].
Limitations of the AUC
While the AUC is a valuable general-purpose metric, it has significant limitations:
- Insensitivity to Improvement: The AUC is an insensitive measure for evaluating the incremental value of a new biomarker added to an existing model. Even a biomarker with a strong independent association with the disease may only marginally improve the AUC [97].
- Dependence on Balance: AUC and ROC curves work well for comparing models when the dataset is roughly balanced between classes. For imbalanced datasets, precision-recall curves may offer a better comparative visualization [93].
- Abstract Interpretation: The AUC does not directly translate to clinical consequences. A high AUC does not, by itself, guarantee that a biomarker will improve clinical decision-making or patient health [92] [97].
Advanced Metrics for Clinical Utility
Risk Reclassification and the Net Reclassification Improvement (NRI)
To address the limitations of the AUC, the paradigm of risk reclassification was developed. This method is used when clinical risk strata (e.g., low, intermediate, high) guide treatment decisions [97].
The process involves:
- Defining clinically meaningful risk categories.
- Classifying patients into these categories using a baseline model (e.g., with established risk factors).
- Reclassifying the same patients using a new model that includes the novel biomarker.
- Analyzing the net movement of patients, particularly cases (those who experience the event) and controls (those who do not), across categories.
The Net Reclassification Improvement (NRI) quantifies this improvement. It is calculated as the sum of the net proportion of cases correctly moving up to a higher risk category and the net proportion of controls correctly moving down to a lower risk category [97].
NRI = (Proportion of cases moving up - Proportion of cases moving down) + (Proportion of controls moving down - Proportion of controls moving up)
A positive NRI indicates that the new model improves classification accuracy. For example, adding systolic blood pressure to a cardiovascular risk model resulted in a significant NRI, demonstrating its value even though the AUC increase was minimal [97].
Table 2: Comparison of Key Biomarker Evaluation Metrics
| Metric | Measures | Key Strength | Key Limitation |
|---|---|---|---|
| AUC | Overall model discrimination across all thresholds. | Intuitive summary of performance; threshold-independent. | Insensitive to incremental value; does not reflect clinical utility directly. |
| Net Reclassification Improvement (NRI) | Improvement in classification into clinically relevant risk strata. | Directly tied to clinical decision-making; more sensitive than AUC. | Requires pre-defined, meaningful risk categories. |
| Reclassification Calibration (RC) | Agreement between predicted and observed risk after reclassification. | Assesses the calibration (accuracy) of the new risk estimates. | Requires a large sample size for stable estimates. |
Experimental Protocols for Evaluation
Protocol 1: ROC Analysis and AUC Calculation for a Novel Biomarker
Objective: To evaluate the diagnostic discrimination of a novel blood-based DNA methylation biomarker for early breast cancer detection [98].
Materials:
- Research Reagent Solutions:
- Patient Samples: Plasma samples from a cohort of confirmed breast cancer patients (cases) and healthy controls.
- DNA Extraction Kit: For isolating cell-free DNA (cfDNA) from plasma.
- Bisulfite Conversion Kit: To treat DNA for methylation analysis (e.g., EZ DNA Methylation-Lightning Kit).
- Quantitative Methylation-Specific PCR (qMSP) Assay: Primers and probes specific to the methylated sequence of the target biomarker.
- Real-Time PCR System: Instrument to run qMSP assays (e.g., Applied Biosystems 7500).
- Statistical Software: R or Python with
pROC,scikit-learnpackages.
Procedure:
- Sample Preparation: Isolate cfDNA from all plasma samples.
- Bisulfite Conversion: Treat all isolated cfDNA with bisulfite, converting unmethylated cytosine to uracil while leaving methylated cytosine unchanged.
- Target Amplification: Perform qMSP on the bisulfite-converted DNA for the target biomarker. The cycle threshold (Ct) value will be used to calculate the methylation level.
- Data Collection: For each sample, obtain a continuous numerical value representing the level of methylation (e.g., normalized methylation ratio).
- ROC Analysis: a. Using statistical software, input the continuous methylation values and the true class labels (case vs. control). b. Generate the ROC curve by plotting the TPR against the FPR at every possible threshold for the methylation value. c. Calculate the AUC, often using the trapezoidal rule [94].
- Interpretation: Compare the calculated AUC to standard benchmarks (Table 1). An AUC > 0.8 suggests considerable diagnostic potential warranting further study [95].
Protocol 2: Assessing Clinical Utility via Reclassification Analysis
Objective: To determine if a novel predictive biomarker (e.g., LCK or ERK1, as identified by ML [27]) improves risk stratification for therapy response in oncology over a standard model.
Materials:
- Clinical Cohort Data: A dataset of cancer patients with recorded outcomes (responders vs. non-responders to a targeted therapy), standard clinical variables (e.g., TNM stage, age), and measurements of the novel biomarker.
- Statistical Software: R or Python with packages for logistic regression and NRI calculation (e.g., R
nricenspackage).
Procedure:
- Define Risk Strata: Establish clinically relevant risk categories for non-response (e.g., Low: <20%, Intermediate: 20-50%, High: >50% probability).
- Develop Baseline Model: Build a multivariable logistic regression model predicting non-response using only standard clinical variables.
- Calculate Baseline Risk: Use this model to calculate each patient's predicted probability of non-response and classify them into the risk strata.
- Develop Enhanced Model: Build a second logistic regression model that includes all standard variables plus the novel biomarker.
- Calculate Enhanced Risk: Use the enhanced model to calculate new probabilities and reclassify patients.
- Construct Reclassification Table: Create a contingency table comparing the risk strata from the baseline and enhanced models.
- Calculate NRI: a. Among the non-responders (cases), calculate the proportion who moved to a higher risk category minus the proportion who moved to a lower risk category. b. Among the responders (controls), calculate the proportion who moved to a lower risk category minus the proportion who moved to a higher risk category. c. Sum these two values to get the NRI. Test its statistical significance.
- Assess Calibration: Calculate the Reclassification Calibration (RC) statistic to evaluate if the predicted risks from the new model align with observed outcomes [97].
Visualizing the Evaluation Workflow
The following diagram illustrates the logical pathway from biomarker discovery to the assessment of clinical utility, integrating the metrics and protocols described above.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Biomarker Evaluation
| Reagent / Material | Function in Evaluation | Example Applications |
|---|---|---|
| Liquid Biopsy Collection Tubes | Stabilizes blood samples for plasma and cfDNA isolation. | Early cancer detection from ctDNA [98]. |
| Cell-free DNA Extraction Kits | Isolves circulating, tumor-derived DNA from plasma. | Enabling methylation analysis of ctDNA [98]. |
| Bisulfite Conversion Kits | Treats DNA to distinguish methylated from unmethylated cytosines. | Fundamental step for most DNA methylation analyses [98]. |
| Droplet Digital PCR (ddPCR) | Provides absolute quantification of target molecules with high sensitivity. | Validating and detecting rare methylation events in ctDNA [98]. |
| Next-Generation Sequencing (NGS) | Allows for high-throughput, genome-wide profiling of biomarkers. | Comprehensive methylation sequencing (e.g., WGBS, RRBS) [98]. |
| Validated Antibody Panels | Enables protein-level quantification via immunoassays or flow cytometry. | Measuring protein biomarkers in blood or tissue samples. |
| Statistical Software (R, Python) | Performs ROC analysis, calculates AUC, NRI, and other advanced metrics. | Essential for all statistical evaluation of predictive performance [11] [97]. |
Assessing Biomarker Stability and Reproducibility Across Cohorts
Biomarkers have revolutionized research and clinical practice for neurodegenerative diseases and beyond, transforming drug trial design and enhancing patient management [99]. However, the field grapples with a significant challenge: many biomarker findings, despite initially promising results, demonstrate low reproducibility in subsequent studies [99]. This irreproducibility wastes valuable research resources and hampers the translation of discoveries into clinical tools [99]. The problem is multifaceted, stemming from cohort-related biases, pre-analytical and analytical variability, and insufficient statistical approaches [99]. Furthermore, the integration of machine learning (ML) into biomarker discovery, while powerful, introduces new pitfalls—such as overfitting and data leakage—that can further compromise reproducibility if not meticulously managed [89] [100]. This application note provides a detailed framework for assessing biomarker stability and reproducibility, a critical component for advancing reliable, ML-driven biomarker research.
Foundational Pillars of Biomarker Reproducibility
A reproducible biomarker study is built upon three core pillars: robust cohort design, stringent control of pre-analytical and analytical variables, and rigorous statistical validation. The table below summarizes key challenges and mitigation strategies.
Table 1: Key Challenges and Mitigations for Biomarker Reproducibility
| Domain | Challenge | Proposed Mitigation Strategy |
|---|---|---|
| Cohort Design | Small sample sizes leading to overestimated effects [99] | Prioritize large, prospectively recruited cohorts; pre-register study designs [99]. |
| Recruitment bias (e.g., "super-healthy" controls) [99] | Recruit consecutively; ensure patient and control groups are matched and recruited from the same centers [99]. | |
| Confounding factors (e.g., age, co-morbidities, medication) [99] | Record and statistically adjust for known confounders [99]. | |
| Pre-Analytical & Analytical Factors | Poor assay specificity and selectivity [99] | Validate assays for cross-reactivity and perform spike-recovery experiments [99]. |
| Lot-to-lot variability of analytical kits [99] | Perform batch-bridging experiments; use a single kit lot for a single study where possible [99]. | |
| Sample handling variability (e.g., centrifugation, storage) [99] | Implement and adhere to standardized operating procedures (SOPs) for all steps [99]. | |
| Statistical & ML Modeling | Overfitting in high-dimensional data (p >> n problem) [100] | Use simple, interpretable models; apply strong regularization and feature selection [89] [100]. |
| Data leakage and optimistic performance estimates [100] | Employ strict separation of training, validation, and test sets; use nested cross-validation [100]. | |
| Lack of model interpretability ("black box" models) [11] | Utilize explainable AI (XAI) techniques, such as SHAP, to interpret feature contributions [11]. |
Experimental Protocol: Assessing Pre-Analytical Sample Stability
Aim: To determine the stability of a candidate biomarker under varying pre-analytical conditions. Materials:
- Freshly collected bio-samples (e.g., plasma, serum, CSF) from a minimum of 5 healthy donors.
- Standard collection tubes (e.g., EDTA, serum separator).
- Refrigerated centrifuge.
- -80°C freezer.
- Validated assay for biomarker quantification (e.g., ELISA, mass spectrometry).
Procedure:
- Sample Collection: Collect venous blood or CSF using a standardized protocol. Pool samples if necessary to ensure sufficient volume.
- Time Delay Experiment: Aliquot samples and process them at different time intervals (e.g., 0, 1, 2, 4, 8, 24 hours) post-collection. Hold samples at room temperature during the delay.
- Freeze-Thaw Cycle Experiment: Aliquot processed samples (e.g., plasma). Subject aliquots to multiple freeze-thaw cycles (e.g., 1, 2, 3, 5 cycles). For each cycle, freeze at -80°C for at least 12 hours, then thaw completely on ice or in a refrigerator.
- Storage Temperature Experiment: Aliquot processed samples and store them at different temperatures (e.g., 4°C, -20°C, -80°C). Analyze aliquots at predefined time points (e.g., 1 week, 1 month, 3 months, 1 year).
- Analysis: Quantify the biomarker level in all aliquots using the validated assay in a single batch to minimize analytical variance.
- Data Analysis: Calculate the mean concentration and coefficient of variation (CV) for each condition. A change of less than 10-15% from the baseline (time 0, single freeze-thaw) is often considered acceptable for stability.
Workflow for Reproducibility Assessment
The following diagram outlines a logical workflow for a comprehensive biomarker reproducibility assessment, integrating both traditional and machine-learning approaches.
The Machine Learning Pipeline for Reproducible Biomarker Discovery
Machine learning offers powerful tools for identifying complex, multi-analyte biomarker signatures from high-dimensional omics data [11]. However, this power comes with a heightened risk of irreproducibility if the pipeline is not carefully constructed [89].
Experimental Protocol: A Rigorous ML Cross-Validation Scheme
Aim: To train and validate a biomarker model without data leakage, ensuring a realistic estimate of its performance on unseen data. Materials:
- A dataset with samples (n) and features (p), where p can be much larger than n (p >> n).
- Computing environment (e.g., Python with scikit-learn, R).
- Research Reagent Solutions: Table 2 lists key computational "reagents" for this protocol.
Table 2: Research Reagent Solutions for ML Biomarker Discovery
| Reagent / Tool | Function / Explanation | Example |
|---|---|---|
| Feature Selection Algorithm | Reduces high-dimensional data to the most informative features, mitigating overfitting. | LASSO regression, Recursive Feature Elimination (RFECV) [16] [100]. |
| Cross-Validation Scheduler | Manages the splitting of data into training and validation sets to tune model parameters. | RepeatedStratifiedKFold from scikit-learn. |
| Machine Learning Algorithms | The models that learn the relationship between features and the outcome. | Logistic Regression, Random Forest, Support Vector Machines [11] [16]. |
| Interpretability Package | Explains model predictions, building trust and biological insight. | SHAP (SHapley Additive exPlanations) [101]. |
| Independent Test Set | A hold-out set of data, completely untouched during model training, used for the final performance assessment. | A cohort from a different clinical site or a temporally distinct collection [100]. |
Procedure (Nested Cross-Validation):
- Data Partitioning: Hold back a portion of the full dataset (e.g., 20-30%) as a final external test set. This set must never be used for feature selection or model tuning.
- Outer Loop (Performance Estimation): Split the remaining data (the training pool) into k-folds (e.g., k=5 or 10). For each fold: a. Hold out one fold as the validation set. b. Use the remaining k-1 folds for the inner loop.
- Inner Loop (Model Selection & Tuning): On the k-1 folds from step 2b, perform another cross-validation to select the best model parameters and features. This is where you would apply feature selection methods like RFECV [16]. a. Train the model with the selected features and parameters on the k-1 folds. b. Evaluate the trained model on the validation fold from step 2a. Store the performance metric.
- Final Model Training: After looping through all outer folds, train a final model on the entire training pool (excluding the external test set), using the optimal parameters and features identified from the nested process.
- Final Evaluation: Apply the final model to the external test set from step 1 to obtain an unbiased estimate of its real-world performance. Report metrics like AUC, accuracy, precision, and recall [16] [102].
Workflow for ML-Specific Reproducibility
The diagram below details the critical steps within a machine learning pipeline that are essential for ensuring the resulting biomarker signature is reproducible and generalizable.
Achieving reproducible biomarkers across cohorts is a demanding but attainable goal. It requires a holistic strategy that marries rigorous traditional laboratory practices—meticulous cohort design, pre-analytical standardization, and analytical validation—with a modern, disciplined approach to machine learning. The protocols and frameworks outlined here provide a concrete path forward. By adopting these practices, researchers can enhance the reliability of their biomarker discoveries, accelerate their translation into clinical tools, and ultimately strengthen the foundation of precision medicine.
Comparative Analysis of Feature Selection Methods and Resulting Biomarker Signatures
The advent of high-throughput molecular profiling technologies has generated vast, complex omics datasets, presenting a dimensionality reduction challenge for biomarker discovery in precision medicine [11] [103]. Feature selection methodologies represent a critical computational solution to this problem by identifying optimal subsets of molecular features that are most relevant for distinguishing disease states, predicting treatment responses, and understanding biological mechanisms [104]. Unlike feature extraction methods that transform original features into new representations, feature selection preserves the biological interpretability of selected biomarkers, making it particularly valuable for generating clinically actionable gene signatures [104].
The integration of machine learning (ML) with multi-omics data represents a paradigm shift from traditional single-marker approaches, enabling the identification of complex molecular signatures that more accurately capture disease heterogeneity [11] [9]. This application note provides a structured comparative analysis of feature selection methodologies, detailed experimental protocols, and practical visualization tools to guide researchers in selecting appropriate strategies for biomarker discovery projects within drug development and clinical diagnostics.
Biomarker Types and Machine Learning Applications in Precision Medicine
Biomarkers serve as measurable indicators of biological processes, pathological states, or responses to therapeutic interventions, playing critical roles in disease diagnosis, prognosis, and personalized treatment strategies [11]. In precision medicine, biomarkers can be categorized into several functional types:
- Diagnostic biomarkers identify the presence or type of a disease
- Prognostic biomarkers forecast disease progression or recurrence
- Predictive biomarkers estimate responses to specific therapeutic interventions
- Pharmacodynamic biomarkers monitor biological responses to treatment [11]
Machine learning approaches have demonstrated significant utility across diverse disease domains, including oncology (breast, lung, colon cancers), infectious diseases (COVID-19, tuberculosis), neurological disorders (Alzheimer's, schizophrenia), and autoimmune conditions [11] [9]. ML enables disease endotyping—classifying subtypes based on shared molecular mechanisms rather than purely clinical symptoms—thereby supporting more precise patient stratification and therapy selection [11].
Table 1: Machine Learning Applications Across Disease Domains
| Disease Domain | ML Application Examples | Data Types Utilized |
|---|---|---|
| Oncology | Early detection, tumor subtyping, immunotherapy response prediction | Genomics, transcriptomics, epigenomics, histopathology [11] |
| Infectious Diseases | Distinguishing viral vs. bacterial infections, predicting disease severity | Host and microbial biomarkers, metagenomics [11] |
| Neurological Disorders | Identifying biomarkers for depression, schizophrenia, Alzheimer's | Structural and functional neuroimaging, CSF biomarkers [11] [9] |
| Cardiovascular Diseases | Predicting large-artery atherosclerosis, plaque progression | Clinical factors, metabolites, imaging data [16] |
Feature Selection Methodologies: A Comparative Analysis
Feature selection algorithms can be broadly categorized into filter, wrapper, and embedded methods, each with distinct mechanisms for evaluating feature subsets [104]. The supervised feature selection approaches leverage class labels to identify the most discriminative features, while unsupervised methods discover inherent structures in unlabeled data [104].
Key Feature Selection Algorithms
Recent comparative studies have evaluated multiple feature selection algorithms across various omics data types. The following table summarizes five widely used supervised feature selection methods and their performance characteristics:
Table 2: Comparative Analysis of Feature Selection Algorithms
| Algorithm | Mechanism | Strengths | Limitations | Optimal Use Cases |
|---|---|---|---|---|
| mRMR (Minimal Redundancy Maximal Relevance) | Selects features that have high relevance to target and low redundancy between features [104] | Maintains feature diversity, strong theoretical foundation | May overlook complementary features | Initial filtering of high-dimensional data [104] |
| INMIFS (Improved Normalized Mutual Information Feature Selection) | Uses normalized mutual information to balance relevance and redundancy [104] | Improved normalization compared to earlier MIFS variants | Parameter sensitivity | Data with known feature interactions |
| DFS (Discriminative Feature Selection) | Emphasizes class separation capability in feature evaluation [104] | Strong focus on discriminative power | May select correlated features if all are discriminative | Classification tasks with clear class boundaries |
| SVM-RFE-CBR (SVM Recursive Feature Elimination with Correlation Bias Reduction) | Recursively removes features with smallest weights from SVM while reducing correlation bias [104] | Handles non-linear relationships, reduces bias | Computationally intensive for very high dimensions | Small to medium datasets with complex patterns |
| VWMRmR (Variable Weighted Maximal Relevance minimal Redundancy) | Uses variable weighting in mutual information calculations [104] | Best overall performance in multi-omics study, optimal balance of accuracy and redundancy reduction [104] | Algorithmic complexity | Multi-omics data integration projects |
Performance Metrics and Evaluation
The evaluation of feature selection methods typically employs multiple criteria to assess different aspects of performance:
- Classification Accuracy (Acc): Measures predictive performance using classifiers like C4.5, NaiveBayes, KNN, and AdaBoost [104]
- Redundancy Rate (RR): Quantifies feature overlap using normalized mutual information or Pearson correlation coefficient [104]
- Representation Entropy (RE): Assesses the informational content of selected feature subsets [104]
In a comprehensive benchmark study across five omics datasets (gene expression, exon expression, DNA methylation, copy number variation, and pathway activity), the VWMRmR algorithm demonstrated superior performance, achieving the best classification accuracy for three datasets (ExpExon, hMethyl27, and Paradigm IPLs), the best redundancy rate for three datasets, and the best representation entropy for three datasets [104].
Integrated Experimental Protocols for Biomarker Discovery
This section provides detailed methodologies for implementing feature selection in biomarker discovery workflows, incorporating best practices for experimental validation.
Data Preprocessing and Preparation
Protocol 1: Data Cleaning and Normalization
- Input Data Requirements: Table-like structure with samples in rows and features in columns; field separators (tab, comma, semicolon) automatically detected [103]
- Missing Value Imputation: Apply mean imputation for each variable using specialized packages in R or Python [16]
- Data Integration: Merge multiple input files (e.g., clinico-pathological with omics data) using sample identifiers as keys [103]
- Train-Test Splitting: Separate data into training (2/3) and test (1/3) sets to assess non-overfitting; maintain class distribution balance [103]
Protocol 2: Handling High-Dimensional Data Challenges
- Feature Ranking: Apply initial filter to sort features by predictive power using univariate statistical tests [103]
- Dimensionality Reduction: Retain top 1,000 features by default to manage computational complexity while preserving signal [103]
- Cross-Validation Framework: Implement nested cross-validation to avoid overfitting during model selection [105]
Feature Selection Implementation
Protocol 3: Hybrid Sequential Feature Selection
Based on successful application in Usher syndrome biomarker discovery [105]:
- Step 1: Initial filtering using variance thresholding to remove low-variance features
- Step 2: Apply recursive feature elimination to rank features by importance
- Step 3: Implement Lasso regression for further feature refinement
- Step 4: Integrate within nested cross-validation framework for robust selection
- Step 5: Validate selected features using multiple ML models (Logistic Regression, Random Forest, SVM)
Protocol 4: Recursive Feature Elimination with Cross-Validation (RFECV)
As applied in large-artery atherosclerosis biomarker discovery [16]:
- Step 1: Train initial model on all features
- Step 2: Recursively eliminate least important features
- Step 3: Evaluate performance at each step using cross-validation
- Step 4: Select feature subset with optimal cross-validation performance
- Step 5: Validate on held-out test set
Model Validation and Biological Confirmation
Protocol 5: Multi-Model Validation Framework
- Classifier Diversity: Employ multiple algorithm types (LR, SVM, RF, XGBoost) with different inductive biases [16]
- Performance Metrics: Evaluate using AUC-ROC, accuracy, precision, recall, and F1-score [16]
- Shared Feature Analysis: Identify features consistently selected across different models as high-confidence candidates [16]
Protocol 6: Experimental Validation of Computational Predictions
- ddPCR Validation: Confirm expression patterns of top candidate mRNA biomarkers using droplet digital PCR [105]
- Pathway Analysis: Interpret selected biomarkers in context of biological pathways (e.g., aminoacyl-tRNA biosynthesis, lipid metabolism) [16]
- Clinical Correlation: Associate biomarker signatures with clinical outcomes and patient stratification [11]
Visualization of Experimental Workflows and Computational Pipelines
Biomarker Discovery Workflow
Algorithm Performance Comparison
Table 3: Research Reagent Solutions for Biomarker Discovery
| Resource Category | Specific Tools & Platforms | Function & Application |
|---|---|---|
| Omics Profiling Technologies | Absolute IDQ p180 Kit (Biocrates) | Quantifies 194 endogenous metabolites from 5 compound classes for metabolomics [16] |
| Data Generation Platforms | DNA microarrays, RNA sequencing, mass spectrometry, whole exome/genome sequencing | Generate high-dimensional molecular profiling data [103] |
| Automated Machine Learning Tools | BioDiscML | Stand-alone program for biomarker signature identification; automates preprocessing, feature selection, model selection [103] |
| Programming Libraries & Frameworks | Weka, scikit-learn, Pandas, NumPy | Provide machine learning algorithms, data manipulation, and statistical analysis capabilities [103] [16] |
| Experimental Validation Tools | Droplet digital PCR (ddPCR) | Validates expression patterns of computationally identified mRNA biomarkers [105] |
The comparative analysis presented in this application note demonstrates that feature selection methodology choice significantly impacts the performance and interpretability of resulting biomarker signatures. Among the algorithms evaluated, VWMRmR achieved superior performance across multiple omics datasets and evaluation criteria, providing an optimal balance between classification accuracy, redundancy reduction, and representation entropy [104].
The integration of hybrid sequential feature selection approaches with rigorous validation frameworks has proven effective across diverse disease contexts, from Usher syndrome to large-artery atherosclerosis [105] [16]. The consistent finding that shared features across multiple models exhibit strong predictive power highlights the importance of multi-algorithm validation in identifying robust biomarker signatures [16].
Future directions in feature selection for biomarker discovery will likely focus on multi-omics data integration, with ML approaches simultaneously analyzing genomics, transcriptomics, proteomics, metabolomics, and clinical data to identify complex biomarker patterns [11]. Additionally, the development of explainable AI techniques will be crucial for enhancing model interpretability and facilitating clinical adoption [11] [9]. As these methodologies mature, they will increasingly enable the transition from traditional disease classification to mechanistic endotyping, ultimately supporting more precise and personalized therapeutic interventions [11].
The integration of machine learning (ML) into biomarker discovery represents a paradigm shift in precision medicine, offering the potential to decipher complex, multi-omics datasets for improved disease diagnosis, prognosis, and treatment selection [11]. However, the journey from a promising computational model to a clinically validated tool approved by regulatory bodies like the U.S. Food and Drug Administration (FDA) is arduous [106]. The foundational element of this journey is a robust, transparent, and statistically sound benchmarking process that moves beyond mere algorithmic performance to demonstrate real-world clinical utility and safety [89] [107]. This document outlines application notes and detailed protocols for benchmarking ML models, framed within the critical pathway from research to regulatory approval and clinical implementation.
Unrealistic expectations and methodological pitfalls currently limit the real-world impact of ML in clinical proteomics and biomarker discovery [89]. A significant challenge is the uncritical application of complex models, such as deep learning architectures, which often exacerbates problems of overfitting, reduces interpretability, and offers negligible performance gains on typical clinical datasets with limited sample sizes [89]. Consequently, a cultural shift is necessary—one that prioritizes methodological rigor, transparency, and domain awareness over hype-driven complexity [89] [108]. The following sections provide a structured approach to achieve this rigor, ensuring that ML-derived biomarkers can withstand regulatory scrutiny and improve patient outcomes.
Regulatory and Clinical Framework
The Evolving Regulatory Landscape for AI/ML Biomarkers
Regulatory frameworks for AI/ML-based medical devices and biomarkers are evolving rapidly. The FDA, Health Canada, and the UK's MHRA have jointly proposed ten guiding principles for Good Machine Learning Practice (GMLP) [108]. These principles provide a foundational framework for the entire product life cycle, from development to deployment and monitoring. Concurrently, there is significant legislative activity at the state level, particularly regarding biomarker testing coverage mandates, which often focus on clinical utility and are initially centered on areas like oncology and Alzheimer's disease [109].
Table 1: Key Regulatory Principles and Their Implications for Benchmarking
| Regulatory Principle | Description | Benchmarking Implication |
|---|---|---|
| Multi-Disciplinary Expertise [108] | Leverage diverse expertise throughout the total product life cycle. | Benchmarking teams must include clinicians, statisticians, and data scientists. |
| Representative Training Data [108] | Clinical study participants and datasets must represent the intended patient population. | Benchmarking must include fairness and bias assessments across subpopulations. |
| Independent Training & Test Sets [108] | Training datasets must be independent of test sets. | Rigorous protocols to prevent data leakage are mandatory. |
| Human-AI Team Performance [108] | Focus on the performance of the human-AI team. | Benchmarking should evaluate the model's utility in the clinical workflow, not just its standalone accuracy. |
| Clear User Information [108] | Users must be provided with clear, essential information. | Models must be interpretable, and performance metrics must be communicable to clinicians. |
| Deployment Monitoring [108] | Deployed models must be monitored for performance and re-training risks managed. | Benchmarking should establish baselines for ongoing performance monitoring post-deployment. |
The role of biomarkers in regulatory decision-making has expanded significantly, with prominent applications as surrogate endpoints, confirmatory evidence, and for dose selection in clinical trials [106]. For example, in neurology, biomarkers like neurofilament light chain (NfL) in Amyotrophic Lateral Sclerosis (ALS) and amyloid beta in Alzheimer's Disease have been used as surrogate endpoints for accelerated approval [106]. Benchmarking ML models that identify such biomarkers must therefore be designed to meet the high evidence standards required for these specific regulatory roles.
Defining Clinical Utility and Intended Use
A biomarker's intended use (e.g., risk stratification, diagnosis, prognosis, or prediction of treatment response) must be defined early in the development process, as this dictates the target population, specimen type, and the statistical validation strategy [13]. Prognostic biomarkers (forecasting disease progression) can be identified through retrospective studies, while predictive biomarkers (estimating treatment efficacy) typically require data from randomized clinical trials and an interaction test between treatment and biomarker [13].
Benchmarking Protocols and Experimental Design
Foundational Principles for Method Comparison
Robust benchmarking in ML for drug discovery lies at the intersection of multiple scientific disciplines and requires statistically rigorous protocols and domain-appropriate performance metrics to ensure replicability [107]. The core challenge is to determine whether a higher metric score signifies a genuinely better model or is merely an artifact of statistical bias or flawed metric design [110].
- Null Hypothesis and Statistical Testing: Employ statistical tests like null hypothesis testing to determine if performance differences between models are statistically significant rather than random noise [110]. For multiple model comparisons, techniques like ANOVA or ten-fold cross-validation followed by a paired t-test can be used [110].
- Avoiding Data Leakage: Data leakage, where information from the test set inadvertently influences the training process, is a catastrophic failure in benchmarking. Safeguards include [111]:
- Examining global explanations (e.g., permutation feature importance) to identify illogical proxy features.
- Conducting ablation experiments to remove suspected proxy features.
- Running silent trials on infrastructure that mirrors the deployment environment.
- Fairness and Bias Evaluation: Benchmarking must include an evaluation of algorithmic bias. This involves stratifying model performance across key subpopulations defined by sex, age, socioeconomic status, and race/ethnicity (where available) [111]. Satisfying all fairness criteria is often impossible, making clinical input crucial for defining context-appropriate fairness goals [111].
Performance Metrics and Evaluation Criteria
The choice of performance metrics must be aligned with the biomarker's intended use and clinical context.
Table 2: Core Performance Metrics for Biomarker Model Evaluation
| Metric Category | Specific Metric | Clinical/Regulatory Relevance |
|---|---|---|
| Diagnostic Accuracy | Sensitivity, Specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV) [13] | Fundamental for diagnostic and screening biomarkers. PPV/NPV are influenced by disease prevalence. |
| Discrimination | Area Under the Receiver Operating Characteristic Curve (AUC-ROC) [13] | Measures how well the model separates cases from controls. A value of 0.5 is no better than chance. |
| Calibration | Calibration Plots, Brier Score [13] | Assesses how well the model's predicted probabilities match the actual observed frequencies. Critical for risk stratification. |
| Operational Metrics | Number Needed to Alert (NNA), Alert Burden [111] | In deployment, balances the cost of false alerts (resource use) against the consequence of missed outcomes. |
For classification tasks, the selection of a probability threshold is a key decision that balances intervention downsides (e.g., alert burden) with the consequences of a missed outcome [111]. This threshold should not be chosen based on a single metric like Youden's index alone but should be determined collaboratively with clinical stakeholders by presenting operational data (PPV, Sensitivity, NNA) at multiple thresholds [111].
The MLOps Framework for Reproducible Benchmarking
A Machine Learning Operations (MLOps) paradigm is essential for productionizing ML systems and ensuring benchmarking is automated, reproducible, and modular [111]. Key components include:
- Experimentation: An orchestrated pipeline that handles feature extraction, model training, evaluation, and selection on a static set of data to ensure reproducibility [111]. All experiments must be tracked, storing metadata about models, features, and results [110].
- Model Design and Generalization: The model must be tailored to the available data and intended use [108]. Learning curves, which plot evaluation metrics against time or training iterations, are vital tools for diagnosing overfitting (where training performance improves but validation performance stagnates or worsens) and ensuring the model generalizes well [110].
Diagram 1: ML model benchmarking and validation workflow.
Protocol: A Step-by-Step Benchmarking and Validation Pipeline
This protocol provides a detailed methodology for benchmarking ML models for biomarker discovery, incorporating regulatory and clinical considerations.
Protocol 1: Retrospective Benchmarking and Confirmation
Objective: To compare the performance of multiple ML algorithms for a specific biomarker discovery task using a retrospective dataset and select the best candidate for further validation.
Materials and Reagents:
- Table 3: Research Reagent Solutions for ML Benchmarking
| Reagent / Resource | Function / Explanation |
|---|---|
| Curated Dataset (e.g., from GEO, Proteomics repositories) [112] | Provides the labeled data (e.g., case/control, response/non-response) for model training and testing. |
| Trusted Research Environment (e.g., SEDAR at SickKids) [111] | A secure, centralized data repository with a standardized schema that ensures data integrity and facilitates feature extraction. |
| Experiment Tracking Tool (e.g., Neptune.ai) [110] | Logs all experiment metadata, parameters, and results to ensure reproducibility and facilitate model comparison. |
| Statistical Software (e.g., R, Python with scikit-learn) | Provides the computational environment for data preprocessing, model training, statistical testing, and visualization. |
Procedure:
- Define Cohort and Label: In close collaboration with clinical domain experts, define the patient cohort and the target outcome (label) for the biomarker. Ensure the definition accurately reflects the clinical workflow to avoid introducing bias or data leakage [111]. For example, if predicting heart transplant, the label should be "death or waitlisted for transplant," not just "transplant," as waitlist status is known prospectively [111].
- Data Partitioning: Split the dataset into three independent sets: training (~70%), validation (~15%), and a held-out test set (~15%). The test set must be locked away and used only for the final evaluation of the selected model. Ensure splits are representative of the overall population and consider stratified splitting to preserve the distribution of the outcome [108].
- Model Training and Selection: a. Train multiple candidate models (e.g., Logistic Regression, Random Forest, XGBoost, simple Neural Networks) on the training set using a cross-validation scheme. b. Use the validation set for hyperparameter tuning and for selecting the best-performing model architecture based on pre-defined primary metrics (e.g., AUC). c. Employ statistical tests (e.g., 10-fold cross-validation with a paired t-test) to confirm that performance differences between the top models are statistically significant [110].
- Comprehensive Model Evaluation: a. Perform a final assessment of the selected model on the held-out test set, reporting a comprehensive set of metrics (see Table 2). b. Conduct a bias/fairness assessment by stratifying test set performance across relevant demographic and clinical subgroups [111]. c. Perform interpretability analysis (e.g., using SHAP, LIME, or permutation feature importance) to ensure the model's decisions are based on clinically plausible features [89] [11].
- Documentation and Reporting: Document the entire process, including cohort definition, data preprocessing steps, all models tested, hyperparameters, full results on the test set, and interpretability analyses. This is essential for regulatory submission and scientific transparency [108].
Protocol 2: Integration into Clinical Workflow and Prospective Validation
Objective: To evaluate the performance and clinical impact of a previously benchmarked ML model in a real-world, prospective setting, integrated into a clinical workflow.
Procedure:
- Integration and Interface Development: Work with clinical engineers and IT staff to integrate the model prediction into the Electronic Health Record (EHR) system or a separate clinical decision support interface. The output must be presented to clinicians in a clear, actionable format with essential information and uncertainty estimates [111] [108].
- Silent Trial: Run the model in "silent mode" (predictions are generated and logged but not shown to clinicians) for a predefined period. This provides a prospective validation of the model's performance on live, streaming data without interfering with care [111].
- Clinical Workflow Design: Collaborate with the clinical champion and end-users (e.g., physicians, nurses) to design the new clinical workflow. Define the clinical action triggered by the model's prediction and establish clear authority for clinicians to override the AI output [111] [109].
- Pilot Deployment and Evaluation: Deploy the model for a pilot group of clinicians. Evaluate the performance of the "human-AI team" [108], focusing on clinical utility outcomes such as:
- Adherence to the intended clinical protocol.
- Impact on process measures (e.g., time to diagnosis, appropriate ordering of tests).
- Ultimately, patient outcomes and resource utilization.
- Monitoring and Maintenance: Establish a continuous monitoring system to track model performance and data drift over time. Manage the risks associated with model re-training, ensuring that updated models are validated with the same rigor as the original [108].
Diagram 2: The total product life cycle for a clinical ML model.
The path to regulatory approval and successful clinical implementation for ML-based biomarkers is underpinned by meticulous, transparent, and clinically grounded benchmarking. This requires a disciplined approach that prioritizes methodological rigor over algorithmic novelty, emphasizes model interpretability and generalizability, and is embedded within a multi-disciplinary framework from inception [89] [108]. By adhering to the protocols and principles outlined in this document—from robust retrospective comparison and fairness evaluations to prospective silent trials and continuous monitoring—researchers and drug development professionals can build the evidentiary foundation necessary to translate promising computational models into trustworthy tools that enhance patient care and achieve regulatory endorsement.
Conclusion
Machine learning has indisputably revolutionized biomarker discovery, enabling a shift from reductionist single-analyte approaches to a holistic, data-driven paradigm that captures the complex, multi-faceted nature of disease. The successful integration of diverse data types through sophisticated algorithms allows for the identification of robust, clinically actionable biomarkers. However, the path from computational discovery to clinical application is paved with challenges, including the critical need for rigorous validation, model interpretability, and standardization. Future progress hinges on developing more trustworthy AI systems, fostering collaborative partnerships between computational and clinical domains, and adapting regulatory frameworks to accommodate dynamic ML-driven models. By addressing these challenges, the field is poised to fully realize the promise of AI in delivering personalized diagnostic, prognostic, and therapeutic strategies, ultimately advancing precision medicine and improving patient outcomes.
References
- 1. The Biomarker Toolkit — an evidence-based guideline to ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-03075-3]
- 2. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 3. A Perspective on Challenges and Issues in Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2773185/]
- 4. The benefits and pitfalls of machine learning for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558383/]
- 5. Biomarkers: Potential Uses and Limitations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC534923/]
- 6. Study Designs and Statistical Analyses for Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3444086/]
- 7. What Are Biomarkers? Definition, Applications and ... [https://blog.omni-inc.com/blog/what-are-biomarkers-and-whats-new-in-2025]
- 8. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 9. Machine learning enhances biomarker discovery: From multi [https://esmed.org/MRA/mra/article/view/6888]
- 10. Biomarker definitions and their applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5813875/]
- 11. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 12. An introductory guide to biomarkers, precision, ... [https://www.almacgroup.com/diagnostics/diagnostic-resource/an-introductory-guide-to-biomarkers-precision-personalised-and-stratified-medicine/]
- 13. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 14. Prognostic and Predictive Biomarkers: Tools in Personalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4031398/]
- 15. Prognostic and predictive biomarker developments in multiple ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-021-01162-7]
- 16. Machine learning approaches for biomarker discovery to ... [https://www.nature.com/articles/s41598-023-42338-0]
- 17. Biomarker Discovery: Types, Phases and Applications [https://lifesciences.danaher.com/us/en/library/biomarker-discovery.html]
- 18. The Power of Multi-Omics: Understanding the Omes [https://frontlinegenomics.com/the-power-of-multi-omics-understanding-the-omes/]
- 19. Supporting Multi-omics Approaches [https://www.thermofisher.com/us/en/home/brands/thermo-scientific/molecular-biology/molecular-biology-learning-center/molecular-biology-resource-library/spotlight-articles/supporting-multi-omics-approaches.html]
- 20. Challenges in AI-driven multi-omics data analysis for ... [https://www.sciencedirect.com/science/article/pii/S2352914825000681]
- 21. Challenges in multi-omics data integration [https://www.mindwalkai.com/blog/challenges-in-multi-omics-data-integration]
- 22. Multi-Omics Integration for the Design of Novel Therapies and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10594525/]
- 23. A guide to multi-omics data collection and integration for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9747357/]
- 24. Network-based multi-omics integrative analysis methods in ... [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-025-00442-z]
- 25. A Multi-Omics Integration Framework with Automated ... [https://pubmed.ncbi.nlm.nih.gov/40806769/]
- 26. Integrative multi-omics and machine learning reveal critical ... [https://www.nature.com/articles/s41698-025-01027-z]
- 27. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 28. A Review on Biomarker‐Enhanced Machine Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421415/]
- 29. Development and validation of machine learning models with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11925590/]
- 30. Machine Learning and Artificial Intelligence for Infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299889/]
- 31. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 32. key Uncovering , potential therapeutic targets... | PLOS One biomarkers [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330780]
- 33. Frontiers | Leveraging the integration of bioinformatics and machine ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1574157/full]
- 34. Imaging biomarkers in optic neuritis: current tools and future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531036/]
- 35. Large-Scale Automatic Feature Selection for Biomarker ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2019.00452/full]
- 36. Research Article Benchmarking feature selection and ... [https://www.sciencedirect.com/science/article/pii/S2001037024000692]
- 37. Benchmark study of feature selection strategies for multi-omics ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-04962-x]
- 38. A technical review of multi-omics data integration methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315550/]
- 39. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 40. Matthews correlation coefficient-based feature ranking in ... [https://www.sciencedirect.com/science/article/pii/S2666827025001409]
- 41. Multi-Omics Feature Selection to Identify Biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12471784/]
- 42. SMOPCA: spatially aware dimension reduction integrating ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03576-9]
- 43. Intrinsic-dimension analysis for guiding dimensionality ... [https://www.sciencedirect.com/science/article/pii/S0933365724002914]
- 44. Basic Comparison Between RandomForest, SVM, and ... [https://medium.com/@ap.nattapoj_st/basic-comparison-between-randomforest-svm-and-xgboost-0e5862871175]
- 45. XGBoost Parameters [https://www.geeksforgeeks.org/machine-learning/xgboost-parameters/]
- 46. XGB-BIF: An XGBoost-Driven Biomarker Identification ... [https://pubmed.ncbi.nlm.nih.gov/40565055/]
- 47. Data-Driven Facies Prediction: A Comparative Study of ... [https://eartharxiv.org/repository/view/9382/]
- 48. Random Forests(TM) in XGBoost [https://xgboost.readthedocs.io/en/stable/tutorials/rf.html]
- 49. Deep learning facilitates multi-data type analysis and ... [https://www.sciencedirect.com/science/article/pii/S2001037023000405]
- 50. Biological insights and novel biomarker discovery through ... [https://www.nature.com/articles/s41523-023-00518-1]
- 51. Convolutional neural network for biomarker discovery ... [https://www.sciencedirect.com/science/article/pii/S2405844023020261]
- 52. Biomarker Analysis in Drug Development [https://blog.crownbio.com/biomarker-analysis-drug-development-precision-medicine]
- 53. Explainable machine learning framework for biomarker ... [https://www.nature.com/articles/s41598-025-98948-3]
- 54. Ten quick tips for biomarker discovery and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371329/]
- 55. AI/ML advances in non-small cell lung cancer biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10750392/]
- 56. Multimodal integration strategies for clinical application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405423/]
- 57. Multi-Omics Biomarker Integration: A Systems Approach [https://www.motif.bio/blog/multi-omics-biomarker-integration-2025]
- 58. A machine learning approach for multimodal data fusion ... [https://www.nature.com/articles/s41698-025-00917-6]
- 59. Multi-modal deep learning framework for early detection of ... [https://www.nature.com/articles/s41598-025-21407-6]
- 60. Method/ology of Phases of Biomarker Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10312229/]
- 61. AI-driven fusion of multimodal data for Alzheimer's disease ... [https://www.nature.com/articles/s41467-025-62590-4]
- 62. Machine learning approaches for biomarker discovery to ... [https://pubmed.ncbi.nlm.nih.gov/37704672/]
- 63. Machine learning-based marker for coronary artery disease [https://www.sciencedirect.com/science/article/abs/pii/S0140673622020797]
- 64. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 65. Deep learning facilitates multi-data type analysis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9929204/]
- 66. How to Integrate Data from Multiple Sources (2025 Guide) [https://www.domo.com/learn/article/integrate-data-from-multiple-sources]
- 67. Top Data Integration Techniques for 2025 [https://airbyte.com/data-engineering-resources/data-integration-techniques]
- 68. Overfitting in prediction models – Is it a problem only in ... [https://www.sciencedirect.com/science/article/abs/pii/S1551714413001031]
- 69. Overfitting In Bioinformatics [https://www.meegle.com/en_us/topics/overfitting/overfitting-in-bioinformatics]
- 70. Validation of Biomarker-based risk prediction models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3896456/]
- 71. High-dimensional Biomarker Identification for Scalable and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11482776/]
- 72. Applying machine learning to high-dimensional proteomics ... [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-025-00634-z]
- 73. The benefits and pitfalls of machine learning for biomarker ... [https://link.springer.com/article/10.1007/s00441-023-03816-z]
- 74. The crucial role of explainable artificial intelligence (XAI) in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535480/]
- 75. Explainable AI in medicine: challenges of integrating XAI ... [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1627169/full]
- 76. A historical perspective of biomedical explainable AI research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10500028/]
- 77. Exploring the Power of Visualization and XAI | by Tianqi Song [https://medium.com/@holliea1027/exploring-the-power-of-visualization-and-xai-6817d2327906]
- 78. The human factor in explainable artificial intelligence [https://www.nature.com/articles/s41746-025-02023-0]
- 79. Batch correction methods used in single-cell RNA sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315870/]
- 80. Batch Effect Correction [https://www.10xgenomics.com/analysis-guides/introduction-batch-effect-correction]
- 81. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 82. A benchmark of batch-effect correction methods for single-cell ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1850-9]
- 83. Highly effective batch effect correction method for RNA-seq ... [https://www.sciencedirect.com/science/article/pii/S200103702400432X]
- 84. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 85. Exploring the ethical issues posed by AI and big data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581208/]
- 86. FDA Oversight: Understanding the Regulation of Health AI ... [https://bipartisanpolicy.org/issue-brief/fda-oversight-understanding-the-regulation-of-health-ai-tools/]
- 87. AI Medical Devices: 2025 Status, Regulation & Challenges [https://intuitionlabs.ai/articles/ai-medical-devices-regulation-2025]
- 88. Data privacy in healthcare: Global challenges and solutions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12138216/]
- 89. A 2025 perspective on the role of machine learning for ... [https://pubmed.ncbi.nlm.nih.gov/40772544/]
- 90. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 91. Color Contrast Accessibility: Complete WCAG 2025 Guide ... [https://www.allaccessible.org/blog/color-contrast-accessibility-wcag-guide-2025]
- 92. Evaluating the Clinical Utility of a Biomarker - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3138723/]
- 93. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 94. How to explain the ROC curve and ROC AUC score? [https://www.evidentlyai.com/classification-metrics/explain-roc-curve]
- 95. A guide to interpreting the area under the curve value [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 96. Machine learning based prediction of cognitive metrics ... [https://pubmed.ncbi.nlm.nih.gov/40436987/]
- 97. Methods for Evaluating Novel Biomarkers – a New Paradigm [https://pmc.ncbi.nlm.nih.gov/articles/PMC3057673/]
- 98. DNA methylation in breast cancer: early detection and biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020129/]
- 99. Increasing the reproducibility of fluid biomarker studies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7721731/]
- 100. Ten quick tips for biomarker discovery and validation analyses ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1010357]
- 101. Improved analytical workflow towards machine learning ... [https://www.sciencedirect.com/science/article/pii/S0039914025008793]
- 102. Machine learning comparison for biomarker level ... [https://www.nature.com/articles/s41598-025-16185-0]
- 103. Large-Scale Automatic Feature Selection for Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6532608/]
- 104. Comparison of five supervised feature selection algorithms ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-04678-y]
- 105. A Hybrid Sequential Feature Selection Approach for ... [https://pubmed.ncbi.nlm.nih.gov/40723835/]
- 106. Biomarker Utilization for Regulatory Decision Making [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619682/]
- 107. Practically Significant Method Comparison Protocols for ... [https://pubmed.ncbi.nlm.nih.gov/40932128/]
- 108. Good Machine Learning Practice for Medical Device ... [https://www.fda.gov/medical-devices/software-medical-device-samd/good-machine-learning-practice-medical-device-development-guiding-principles]
- 109. AI, Biomarker Legislation, and the Healthcare Policy Landscape [https://www.avalonhcs.com/resources/ai-biomarker-legislation-and-the-healthcare-policy-landscape-a-strategic-update-for-executives/]
- 110. How to Compare Machine Learning Models and Algorithms [https://neptune.ai/blog/how-to-compare-machine-learning-models-and-algorithms]
- 111. A roadmap to implementing machine learning in healthcare [https://pmc.ncbi.nlm.nih.gov/articles/PMC11788154/]
- 112. A beginner's guide into curated analyses of open access ... [https://www.nature.com/articles/s41597-023-02338-1]