Optimization Algorithms for Parameter Estimation in Drug Development: From Foundational Principles to AI-Driven Applications
This article provides a comprehensive exploration of optimization algorithms for parameter estimation, tailored for researchers and drug development professionals.
Optimization Algorithms for Parameter Estimation in Drug Development: From Foundational Principles to AI-Driven Applications
Abstract
This article provides a comprehensive exploration of optimization algorithms for parameter estimation, tailored for researchers and drug development professionals. It covers the foundational principles of parameter estimation within Model-Informed Drug Development (MIDD) and fit-for-purpose modeling frameworks. The piece delves into specific methodological applications, including AI and machine learning integration, advanced hybrid algorithms like HSAPSO, and their use in pharmacokinetic/pharmacodynamic (PK/PD) modeling and ADMET prediction. It also addresses critical troubleshooting strategies for overcoming common challenges such as data quality issues and model overfitting, and concludes with rigorous validation techniques and comparative analyses of different algorithmic approaches to ensure regulatory readiness and robust model performance.
The Core Principles: Understanding Parameter Estimation in Modern Drug Development
The Pivotal Role of Parameter Estimation in Model-Informed Drug Development (MIDD)
Technical Support: Frequently Asked Questions (FAQs)
FAQ 1: Why are my parameter estimates unstable or associated with unacceptably high variance?
- Problem Explanation: This is a classic symptom of multicollinearity, where strong correlations between explanatory variables inflate the variance of parameter estimates. It can lead to unreliable coefficients with unexpected signs and reduced model reliability [1].
- Solution:
- For Generalized Linear Models (e.g., Poisson Regression): Replace the standard Poisson Maximum Likelihood Estimator (PMLE) with a robust biased estimator. The proposed Robust Poisson Two-Parameter Estimator (PMT-PTE) is designed to handle both multicollinearity and outliers simultaneously, providing more stable estimates [1].
- General Practice: Incorporate regularization techniques (e.g., ridge regression) that introduce a small bias to achieve a substantial reduction in the variance of the estimates.
FAQ 2: How can I efficiently perform covariate selection for a Nonlinear Mixed-Effects (NLME) model without repeated, time-consuming model runs?
- Problem Explanation: Traditional stepwise covariate selection requires manually testing numerous covariate-parameter combinations, which is computationally expensive and inefficient [2].
- Solution:
- Adopt a novel Generative AI framework using Variational Autoencoders (VAEs). This method replaces the standard Evidence Lower Bound objective with one based on the corrected Bayesian information criterion.
- This allows for the simultaneous evaluation of all potential covariate-parameter combinations, enabling automated, joint estimation of population parameters and covariate selection in a single run [2].
FAQ 3: My model's performance is highly sensitive to outliers in the dataset. What robust methods are available?
- Problem Explanation: Outliers can disproportionately influence parameter estimates, distorting results and reducing predictive accuracy. This is a known issue in both linear regression and models like Poisson Regression [1].
- Solution:
- Use robust regression estimators. For Poisson regression, the Transformed M-estimator (MT) can be combined with biased estimators (like the proposed PMT-PTE) to effectively mitigate the influence of outliers while also addressing multicollinearity [1].
- These methods reduce the weight of influential data points, leading to more reliable parameter estimates that better represent the majority of the data.
FAQ 4: What is a "Fit-for-Purpose" approach in MIDD, and how does it guide parameter estimation?
- Problem Explanation: Selecting an overly complex or overly simplistic model can lead to poor predictions and misguided decisions [3].
- Solution:
- Align your modeling and parameter estimation strategy directly with the Key Question of Interest (QOI) and Context of Use (COU) [3].
- For early discovery (e.g., target identification), simpler models may be sufficient.
- For critical decisions (e.g., dose optimization for regulatory submission), more rigorous methods like Population PK/PD modeling or Quantitative Systems Pharmacology (QSP) are required. The model's level of complexity and the robustness of parameter estimation should be justified by its intended impact on development decisions [3].
FAQ 5: How can I enhance the predictive power and credibility of my mechanistic model?
- Problem Explanation: Models that focus solely on quantitative fit may miss key qualitative, system-level behaviors (e.g., bistability), limiting their predictive value and biological plausibility [4].
- Solution:
- Ensure your model captures emergent properties across biological scales, from molecular interactions to organ-level function [4].
- Integrate foundational biomedical knowledge from physiology and molecular biology into the model structure.
- Proactively and cautiously adapt existing literature models to your specific context through a "learn and confirm" paradigm, critically assessing their biological assumptions and parameter sources before applying them to new data [4].
Experimental Protocols & Methodologies
Protocol: Automated Covariate Selection using a Variational Autoencoder (VAE) Framework
This protocol details the methodology for streamlining covariate selection in NLME models, as presented in the research "Redefining Parameter Estimation and Covariate Selection via Variational Autoencoders" [2].
- Objective: To enable joint estimation of population parameters and covariate selection in a single, automated run.
- Background: NLME models are central to pharmacometrics but traditionally require manual, stepwise covariate model building.
- Materials/Software:
- NLME dataset
- VAE software framework as described in the primary research [2]
- Method Steps:
- Model Setup: Define the base NLME model without covariates.
- VAE Integration: Implement the VAE framework, which is designed to learn structured representations from complex, high-dimensional data.
- Objective Function Modification: Replace the standard VAE evidence lower bound (ELBO) objective function with an objective function based on the corrected Bayesian information criterion (BIC).
- Simultaneous Evaluation: Allow the modified VAE framework to evaluate all potential covariate-parameter combinations concurrently within the model optimization process.
- Output: The algorithm outputs the final model, which includes the identified significant covariate-parameter relationships and the associated population parameter estimates.
- Key Outcomes: This approach eliminates the need for manual selection and repeated model fitting, outperforming traditional procedures in efficiency while maintaining high-quality results [2].
Protocol: Implementing a Robust Poisson Two-Parameter Estimator (PMT-PTE)
This protocol outlines the procedure for applying the PMT-PTE to manage outliers and multicollinearity in Poisson regression, based on the work by Lukman et al. [1].
- Objective: To obtain stable and reliable parameter estimates for a Poisson regression model in the presence of multicollinearity and outliers.
- Background: The Poisson Maximum Likelihood Estimator (PMLE) is highly sensitive to both multicollinearity and outliers, which can distort results.
- Materials/Software:
- Dataset with count-based response variable and potentially correlated predictors.
- Statistical software capable of implementing custom estimation routines (e.g., R, Python).
- Method Steps:
- Diagnostics: Confirm the presence of multicollinearity (e.g., via Variance Inflation Factors) and identify potential outliers.
- Estimator Formulation: The proposed PMT-PTE estimator combines the Transformed M-estimator (MT) to handle outliers with a two-parameter biased estimation technique to handle multicollinearity. The form of the estimator is:
PMT-PTE = (D + kI)^{-1}(D + dI) {\hat{\beta}}_{MT}where{\hat{\beta}}_{MT}is the robust Transformed M-estimator,D = X^\prime {\hat{U}} X,kanddare the biasing parameters [1]. - Parameter Selection: Optimize the biasing parameters
kanddto minimize the Mean Squared Error (MSE), typically via Monte Carlo simulation or cross-validation on the specific dataset. - Model Fitting: Solve for the regression coefficients using the proposed PMT-PTE estimator instead of the standard PMLE.
- Key Outcomes: Simulation results indicate that the PMT-PTE estimator outperforms other estimators (like PMLE, Poisson Ridge, etc.) in scenarios with coexisting multicollinearity and outliers, as measured by a lower MSE [1].
Table: Comparison of Poisson Regression Estimators
The following table summarizes the performance characteristics of various estimators for Poisson regression models under different data challenges, as evaluated in a Monte Carlo simulation study [1].
| Estimator Name | Acronym | Primary Strength | Limitations | Reported Performance (MSE) |
|---|---|---|---|---|
| Poisson Maximum Likelihood Estimator | PMLE | Standard, unbiased estimator | Highly sensitive to multicollinearity & outliers | Highest MSE in adverse conditions [1] |
| Poisson Ridge Estimator | - | Handles multicollinearity | Does not address outliers | Higher MSE than robust estimators when outliers exist [1] |
| Transformed M-estimator (MT) | MT | Robust against outliers | Does not fully address multicollinearity | Improved over PMLE, but outperformed by combined methods [1] |
| Robust Poisson Two-Parameter Estimator | PMT-PTE | Handles both multicollinearity & outliers | Requires optimization of two parameters | Lowest MSE when both problems are present [1] |
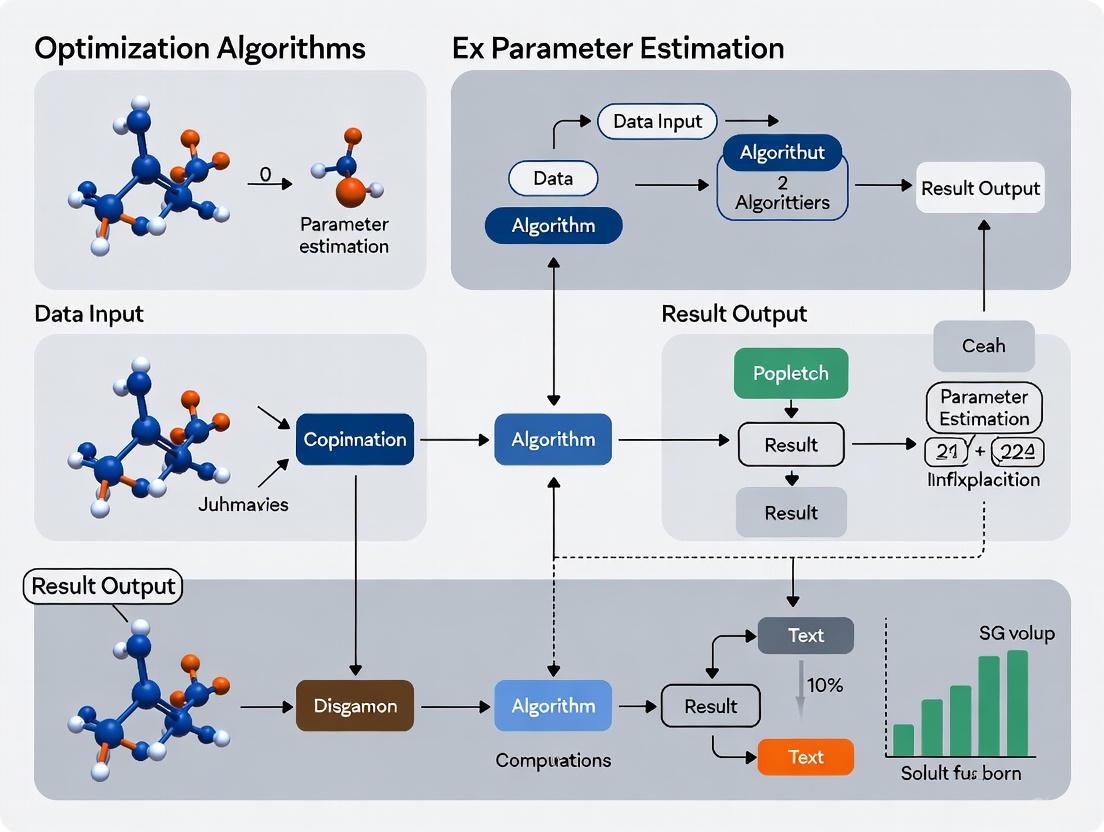
Workflow and Pathway Visualizations
VAE for Covariate Selection Workflow
Multiscale Emergent Properties
Robust Parameter Estimation Logic
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table: Key MIDD and Optimization Tools
This table details essential methodological "tools" and their functions in parameter estimation and model-informed drug development [5] [3] [4].
| Tool / Methodology | Function in Parameter Estimation & MIDD |
|---|---|
| Nonlinear Mixed Effects (NLME) Modeling | A foundational framework for quantifying fixed effects (typical values) and random effects (variability) of parameters in a population [5]. |
| Variational Autoencoder (VAE) | A generative AI framework used to automate and streamline complex tasks like covariate selection and parameter estimation in a single run [2]. |
| Robust Biased Estimators (e.g., PMT-PTE) | A class of statistical estimators designed to provide stable parameter estimates when data suffers from multicollinearity and/or outliers [1]. |
| Quantitative Systems Pharmacology (QSP) | Integrative, multiscale modeling that uses prior knowledge and experimental data to estimate system-specific parameters, helping to predict clinical efficacy and toxicity [3] [4]. |
| Physiologically Based Pharmacokinetic (PBPK) Modeling | A mechanistic approach to estimate and predict drug absorption, distribution, metabolism, and excretion (ADME) based on physiology, drug properties, and experiment data [3]. |
| Model-Based Meta-Analysis (MBMA) | Quantitatively integrates summary results from multiple clinical trials to estimate overall treatment effects and understand between-study heterogeneity [3]. |
| Bayesian Inference | A probabilistic approach to parameter estimation that combines prior knowledge with newly collected data to produce a posterior distribution of parameter values [3]. |
| Iteratively Reweighted Least Squares (IRLS) | The standard algorithm used to compute parameter estimates for Generalized Linear Models, such as the Poisson regression model [1]. |
In modern drug development and parameter estimation research, the "Fit-for-Purpose" (FFP) paradigm ensures that modeling approaches are strategically aligned with specific scientific questions and contexts. FFP modeling provides a structured framework for selecting computational tools that directly address Key Questions of Interest (QOI) within a defined Context of Use (COU). This approach emphasizes that models must be appropriate for their intended application, with validation rigor proportional to the decision-making stakes [3].
A model is considered FFP when it properly defines the COU, ensures data quality, and completes appropriate verification, calibration, and validation. Conversely, models become non-FFP through oversimplification, insufficient data quality, unjustified complexity, or failure to properly define the COU [3]. For researchers in parameter estimation, adopting FFP principles means matching algorithmic complexity to the specific questions being investigated, whether in early discovery, preclinical testing, clinical trials, regulatory submission, or post-market surveillance [3].
Core Concepts and Definitions
Key Questions of Interest (QOI): These are the specific scientific or clinical questions that a model aims to address. In parameter estimation research, QOIs might include identifying optimal dosing strategies, predicting patient population responses, or understanding compound behavior under specific physiological conditions [3].
Context of Use (COU): The COU explicitly defines how the model will be applied, including the specific conditions, populations, and decision points it will inform. This encompasses the intended application within the drug development pipeline or research workflow [3] [6].
Fit-for-Purpose (FFP): This principle ensures that the selected modeling methodology, its implementation, and validation level are appropriate for the specific QOI and COU. The FFP approach balances scientific rigor with practical considerations, avoiding both oversimplification and unnecessary complexity [3].
Troubleshooting Guides and FAQs
FAQ 1: How do I determine if my model is truly "fit-for-purpose"?
Answer: A truly FFP model must meet several criteria. First, it must be precisely aligned with your QOI and have a clearly defined COU. Second, the model must undergo appropriate verification and validation for its intended use. Third, it should utilize data of sufficient quality and quantity. Finally, the model's complexity should be justified—neither oversimplified to the point of being inaccurate nor unnecessarily complex [3].
Troubleshooting Guide:
- Problem: Model predictions consistently deviate from experimental observations.
- Potential Cause: Model may not be FFP due to oversimplification of biological processes.
- Solution: Re-evaluate QOI and COU. Consider incorporating additional mechanistic elements or switching to a more appropriate modeling framework.
- Problem: Model performs well on training data but poorly on validation data.
- Potential Cause: Overfitting or insufficient model validation for the COU.
- Solution: Implement cross-validation, reduce model complexity if necessary, or collect additional validation data specific to the COU.
FAQ 2: What are the most common reasons for model rejection in regulatory submissions?
Answer: Regulatory agencies may reject models that lack a clearly defined COU, have insufficient validation for the intended use, or fail to demonstrate clinical relevance. Specifically for digital endpoints, regulatory feedback has emphasized challenges in interpreting clinical significance when the connection between model outputs and meaningful patient benefits isn't established [6]. One case study involving a novel digital endpoint for Alzheimer's disease received regulatory feedback that although the instrument was sensitive for detecting cognitive changes, the clinical significance of intervention effects was unclear [6].
Troubleshooting Guide:
- Problem: Regulatory questions about clinical meaningfulness of model endpoints.
- Potential Cause: Insufficient connection established between model output and patient-centric outcomes.
- Solution: Conduct additional studies to demonstrate clinical relevance, engage with patient groups to establish meaningfulness, and seek early regulatory consultation.
FAQ 3: How does the "fit-for-purpose" requirement change across drug development stages?
Answer: The FFP requirements evolve significantly throughout the drug development lifecycle. Early discovery stages may utilize simpler models with lower validation requirements, while models supporting regulatory decisions or label claims require the highest level of validation evidence [3] [6].
Table: Evolution of FFP Requirements Across Development Stages
| Development Stage | Typical QOIs | FFP Validation Level | Common Methodologies |
|---|---|---|---|
| Discovery | Target identification, compound optimization | Low to Moderate | QSAR, AI/ML approaches [3] |
| Preclinical | FIH dose prediction, toxicity assessment | Moderate | PBPK, QSP, semi-mechanistic PK/PD [3] |
| Clinical Trials | Dose optimization, patient stratification | Moderate to High | PPK/ER, clinical trial simulation [3] |
| Regulatory Submission | Efficacy confirmation, safety assessment | High | Model-based meta-analysis, virtual population simulation [3] |
| Post-Market | Label updates, population expansion | High | Bayesian inference, adaptive designs [3] |
FAQ 4: What are the key considerations when selecting between different parameter estimation algorithms?
Answer: Algorithm selection should be guided by multiple factors including data structure (sparse vs. rich), model complexity, computational resources, and regulatory acceptance. Bayesian methods are particularly valuable for parameter estimation in complex biological systems with sparse data, as they naturally incorporate prior knowledge and quantify uncertainty [7].
Troubleshooting Guide:
- Problem: Parameter estimates with unacceptably wide confidence intervals.
- Potential Cause: Insufficient data to inform parameters, or structural model identifiability issues.
- Solution: Consider Bayesian approaches with informative priors, redesign experiments to collect more informative data, or simplify model structure.
- Problem: Algorithm convergence failures or excessively long computation times.
- Potential Cause: Model too complex for available data, or inappropriate algorithm selection.
- Solution: Simplify model structure, utilize more efficient optimization algorithms, or increase computational resources.
FAQ 5: How can I assess and mitigate risks associated with model-informed decisions?
Answer: Implement a comprehensive model risk assessment framework that evaluates the impact of model uncertainty on decision-making. This includes sensitivity analysis, uncertainty quantification, and scenario testing. The higher the stakes of the decision being informed, the more robust the risk assessment should be [3].
Troubleshooting Guide:
- Problem: Stakeholder reluctance to accept model-informed decisions.
- Potential Cause: Insufficient communication of model limitations and uncertainties.
- Solution: Develop clear visualizations of uncertainty, implement decision-theoretic frameworks that explicitly incorporate risk, and conduct prospective validation studies.
Methodological Framework and Workflows
The following diagram illustrates the decision process for implementing fit-for-purpose modeling in research and development:
Research Reagent Solutions: Essential Methodologies for Parameter Estimation
Table: Key Methodologies for Parameter Estimation in Biological Modeling
| Methodology | Primary Function | Typical Applications | Regulatory Consideration |
|---|---|---|---|
| Bayesian Inference [7] | Integrates prior knowledge with observed data using probabilistic frameworks | Parameter estimation from sparse data, uncertainty quantification | Well-suited for formal regulatory submissions when priors are well-justified |
| Population PK/PD [3] | Characterizes variability in drug exposure and response across individuals | Dose optimization, covariate effect identification | Established regulatory acceptance with standardized practices |
| PBPK Modeling [3] | Mechanistic modeling of drug disposition based on physiology | Drug-drug interaction prediction, special population dosing | Increasing regulatory acceptance for specific COUs |
| QSP Modeling [3] | Integrates systems biology with pharmacology to simulate drug effects | Target validation, biomarker strategy, combination therapy | Emerging regulatory pathways, early engagement recommended |
| AI/ML Approaches [3] | Pattern recognition and prediction from large, complex datasets | Biomarker discovery, patient stratification, lead optimization | Evolving regulatory landscape, requires rigorous validation |
Implementation Protocols for Common Scenarios
Protocol 1: Bayesian Parameter Estimation for Sparse Data
Background: Appropriate for parameter estimation when dealing with limited observational data, such as in HIV epidemic modeling or rare disease applications [7].
Procedure:
- Define hierarchical model structure incorporating prior knowledge
- Specify appropriate probability distributions for parameters and observables
- Implement Markov Chain Monte Carlo (MCMC) sampling or variational inference
- Conduct convergence diagnostics (Gelman-Rubin statistic, trace plots)
- Validate model using posterior predictive checks
- Quantify uncertainty in parameter estimates and model predictions
Validation: Use cross-validation techniques and compare posterior predictions to held-out data.
Protocol 2: PBPK Model Development for First-in-Human Dose Prediction
Background: Mechanistic modeling approach used to predict human pharmacokinetics from preclinical data [3].
Procedure:
- Collate physicochemical and pharmacokinetic properties of compound
- Develop system parameters for relevant physiology
- Incorporate in vitro-in vivo extrapolation (IVIVE) of clearance mechanisms
- Verify model using preclinical species data
- Predict human PK and determine safe starting dose
- Conduct sensitivity analysis to identify critical parameters
Validation: Compare predictions to observed clinical data as it becomes available.
Protocol 3: Exposure-Response Analysis for Dose Optimization
Background: Population modeling approach to characterize relationship between drug exposure and efficacy/safety outcomes [3].
Procedure:
- Develop population pharmacokinetic model to describe exposure variability
- Identify significant covariates influencing drug exposure
- Develop exposure-response models for primary efficacy and safety endpoints
- Simulate alternative dosing regimens and their predicted outcomes
- Identify optimal dosing strategy balancing efficacy and safety
- Quantify uncertainty in recommended dosing
Validation: Use visual predictive checks and bootstrap methods to evaluate model performance.
Frequently Asked Questions (FAQs)
FAQ 1: What are the most common signs that my gradient-based optimization is failing? You may observe several clear indicators. The loss function converges too quickly to a poor solution with high error, showing little to no improvement over many epochs [8]. The training loss becomes unstable, oscillating erratically or even diverging, which often signals exploding gradients [9]. For recurrent neural networks specifically, a key sign is the model's inability to capture long-term dependencies in sequence data [9].
FAQ 2: When should I consider using an evolutionary algorithm over a gradient-based method? Evolutionary algorithms are particularly advantageous in specific scenarios. They excel when optimizing non-convex objective functions commonly encountered in drug discovery and parameter estimation, where gradient-based methods often get trapped in local optima [10]. They are also highly effective when the objective function lacks differentiability, when dealing with discrete parameter spaces (like molecular structures), or when you need to perform global optimization without relying on derivative information [11] [12].
FAQ 3: How can I improve the convergence speed of my Genetic Algorithm? Recent research demonstrates several effective approaches. The Gradient Genetic Algorithm incorporates gradient information from a differentiable objective function to guide the search direction, achieving up to a 25% improvement in Top-10 scores compared to vanilla genetic algorithms [11]. For Particle Swarm Optimization (PSO), using adaptive parameter tuning (APT) can systematically adjust parameters during the optimization process, significantly enhancing convergence rates [12].
FAQ 4: How do I prioritize which algorithm error to troubleshoot first? A structured approach to prioritization is recommended. First, assess the impact of each error, focusing immediately on those causing system-wide failures or data corruption [13]. Next, consider error frequency, as issues that occur often and disrupt normal workflow should take precedence [13]. Finally, analyze dependencies, prioritizing errors in core components that other parts of your algorithm rely on, as fixing these may resolve multiple issues simultaneously [13].
Troubleshooting Guides
Issue 1: Vanishing or Exploding Gradients in Deep Neural Networks
Problem Description: During backpropagation, gradients become extremely small (vanishing) or excessively large (exploding), leading to slow learning in early layers or unstable training dynamics that prevent convergence [9].
Diagnosis Steps:
- Monitor Gradient Norms: Track the magnitudes (L2-norm) of gradients for each layer during training. A sharp decrease in early layers indicates vanishing gradients, while a sharp increase signals exploding gradients.
- Analyze Weight Updates: Check if weight updates are becoming infinitesimally small or disproportionately large.
- Observe Loss Behavior: A loss that stagnates for extended periods may indicate vanishing gradients. A loss that spikes or becomes NaN (Not a Number) often indicates exploding gradients [8].
Resolution Methods:
- Use Alternative Activation Functions: Replace saturating functions like Sigmoid or Tanh with non-saturating ones like ReLU, Leaky ReLU, or ELU to prevent gradients from shrinking [9].
- Apply Batch Normalization: Normalize the inputs to each layer to maintain zero mean and unit variance, which stabilizes and accelerates training [9].
- Employ Gradient Clipping: For exploding gradients, cap the gradients at a predefined threshold during backpropagation to prevent unstable updates [9].
- Use Proper Weight Initialization: Utilize initialization schemes (e.g., He, Xavier) that are designed to keep the scale of gradients consistent across layers [9].
Prevention Strategies:
- Implement a structured weight initialization strategy from the start.
- Incorporate Batch Normalization layers into your model architecture by default for deep networks.
- Continuously monitor gradient statistics throughout the training process.
Issue 2: Poor Convergence in Evolutionary Algorithms
Problem Description: The algorithm fails to find a satisfactory solution, gets stuck in a local optimum, or converges unacceptably slowly.
Diagnosis Steps:
- Check Diversity: Monitor the population diversity. A rapid loss of diversity suggests the algorithm is converging prematurely to a suboptimal point.
- Analyze Parameter Settings: Evaluate if the algorithm's parameters (e.g., mutation rate, crossover rate, selection pressure) are appropriate for the problem landscape.
- Profile Computational Cost: Determine if the algorithm is hindered by excessive computational overhead per iteration [10].
Resolution Methods:
- Hybridize with Gradient Information: For problems where a differentiable objective function can be defined, incorporate gradient guidance to direct the evolutionary search, as seen in the Gradient Genetic Algorithm [11].
- Implement Adaptive Parameter Tuning: Use methods like Adaptive Parameter Tuning (APT) or Hierarchically Self-Adaptive PSO (HSAPSO) to dynamically adjust algorithm parameters during a run, improving performance and convergence [12] [10].
- Consider a Two-Stage Approach: For complex parameter estimation, algorithms like the Two-stage Differential Evolution (TDE) can be highly effective. The first stage uses a mutation strategy with historical solutions for broad exploration, while the second stage uses a strategy with inferior solutions for refined exploitation, balancing diversity and convergence speed [14].
Prevention Strategies:
- Conduct preliminary experiments to understand the problem landscape and select appropriate algorithm parameters.
- Design experiments with multiple random seeds to account for the stochastic nature of evolutionary algorithms.
- Consider using advanced, self-adaptive algorithms from the outset for complex optimization tasks.
Issue 3: Algorithm Selection for Parameter Estimation
Problem Description: Uncertainty in choosing the most suitable optimization algorithm for a specific parameter estimation problem in research, leading to suboptimal results or excessive computational cost.
Diagnosis Steps:
- Define Problem Characteristics: Determine if the problem is continuous or discrete, convex or non-convex, differentiable or non-differentiable.
- Identify Constraints: Clarify the nature of the constraints (e.g., linear, non-linear, box constraints).
- Assess Computational Budget: Evaluate the available computational resources and the cost of a single function evaluation.
Resolution Methods:
- Leverage Problem Structure: If the problem is differentiable and convex, gradient-based methods (e.g., SGD, Adam) are typically efficient. For non-convex, non-differentiable, or discrete problems, evolutionary methods (e.g., GA, DE, PSO) are often more robust [12] [15].
- Consult Performance Tables: Refer to comparative studies and performance tables (see Table 2 below) to understand the strengths and weaknesses of different algorithms on benchmark problems.
- Start Simple, Then Scale: Begin with a well-understood, simple algorithm to establish a baseline performance. Then, progress to more sophisticated methods like self-adaptive PSO [10] or TDE [14] if needed.
Prevention Strategies:
- Maintain a toolkit of different optimization algorithms.
- Stay updated on recent algorithmic advancements and their proven application domains.
Performance Data Tables
Table 1: Quantitative Performance of Advanced Optimization Algorithms
This table summarizes the reported performance gains of several advanced algorithms over their traditional counterparts as cited in recent literature.
| Algorithm | Key Innovation | Benchmark/Application | Reported Improvement | Citation |
|---|---|---|---|---|
| Gradient GA | Incorporates gradient guidance into genetic algorithms | Molecular design benchmarks | Up to 25% improvement in Top-10 score vs. vanilla GA | [11] |
| TDE (Two-stage DE) | Novel mutation strategy using historical & inferior solutions | PEMFC parameter estimation (SSE minimization) | 41% reduction in SSE; 98% more efficient (0.23s vs 11.95s) | [14] |
| HSAPSO-SAE | Hierarchically Self-Adaptive PSO for autoencoder tuning | Drug classification (DrugBank, Swiss-Prot) | 95.5% accuracy; computational cost of 0.010s per sample | [10] |
Table 2: Troubleshooting Guide for Common Optimization Problems
This table provides a quick-reference guide for identifying and addressing common issues across different algorithm types.
| Problem | Likely Causes | Recommended Solutions |
|---|---|---|
| Vanishing Gradients | Saturating activation functions (Sigmoid/Tanh), poor weight initialization, very deep networks [9] | Use ReLU/Leaky ReLU, Batch Normalization, proper weight initialization [9] |
| Exploding Gradients | Large weights, high learning rate, unscaled input data [9] | Gradient clipping, lower learning rate, weight regularization, input normalization [9] |
| Premature Convergence (EA) | Loss of population diversity, excessive selection pressure, incorrect mutation rate [12] | Adaptive parameter tuning [12], hybrid approaches [11], fitness sharing |
| Slow Convergence (EA) | Poor exploration/exploitation balance, inadequate parameter settings [11] [12] | Incorporate gradient guidance [11], use adaptive parameter tuning [12] |
Experimental Protocols
Protocol 1: Demonstrating the Vanishing/Exploding Gradient Problem
Objective: To empirically observe and compare the effects of activation functions and initialization on gradient stability in a Deep Neural Network (DNN).
Materials:
- Dataset: A synthetic binary classification dataset (e.g., from
sklearn.datasets.make_classificationormake_moons). - Libraries: Python with TensorFlow/Keras or PyTorch, NumPy, Matplotlib.
Methodology:
- Model Architecture: Construct two DNNs with identical, sufficiently deep architectures (e.g., 10 layers with 10-50 neurons each).
- Variable Manipulation:
- For vanishing gradients, train one model with
sigmoidactivation and another withReLUactivation, using standard initialization (e.g., Glorot) [9]. - For exploding gradients, train a deep model (e.g., 50 layers) with a very high learning rate (e.g., 1.0) and large initial weights (e.g., stddev=3.0), comparing it to a model trained with a low learning rate and small initial weights [9].
- For vanishing gradients, train one model with
- Data Collection:
- Record the training loss over epochs for both models.
- For vanishing gradients, approximate the average gradient magnitude by comparing weight changes before and after a training epoch [9].
- Analysis:
- Plot the loss curves for both models. The model with
sigmoidactivation will typically show slow or stalled convergence, while theReLUmodel will converge faster [9]. - For the exploding gradient test, the model with high learning rate and large weights will show an unstable, spiking loss curve.
- Plot the loss curves for both models. The model with
Protocol 2: Benchmarking an Evolutionary Algorithm for Parameter Estimation
Objective: To evaluate the performance of a Two-stage Differential Evolution (TDE) algorithm against a traditional DE variant for a parameter estimation task.
Materials:
- Problem: A parameter estimation problem with a known ground truth or a standard benchmark function (e.g., from CEC test suites). The Proton Exchange Membrane Fuel Cell (PEMFC) model with seven critical parameters is used in the source study [14].
- Metrics: Sum of Squared Errors (SSE) between estimated and true values, convergence time, and robustness (standard deviation of results over multiple runs) [14].
Methodology:
- Algorithm Setup: Implement or obtain code for the TDE algorithm and a baseline DE algorithm (e.g., HARD-DE) [14].
- Experimental Run: Conduct multiple independent runs of each algorithm on the selected problem, ensuring both use the same computational budget (number of function evaluations).
- Data Collection: For each run, record the final best solution, the SSE at convergence, and the runtime.
- Analysis:
- Compare the minimum, maximum, and average SSE achieved by both algorithms. TDE is reported to achieve a lower minimum SSE and a significantly improved maximum SSE, indicating superior robustness [14].
- Compare the average runtime. TDE has been shown to be significantly more efficient [14].
- Perform statistical tests (e.g., Wilcoxon signed-rank test) to confirm the significance of the performance differences.
Workflow and Algorithm Diagrams
Gradient GA High-Level Workflow
Troubleshooting Gradient Problems
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Computational Tools and Resources
| Item | Function/Description | Relevance to Optimization Research |
|---|---|---|
| Stacked Autoencoder (SAE) | A deep learning model used for unsupervised feature learning and dimensionality reduction. | Serves as a powerful feature extractor in hybrid frameworks like optSAE+HSAPSO for drug classification [10]. |
| Differentiable Objective Function | A parameterized function (e.g., via a neural network) whose gradients can be computed with respect to its inputs. | Enables the incorporation of gradient guidance into traditionally non-gradient algorithms like the Genetic Algorithm [11]. |
| Discrete Langevin Proposal | A method for enabling gradient-based guidance in discrete spaces. | Critical for applying gradient techniques to discrete optimization problems, such as molecular design [11]. |
| Hierarchically Self-Adaptive PSO (HSAPSO) | A variant of Particle Swarm Optimization that dynamically adjusts its own parameters at multiple levels during the search process. | Used for hyperparameter tuning of deep learning models, improving accuracy and computational efficiency in drug discovery [10]. |
| Two-stage Differential Evolution (TDE) | A DE variant that uses a novel dual mutation strategy to enhance exploration and exploitation. | Provides high accuracy, robustness, and computational efficiency for complex parameter estimation tasks, such as in fuel cell modeling [14]. |
| Particle Swarm Optimization (PSO) | A swarm intelligence algorithm that optimizes a problem by iteratively trying to improve a candidate solution. | A foundational evolutionary algorithm often used as a baseline and enhanced with methods like adaptive parameter tuning [12]. |
The Impact of Accurate Parameter Estimation on Reducing Late-Stage Attrition and Development Costs
Frequently Asked Questions
1. Why is parameter estimation so critical in early-stage drug discovery? In drug discovery, parameter estimation involves using computational and statistical methods to precisely determine key biological and chemical variables, such as binding affinities, kinetic rates, and toxicity thresholds. Accurate estimates are foundational for building predictive models of a drug candidate's behavior. Errors at this stage can lead to flawed predictions, causing promising candidates to be wrongly abandoned or, conversely, allowing ineffective or toxic compounds to progress. This wastes significant resources, as the cost of development increases dramatically at each subsequent phase [16] [17].
2. How can machine learning models for parameter estimation be troubleshooted for overfitting? Overfitting occurs when a model learns the noise in the training data instead of the underlying relationship, harming its predictive power on new data. To troubleshoot this:
- Apply Resampling and Validation: Use techniques like k-fold cross-validation and hold back a portion of your data as a validation set to test the model's performance on unseen data [17].
- Use Regularization Methods: Apply regression methods like Ridge, LASSO, or elastic nets, which add penalties to parameters as model complexity increases, forcing the model to generalize [17].
- Implement Dropout: In deep neural networks, randomly remove units in the hidden layers during training to prevent the network from becoming too reliant on any single node [17].
- Simplify the Model: Check if your model structure is too complex for the amount of data available. Using a simpler model or reducing the model order can often prevent overfitting [18].
3. What are common data-related issues that hinder parameter estimation, and how can they be resolved? Data deficiencies are a primary source of estimation problems.
- Issue: Insufficient System Excitation: Simple inputs (e.g., a step input) may not adequately provoke the full range of system dynamics needed to estimate parameters accurately [18].
- Solution: Design experiments with input signals that perturb the system across a wider range of conditions to gather more informative data [18].
- Issue: Poor Data Quality: Data may contain drift, outliers, missing samples, or offsets [18].
- Solution: Preprocess estimation data to correct for these deficiencies before fitting models [18].
- Issue: Low-Volume or Low-Quality Training Data: The predictive power of any machine learning approach is highly dependent on high volumes of high-quality data [17].
- Solution: Invest in generating systematic, comprehensive, and high-dimensional data sets. The practice of ML is said to consist of at least 80% data processing and cleaning [17].
4. How should initial parameter guesses and model structures be selected? Poor initial choices can cause algorithms to converge to a local optimum or fail entirely.
- Initial Guesses: Base initial parameter guesses on prior knowledge of the system or from earlier, simpler experiments. When confident in your initial guesses, specify a smaller initial parameter covariance to give them more importance during estimation [18].
- Model Structure: Start with the simplest model structure that can capture the system dynamics. AR and ARX model structures are good first candidates for linear models due to their algorithmic simplicity and lower sensitivity to initial guesses. Avoid unnecessarily complex models [18].
Quantitative Impact of R&D Costs and Machine Learning
Table 1: Estimated R&D Cost per New Drug [16]
| Drug Type | Cost Range (2018 USD) | Key Notes |
|---|---|---|
| All New Drugs | $113 million - $6 billion+ | Broad range includes new molecular entities, reformulations, and new indications. |
| New Molecular Entities (NMEs) | $318 million - $2.8 billion | Narrower range for novel drugs; highlights high cost of innovative R&D. |
Table 2: Machine Learning Applications in Drug Discovery [17]
| Stage in Pipeline | ML Application | Potential Impact |
|---|---|---|
| Target Identification | Analyzing omics data for target-disease associations. | Provides stronger evidence for novel targets, reducing early scientific attrition. |
| Preclinical Research | Small-molecule compound design and optimization; bioactivity prediction. | Improves hit rates and reduces synthetic effort on poor candidates. |
| Clinical Trials | Identification of prognostic biomarkers; analysis of digital pathology data. | Enriches patient cohorts, predicts efficacy, and improves trial success probability. |
Experimental Protocols for Robust Parameter Estimation
Protocol 1: Building a Predictive Bioactivity Model using Machine Learning
Objective: To train a model that accurately predicts compound bioactivity to prioritize candidates for synthesis and testing.
- Data Curation: Collect a high-quality dataset of chemical compounds with associated bioactivity measurements (e.g., IC50, Ki). This is the most critical step.
- Feature Engineering: Represent each compound using numerical features (e.g., molecular descriptors, fingerprints).
- Model Selection and Training:
- Split data into training, validation, and test sets.
- Train a selected algorithm (e.g., Random Forest, Graph Neural Network) on the training set.
- Use the validation set to tune hyperparameters and apply techniques like dropout or regularization to avoid overfitting [17].
- Model Validation: Evaluate the final model's performance on the held-out test set using metrics such as AUC, precision-recall, and mean squared error [17].
Protocol 2: Tuning a Parameter Estimation Algorithm for a Specific Biological System
Objective: To optimize an optimization algorithm's performance for estimating parameters in a complex, non-linear biological model.
- Problem Formulation: Define the objective function, often as the Root Mean Square Error (RMSE) between model predictions and experimental data [19].
- Algorithm Selection and Enhancement:
- Select a base metaheuristic algorithm (e.g., a nature-inspired optimizer).
- To address common issues like premature convergence, integrate enhancement strategies such as a memory mechanism (to preserve elite solutions), an evolutionary operator (to encourage diversity), and a stochastic local search (for intensive refinement) [20].
- Benchmarking: Compare the performance of the enhanced algorithm against standard algorithms on your specific dataset, using the minimized objective function value and convergence speed as key metrics [20].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Resources for Computational Drug Discovery
| Item | Function |
|---|---|
| High-Throughput Screening (HTS) Data | Provides large-scale experimental data on compound activity, used as a foundational dataset for training and validating ML models [17]. |
| Multi-Omics Datasets (Genomics, Proteomics, etc.) | Enables systems-level understanding of disease mechanisms and identification of novel drug targets [17]. |
| Graph Convolutional Network (GCN) | A type of deep neural network ideal for analyzing structured data like molecular graphs, directly from their structure without needing pre-defined fingerprints [17]. |
| Recursive Least Squares (RLS) Estimator | An online estimation algorithm useful for systems that are linear in their parameters; valued for its simplicity and ease of implementation [18]. |
Workflow and Impact Diagrams
Impact of Parameter Estimation
Parameter Estimation Workflow
Algorithmic Innovations: Applying Advanced Optimization to Drug Development Challenges
Troubleshooting Guides
Troubleshooting Guide 1: Handling Non-Identifiable PK/PD Models
Problem: The parameter estimation algorithm fails to converge, or results in highly uncertain parameter estimates for a parent drug and its metabolite.
Explanation: This often indicates an identifiability problem, where the available data is insufficient to uniquely estimate all parameters in the model [21]. The model structure may violate mathematical principles.
Solution:
- Simplify the Model: Reduce the number of compartments or parameters, especially for the metabolite kinetics, to match the information content of your data.
- Check Data Quality: Ensure your bioanalytical methods are properly validated and that the calibration curve accurately links instrument response to drug concentration [21].
- Re-eassay Study Design: Confirm that the sampling schedule captures key PK/PD events. For future studies, consider whether cassette dosing (administering multiple compounds simultaneously) is appropriate for your goals, though it can sometimes introduce unforeseen interactions [21].
Troubleshooting Guide 2: Optimization Algorithm Stuck in Local Minima
Problem: The machine learning optimization process converges, but the model fits poorly or is not biologically plausible. Small changes in initial parameter guesses lead to different results.
Explanation: Population PK/PD models create a complex, multi-dimensional parameter landscape. Conventional optimization methods like gradient descent can get trapped in a local minimum—a good but not the best solution—instead of finding the global minimum [22].
Solution:
- Use Metaheuristic Algorithms: Implement population-based algorithms like Genetic Algorithms or Ant Colony Optimization which are designed to explore a broader model space and are less prone to getting stuck in local minima [23].
- Run from Multiple Starting Points: Initialize your optimization algorithm from a wide range of different parameter values to survey the landscape.
- Apply Adaptive Optimizers: Use algorithms like Adam (Adaptive Moment Estimation) or RMSprop that adapt the learning rate for each parameter, which can help navigate challenging landscapes [24].
Troubleshooting Guide 3: Poor Out-of-Sample Predictive Performance
Problem: The AI/ML model fits the training data well but fails to accurately predict concentrations or responses for new dosing regimens or patient populations.
Explanation: Purely data-driven AI models (e.g., neural networks, tree-based models) may lack embedded mechanistic understanding of biology (e.g., absorption, distribution, elimination). They learn associations from data but cannot reliably extrapolate beyond the conditions represented in that data [23].
Solution:
- Adopt a Hybrid Approach: Combine mechanistic models (e.g., traditional PK/PD models defined by ordinary differential equations) with ML components. The mechanistic part provides biological structure, while ML identifies complex patterns [23].
- Prioritize Explainable AI (XAI): Use interpretable ML models or build "gray box" models that maintain transparency. This is crucial for both scientific understanding and regulatory acceptance [25].
- Increase Data Quality and Quantity: The core challenge is often limited access to large, high-quality, and reliable datasets for training. Focus on curating robust datasets that cover a wider range of expected conditions [25].
Troubleshooting Guide 4: Managing High Variability in Clinical Data
Problem: A population model cannot adequately capture the high degree of variability in patient responses, leading to poor fits for individual profiles.
Explanation: Understanding and predicting inter-individual variability is inherently difficult, especially when only a few samples are available per patient (sparse data) [25].
Solution:
- Leverage ML for Covariate Analysis: Use unsupervised and supervised ML methods to explore the data for unknown covariate effects and complex, non-linear relationships between patient factors (e.g., weight, genetics) and PK parameters [23].
- Define a Rich Model Space: When using ML-assisted modeling, define a broad model space that includes many potential covariate-parameter relationships and structural models for the algorithm to explore [22].
- Validate with Biological Plausibility: Always review the covariate relationships identified by ML for their biological and clinical plausibility. The role of the scientist is indispensable in this evaluation step [22].
Frequently Asked Questions (FAQs)
FAQ 1: When should I use a metaheuristic algorithm like a Genetic Algorithm over a traditional gradient-based method for PK/PD parameter estimation?
Answer: Use a Genetic Algorithm (GA) when dealing with complex, high-dimensional models where the parameter landscape is likely to have many local minima. GAs perform a global search by evaluating a population of models simultaneously, which gives them a better chance of finding a globally optimal solution compared to gradient-based methods that follow a single path [22] [23]. They are particularly useful for automated structural model selection.
FAQ 2: What are the most common causes of failure in AI/ML-driven PK/PD modeling, and how can I avoid them?
Answer: The most common causes are:
- Data Issues: Insufficient quantity or poor quality of training data. Solution: Invest in robust data generation and curation [25].
- Overfitting: The model learns noise instead of the underlying signal. Solution: Use regularization, cross-validation, and ensure the model is evaluated on a hold-out test set.
- Lack of Biological Plausibility: The model is a "black box" with no grounding in known physiology. Solution: Prefer hybrid models that combine mechanistic principles with ML pattern recognition [23].
FAQ 3: My ML model for predicting drug clearance works well in adults but fails in neonates. What is the likely issue?
Answer: This is a classic problem of extrapolation. Your model was trained on data from one population (adults) and is being applied to a physiologically distinct population (neonates) that was not well-represented in the training data [23]. To address this, use transfer learning techniques to adapt the model with neonatal data, or develop a hybrid PK/ML model that incorporates known physiological differences (e.g., organ maturation functions) as priors [23].
FAQ 4: How can I address the "black box" nature of complex ML models to gain regulatory acceptance for my PK/PD analysis?
Answer: Regulatory agencies emphasize model transparency, validation, and managing bias [25] [26].
- Use Explainable AI (XAI): Employ methods like SHAP (SHapley Additive exPlanations) to interpret the model's predictions.
- Adopt Hybrid Modeling: Ground your ML approach in established PBPK or population PK models. This provides a mechanistic foundation that regulators are familiar with [25].
- Practice Good Machine Learning Practice (GMLP): Maintain rigorous documentation of your model development process, including data provenance, model selection criteria, and validation results [26].
Experimental Protocols
Detailed Protocol: ML-Assisted Population PK Model Development with a Genetic Algorithm
Objective: To automate the selection of a population pharmacokinetic model structure and identify influential covariates using a genetic algorithm (GA).
Background: This non-sequential approach allows for the simultaneous evaluation of multiple model hypotheses and their interactions, which can be missed in traditional stepwise model building [22].
Materials:
- Pharmacokinetic concentration-time data from a clinical study.
- Patient covariate data (e.g., weight, sex, renal function).
- Software with GA capabilities (e.g., Pirana software, custom Python/R scripts).
Methodology:
- Define the Model Space:
- Structural Models: Specify a set of candidate models (e.g., one- vs. two-compartment, first-order vs. saturable elimination, first-order absorption with vs. without lag-time vs. distributed delay) [22].
- Statistical Model: Define options for inter-individual variability (e.g., exponential, proportional) and residual error models.
- Covariate Model: List potential continuous and categorical covariates and their potential relationships (e.g., linear, power) with PK parameters.
Encode the Model Space as "Genes": Represent each combination of structural, statistical, and covariate model choices as a chromosome (a string of genes) in the genetic algorithm.
Define the Fitness Function: Create a scoring function that balances goodness-of-fit (e.g., objective function value, diagnostic plots) with model parsimony (e.g., number of parameters, Akaike Information Criterion). Apply penalties for convergence failures [22].
Run the Genetic Algorithm:
- Initialization: Generate a random population of models.
- Evaluation: Calculate the fitness score for each model.
- Selection: Preferentially select the best-fitting models as "parents."
- Crossover: Create "offspring" models by combining features from two parent models.
- Mutation: Randomly alter a small number of genes in the offspring to introduce new features.
- Repeat: Iterate through selection, crossover, and mutation for a fixed number of generations or until convergence.
Final Model Evaluation: The analyst must review the top-performing model(s) proposed by the GA for biological plausibility, clinical relevance, and robustness before final acceptance [22].
Workflow Diagram: ML-Assisted PK/PD Modeling
Comparison of Optimization Algorithms for Parameter Estimation
| Algorithm | Key Mechanism | Advantages | Common Use Cases in PK/PD |
|---|---|---|---|
| Gradient Descent [24] | Iteratively moves parameters in the direction of the steepest descent of the loss function. | Simple, guaranteed local convergence. | Basic model fitting with smooth, convex objective functions. |
| Stochastic Gradient Descent (SGD) [24] | Uses a single data point (or mini-batch) to approximate the gradient for each update. | Computationally efficient for large datasets; can escape local minima. | Fitting models to very large PK/PD datasets (e.g., from dense sampling or wearable sensors). |
| RMSprop [24] | Adapts the learning rate for each parameter by dividing by a moving average of recent gradient magnitudes. | Handles non-convex problems well; adjusts to sparse gradients. | Useful for complex PK/PD models with parameters of varying sensitivity. |
| Adam [24] | Combines ideas from Momentum and RMSprop, using moving averages of both gradients and squared gradients. | Adaptive learning rates; generally robust and requires little tuning. | A popular default choice for a wide range of ML-assisted PK/PD tasks. |
| Genetic Algorithm (GA) [22] [23] | A metaheuristic that mimics natural selection, evolving a population of model candidates. | Global search; less prone to getting stuck in local minima; good for model selection. | Automated structural model and covariate model discovery in population PK/PD. |
Essential Research Reagent Solutions
| Tool / Reagent | Function in AI/ML-Enhanced PK/PD |
|---|---|
| Python/R Programming Environment | Primary languages for implementing ML algorithms (e.g., scikit-learn, TensorFlow, PyTorch) and performing statistical analysis [27]. |
| Population PK/PD Software (e.g., NONMEM, Monolix) | Industry-standard tools for nonlinear mixed-effects modeling; increasingly integrated with or guided by ML algorithms [25] [22]. |
| Genetic Algorithm Library (e.g., DEAP, GA) | Provides pre-built functions and structures for implementing genetic algorithms to search the model space [22]. |
| High-Quality, Curated PK/PD Datasets | The essential "reagent" for training and validating any ML model. Data must be reliable and representative [25] [23]. |
| Explainable AI (XAI) Toolkits (e.g., SHAP, LIME) | Software libraries used to interpret the predictions of "black box" ML models, crucial for scientific validation and regulatory submissions [25]. |
Key Algorithmic Relationships
Diagram: Genetic Algorithm Operations
The integration of artificial intelligence (AI) with mechanistic models represents a paradigm shift in computational biology and drug development. Mechanistic models describe system behavior based on underlying biological or physical principles, while AI models learn patterns directly from complex datasets. Combining these approaches merges the interpretability and causal understanding of mechanistic modeling with the predictive power and pattern recognition capabilities of AI [28]. This hybrid methodology is particularly valuable for modeling complex biological systems, estimating parameters difficult to capture experimentally, and creating surrogate models to reduce computational costs associated with expensive mechanistic simulations [28].
In pharmaceutical research and development, this integration addresses fundamental limitations of each approach used in isolation. Traditional mechanistic models often struggle with scalability and parameter estimation for highly complex systems, whereas AI models frequently lack interpretability and the ability to generalize beyond their training data [28]. The hybrid framework enables researchers to build more comprehensive and predictive models for critical biomedical applications including target identification, pharmacokinetic/pharmacodynamic (PK/PD) analysis, patient-specific dosing optimization, and disease progression modeling [28] [29].
Technical Support & Troubleshooting Guide
Frequently Asked Questions
Q1: Our hybrid model shows excellent training performance but poor generalization on validation data. What could be causing this issue?
This problem typically stems from overfitting or data mismatch. First, verify that your training and validation datasets follow similar distributions using statistical tests like Kolmogorov-Smirnov. Implement regularization techniques specifically designed for hybrid architectures, such as pathway-informed dropout where randomly selected biological pathways are disabled during training iterations. Additionally, employ cross-validation strategies that maintain temporal structure for time-series data or group structure for patient-derived data [29].
Q2: How can we effectively estimate parameters that are difficult to measure experimentally in our pharmacokinetic model?
Leverage AI-enhanced parameter estimation protocols. Train a deep neural network as a surrogate for the mechanistic model to rapidly approximate parameter likelihoods. Apply Bayesian optimization with AI-informed priors to explore the parameter space efficiently, using the mechanistic model constraints to narrow feasible regions. Transfer learning approaches can also be valuable, where parameters learned from data-rich similar systems provide initial estimates for your specific system [30].
Q3: Our integrated model has become computationally prohibitive for routine use. What optimization strategies can we implement?
Develop a surrogate modeling pipeline. Use active learning to identify the most informative regions of your parameter space, then train a lightweight AI surrogate model (such as a reduced-precision neural network) on targeted mechanistic model simulations. For real-time applications, implement model distillation to transfer knowledge from your full hybrid model to a compact architecture while preserving predictive accuracy for key outputs [28] [30].
Q4: We're experiencing inconsistencies between AI-predicted patterns and mechanistic constraints. How can we better align these components?
Implement physics-informed neural networks (PINNs) that explicitly incorporate mechanistic equations as regularization terms within the loss function. Alternatively, adopt a hierarchical approach where the mechanistic model defines the overall system architecture and conservation laws, while AI components model specific subprocesses with high uncertainty. This maintains biological plausibility while leveraging data-driven insights [30].
Q5: How can we validate that our hybrid model provides genuine biological insights rather than just data fitting?
Employ multiscale validation protocols. Test predictions at both molecular and systems levels, and use mechanistic interpretability techniques to analyze which features and circuits your AI components are leveraging. Design "knock-out" simulations where key biological mechanisms are disabled in the model and compare predictions to experimental inhibition studies. Additionally, use the model to generate novel, testable hypotheses and collaborate with experimentalists to validate these predictions [31] [32].
Common Error Messages and Solutions
Table 1: Troubleshooting Common Hybrid Modeling Issues
| Error Message/Symptom | Potential Causes | Recommended Solutions |
|---|---|---|
| Parameter identifiability warnings | High parameter correlations, insufficient data, structural non-identifiability | Apply regularization with biological constraints; redesign experiments to capture more informative data; reparameterize model to reduce correlations [29] |
| Numerical instability during integration | Stiff differential equations, inappropriate solver parameters, extreme parameter values | Switch to implicit solvers for stiff systems; implement adaptive step sizing; apply parameter boundaries based on biological feasibility [29] |
| Discrepancies between scales (e.g., molecular vs. cellular predictions) | Inadequate bridging between scales, missing emergent phenomena | Implement multiscale modeling frameworks with dedicated scale-bridging algorithms; incorporate additional biological context at interface points [28] [30] |
| Training divergence when incorporating mechanistic constraints | Conflicting gradients between data fitting and constraint terms, learning rate too high | Implement gradient clipping; use adaptive learning rate schedules; progressively increase constraint weight during training rather than fixed weighting [30] |
| Long inference times despite surrogate modeling | Inefficient model architecture, unnecessary complexity for application needs | Perform model pruning and quantization; implement early exiting for simple cases; use model cascades where simple models handle straightforward cases [30] |
Key Experimental Protocols
Protocol 1: Development of AI-Enhanced Quantitative Systems Pharmacology (QSP) Models
Objective: To construct a hybrid QSP model that integrates AI-based parameter estimation with mechanistic disease pathophysiology for optimizing clinical trial design [29].
Materials and Methods:
- Data Integration Layer: Collect and preprocess multi-scale experimental data including omics data (genomics, proteomics), clinical measurements, and literature-derived pathway information. Apply natural language processing (NLP) tools for automated literature mining to extract PK/PD parameters [29].
- Mechanistic Framework Establishment: Define the core biological structure using systems of ordinary differential equations representing key disease mechanisms, drug targets, and physiological interactions. Incorporate known biological constraints and conservation laws [29].
- AI-Hybridization:
- Train machine learning models (random forests, gradient boosting) on structural relationships to estimate difficult-to-measure parameters
- Implement neural ordinary differential equations (Neural ODEs) to model poorly characterized subsystems
- Develop surrogate models for rapid sensitivity analysis and uncertainty quantification [29]
- Validation Framework: Use k-fold cross-validation with temporal holding for time-series data. Compare predictions against experimental outcomes not used in training. Perform virtual patient simulations to assess population-level predictive performance [29].
Expected Outcomes: A validated hybrid QSP model capable of predicting patient-specific treatment responses, optimizing dosing regimens, and informing clinical trial designs with quantified uncertainty estimates.
Protocol 2: Hybrid Mechanistic-AI Approach for Chemical Process Scale-Up
Objective: To accelerate chemical process scale-up by combining molecular-level kinetic models with deep transfer learning to address reactor-specific transport phenomena [30].
Materials and Methods:
- Mechanistic Model Development: Construct a molecular-level kinetic model using laboratory-scale experimental data. For complex systems like fluid catalytic cracking, employ single-event kinetic modeling or bond-electron matrix approaches to represent fundamental reaction mechanisms [30].
- Deep Transfer Learning Architecture:
- Design a specialized network with three residual multi-layer perceptrons (ResMLPs): Process-based ResMLP for process conditions, Molecule-based ResMLP for feedstock composition, and Integrated ResMLP to predict product distribution
- Generate comprehensive training data through mechanistic model simulations across varied conditions
- Pre-train the network on laboratory-scale data (source domain)
- Implement transfer learning using limited pilot-scale data (target domain) with property-informed fine-tuning [30]
- Cross-Scale Optimization: Utilize the trained hybrid model with multi-objective optimization algorithms to identify optimal process conditions at pilot and industrial scales, balancing yield, selectivity, and economic considerations [30].
Expected Outcomes: A unified modeling framework capable of predicting product distribution across different reactor scales, significantly reducing experimental requirements for process scale-up while maintaining molecular-level predictive accuracy.
Visualization of Hybrid Modeling Approaches
Workflow for Hybrid Model Development
Hybrid Model Development Workflow
Parameter Estimation with AI Enhancement
AI-Enhanced Parameter Estimation Process
Research Reagent Solutions
Table 2: Essential Computational Tools for Hybrid Mechanistic-AI Research
| Tool/Category | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Mechanistic Modeling Platforms | MATLAB SimBiology, COPASI, DBSolve, GNU MCSim | Solve systems of differential equations; parameter estimation; sensitivity analysis | Building quantitative systems pharmacology (QSP) models; pharmacokinetic/pharmacodynamic modeling [29] |
| AI/ML Frameworks | PyTorch, TensorFlow, JAX, Scikit-learn | Implement neural networks; deep learning; standard machine learning algorithms | Developing surrogate models; parameter estimation; pattern recognition in complex data [33] [30] |
| Hybrid Modeling Specialized Tools | Neural ODEs, Physics-Informed Neural Networks (PINNs), TensorFlow Probability | Integrate differential equations with neural networks; incorporate physical constraints | Creating hybrid architectures where AI learns unknown terms in mechanistic models [30] |
| Transfer Learning Libraries | Hugging Face Transformers, TLlib, Keras Tuner | Adapt pre-trained models to new domains with limited data | Cross-scale modeling; adapting models from laboratory to industrial scale [30] |
| Optimization & Parameter Estimation | Bayesian optimization tools (BoTorch, Scipy), Markov Chain Monte Carlo (PyMC3, Stan) | Efficient parameter space exploration; uncertainty quantification | Parameter estimation for complex models; design of experiments [29] [30] |
| Data Mining & Curation | NLP tools (spaCy, NLTK), automated literature mining pipelines | Extract and structure knowledge from scientific literature | Populating model parameters; building prior distributions; validating biological mechanisms [29] |
| Visualization & Interpretation | TensorBoard, Plotly, Matplotlib, mechanistic interpretability tools | Model debugging; feature visualization; results communication | Understanding AI component behavior; explaining model predictions [31] [32] |
Advanced Implementation Considerations
Addressing Scale Discrepancies in Multi-Source Data
A significant challenge in hybrid modeling is reconciling data from different scales and resolutions. Laboratory-scale data often includes detailed molecular-level characterization, while pilot and industrial-scale systems typically provide only bulk property measurements [30]. Implement property-informed transfer learning by integrating mechanistic equations for calculating bulk properties directly into neural network architectures. This approach bridges the data gap between scales by enabling the model to learn from molecular-level laboratory data while predicting bulk properties relevant to larger scales [30].
For cross-scale parameter estimation, develop multi-fidelity modeling strategies that combine high-fidelity experimental data with larger volumes of lower-fidelity simulation data. Use adaptive sampling techniques to strategically allocate computational resources between mechanistic simulations and AI training, maximizing information gain while minimizing computational expense [30].
Interpretability and Validation Frameworks
As hybrid models grow in complexity, maintaining interpretability becomes increasingly important, particularly for regulatory acceptance in drug development [31] [32]. Implement mechanistic interpretability techniques to analyze how AI components process information, including:
- Activation Patching: Systematically replace activations in the network to identify causal relationships between components and predictions [31]
- Circuit Analysis: Identify subnetworks responsible for specific computational functions within larger AI architectures [31] [32]
- Feature Visualization: Understand what input patterns maximally activate different components of the hybrid model [32]
Develop comprehensive validation protocols that test both quantitative prediction accuracy and qualitative biological plausibility. Include "stress tests" where the model is evaluated under extreme conditions not represented in training data, assessing whether it maintains physiologically reasonable behavior. For regulatory applications, document both the model development process and the final model architecture, as the process itself provides valuable insights into system behavior [29].
The Hierarchically Self-adaptive Particle Swarm Optimization - Stacked AutoEncoder (HSAPSO-SAE) framework is a novel deep learning approach designed to overcome critical limitations in drug discovery, such as overfitting, computational inefficiency, and limited scalability of traditional models like Support Vector Machines and XGBoost [10]. By integrating a Stacked Autoencoder for robust feature extraction with an advanced PSO variant for hyperparameter tuning, this framework achieves superior performance in drug classification and target identification tasks [10].
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of using HSAPSO over standard optimization algorithms for tuning the SAE? The primary advantage lies in its hierarchically self-adaptive nature. Unlike standard PSO or other static optimization methods, HSAPSO dynamically balances exploration and exploitation during the training process. It adaptively tunes the hyperparameters of the SAE, such as the number of layers, nodes per layer, and learning rate, which leads to faster convergence, greater resilience to variability, and significantly reduces the risk of converging to suboptimal local minima [10].
Q2: My model is achieving high training accuracy but poor validation accuracy. What could be the cause and how can HSAPSO-SAE address this? This is a classic sign of overfitting. The HSAPSO-SAE framework is specifically designed to mitigate this issue through two key mechanisms. First, the SAE component performs hierarchical feature learning, which helps to learn more generalizable and abstract representations from the input data. Second, the HSAPSO algorithm optimizes the model's hyperparameters to ensure a good trade-off between model complexity and generalization capability, thereby enhancing performance on unseen validation and test datasets [10].
Q3: What are the computational performance benchmarks for the HSAPSO-SAE framework? Experimental evaluations on benchmark datasets like DrugBank and Swiss-Prot have demonstrated that the framework achieves a high accuracy of 95.52%. Furthermore, it exhibits low computational complexity, requiring only 0.010 seconds per sample, and shows exceptional stability with a standard deviation of ±0.003 [10]. This makes it suitable for large-scale pharmaceutical datasets.
Q4: Which datasets were used to validate the HSAPSO-SAE framework, and where can I find them? The framework was validated on real-world pharmaceutical datasets, primarily sourced from DrugBank and Swiss-Prot [10]. These repositories provide comprehensive data on drugs, protein targets, and their interactions, which are standard for benchmarking in computational drug discovery. You can access these databases through their official websites.
Troubleshooting Guides
Issue 1: Slow Convergence or Failure to Converge During Training
- Potential Cause: Poorly chosen initial ranges (search space) for the hyperparameters being optimized by HSAPSO.
Solution:
- Conduct a preliminary sensitivity analysis to understand the impact of individual hyperparameters on your model's performance. This helps in defining a more effective and bounded search space [34].
- Consider initializing the HSAPSO swarm with values derived from simpler optimization methods like Random Search, which can provide a good starting point for the more refined HSAPSO algorithm [35].
Potential Cause: Inadequate configuration of the HSAPSO's own parameters (e.g., swarm size, inertia weight).
- Solution: Refer to the foundational literature on the HSAPSO-SAE framework for recommended initial settings [10]. The hierarchical and self-adaptive properties of the algorithm should help, but may require calibration for a new problem domain.
Issue 2: Poor Overall Model Performance (Low Accuracy)
- Potential Cause: The quality of the input feature data is low, or the data contains a significant number of missing values.
Solution: Implement rigorous data preprocessing. For the HSAPSO-SAE framework, this includes:
- Handling Missing Values: Use robust imputation techniques such as MICE (Multivariable Imputation by Chained Equations), k-Nearest Neighbor (kNN) imputation, or Random Forest (RF) imputation, as these have been shown to be effective for clinical and pharmaceutical datasets [35].
- Data Normalization: Apply standardization (e.g., z-score normalization) to continuous features to ensure all features are on a comparable scale [35]. The formula is ( z = \frac{x - \mu}{\sigma} ), where ( x ) is the original value, ( \mu ) is the feature mean, and ( \sigma ) is its standard deviation.
Potential Cause: The architecture of the Stacked Autoencoder is not complex enough to capture the intricacies of your data.
- Solution: Allow the HSAPSO algorithm to search over a larger space of architectural hyperparameters, such as a greater number of hidden layers and a higher number of nodes per layer. The optimization process is designed to find an optimal balance between complexity and performance [10].
Issue 3: Model Performance is Highly Variable Across Different Runs
- Potential Cause: High variance inherent in the training process or optimization algorithm.
- Solution: Implement k-fold cross-validation (e.g., 10-fold cross-validation) to ensure the model's performance is robust and not dependent on a particular split of the data. This technique was used in the original study to validate the framework's stability [10] [35].
Experimental Performance Data
The following table summarizes the key quantitative results from the evaluation of the HSAPSO-SAE framework as reported in the scientific literature [10].
Table 1: Key Performance Metrics of the HSAPSO-SAE Framework
| Metric | Reported Value | Notes / Comparative Context |
|---|---|---|
| Classification Accuracy | 95.52% | Achieved on DrugBank and Swiss-Prot datasets. |
| Computational Speed | 0.010 seconds/sample | Demonstrates high efficiency for large-scale data. |
| Stability (Std. Deviation) | ± 0.003 | Indicates highly consistent and reliable performance. |
| Comparative Performance | Outperformed SVM, XGBoost, and other deep learning models. | Noted for higher accuracy and faster convergence [10]. |
Experimental Protocol: Reproducing HSAPSO-SAE for Drug Target Identification
This section provides a detailed methodology for replicating a key experiment involving the HSAPSO-SAE framework, based on the procedures described in its foundational study [10].
1. Objective To train and evaluate the HSAPSO-SAE framework for the task of druggable protein target identification, achieving high classification accuracy and computational efficiency.
2. Dataset Preparation
- Data Source: Curate a dataset from DrugBank and Swiss-Prot databases. The dataset should include known drug-target pairs and non-interacting pairs for a binary classification task.
- Feature Representation: Represent each protein target using a set of 443 features, which may include sequence-derived descriptors, physicochemical properties, and structural features, as utilized in prior related work [10].
- Data Preprocessing:
- Imputation: Apply the MICE imputation technique to handle missing values in the feature set [35].
- Normalization: Standardize all continuous features using z-score normalization to have a mean of 0 and a standard deviation of 1 [35].
- Data Splitting: Split the dataset into training, validation, and test sets (e.g., 70/15/15).
3. Model Configuration and Workflow The following diagram illustrates the core experimental workflow.
4. Hyperparameter Optimization with HSAPSO
- Algorithm: Configure the Hierarchically Self-adaptive PSO algorithm. The "hierarchically self-adaptive" component means the algorithm's parameters (like inertia) automatically adjust during the optimization process.
- Search Space: Define the hyperparameter search space for the SAE. This typically includes:
- Number of hidden layers and number of nodes per layer.
- Learning rate and optimizer choices.
- Regularization parameters (e.g., L1/L2 penalty).
- Activation functions.
- Objective Function: The objective for HSAPSO is to maximize classification accuracy (or minimize loss) on the validation set.
5. Evaluation
- Metrics: Evaluate the final optimized model (optSAE) on the held-out test set. Report standard classification metrics: Accuracy, Sensitivity, Specificity, and Area Under the Curve (AUC).
- Benchmarking: Compare the performance of HSAPSO-SAE against state-of-the-art methods mentioned in the study, such as standard SVM, XGBoost, and other deep learning models, to demonstrate its superior performance [10].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists the essential computational "reagents" and tools required to implement the HSAPSO-SAE framework.
Table 2: Essential Research Reagents and Computational Tools
| Item / Resource | Function in the Experiment | Notes |
|---|---|---|
| DrugBank Database | Provides curated data on drug molecules, their mechanisms, and protein targets. | Primary source for building the classification dataset [10]. |
| Swiss-Prot Database | Provides high-quality, manually annotated protein sequence data. | Source for protein feature extraction and target identification [10]. |
| Stacked Autoencoder (SAE) | Performs unsupervised pre-training and hierarchical feature extraction from high-dimensional input data. | Core component for learning robust latent representations [10]. |
| Particle Swarm Optimization (PSO) | A population-based stochastic optimization algorithm. | Base algorithm that is enhanced to create HSAPSO [10]. |
| Hierarchically Self-adaptive PSO (HSAPSO) | Automatically and dynamically tunes the hyperparameters of the SAE for optimal performance. | The key innovation that drives the framework's efficiency and accuracy [10]. |
| MICE Imputation | Handles missing data points in the feature set by creating multiple plausible imputations. | Critical for maintaining data integrity with real-world, often incomplete, datasets [35]. |
Troubleshooting Guides and FAQs
This section addresses common challenges researchers face when applying optimization algorithms to key stages of drug development.
ADMET Prediction
Q: Our QSAR model shows high predictive accuracy in cross-validation but performs poorly on new, external chemical series. What could be the cause and how can we resolve this?
- Problem: This typically indicates model overfitting or a lack of domain applicability, where the training data does not adequately represent the chemical space of the new compounds.
- Troubleshooting Steps:
- Assess Applicability Domain: Use distance-based methods (e.g., leverage, Euclidean distance) or range-based methods to verify that new compounds fall within the chemical space of the training set. Compounds outside this domain require extrapolation and predictions are unreliable.
- Evaluate Data Quality and Diversity: Audit the training data for biases, structural redundancies, or limited scaffold diversity. Incorporate more diverse chemical structures that better represent the project's chemical space.
- Simplify the Model: Reduce model complexity by using feature selection algorithms to eliminate non-predictive descriptors. This can decrease variance and improve generalizability.
- Implement Ensemble Methods: Switch from a single model to an ensemble approach (e.g., Random Forest, Gradient Boosting) that combines multiple models to improve robustness on new data.
Q: How can we optimize ADMET properties for a lead compound without compromising its primary pharmacological activity?
- Problem: This is a classic multi-objective optimization challenge in medicinal chemistry, where improving one property (e.g., metabolic stability) can detrimentally affect another (e.g., potency).
- Troubleshooting Steps:
- Systematic SAR Exploration: Structure-Activity Relationship (SAR) studies are crucial. Methodically synthesize and test analogs to identify regions of the molecule that can be modified to improve ADMET properties while maintaining core interactions with the biological target [36].
- Utilize Predictive Tools: Leverage in silico models (PBPK, QSP) early to predict the outcomes of structural changes on absorption, distribution, and metabolism before committing to synthesis [3].
- Apply Multi-Parameter Optimization (MPO): Implement scoring functions or algorithms that balance multiple criteria (e.g., potency, solubility, lipophilicity) to prioritize compounds with the best overall profile [36] [37].
- Consider Prodrug Strategies: If direct optimization fails, explore prodrug approaches. A prodrug is a chemically modified, inactive version of the lead compound designed to improve a specific ADMET property (like absorption), which then converts to the active drug within the body [36].
Lead Compound Optimization
Q: During the Design-Make-Test-Analyze (DMTA) cycle, how should we prioritize which compound analogs to synthesize next from a large virtual library?
- Problem: The bottleneck between ideation and synthetic throughput necessitates a strategic compound prioritization process [37].
- Troubleshooting Steps:
- Define a Clear Scoring Strategy: Move beyond single-parameter ranking (e.g., potency). Use Multi-Criteria Decision Analysis (MCDA) to create a weighted score based on project goals, incorporating predicted activity, ADMET properties, and synthetic feasibility [37].
- Implement Active Learning: Use machine learning models that can query the most informative compounds for synthesis. This strategy helps explore the chemical space more efficiently and identifies optimal compounds in fewer DMTA cycles [37].
- Balance Exploration and Exploitation: Allocate a portion of synthetic effort to exploring new, uncertain chemical regions (exploration) while also refining the most promising existing scaffolds (exploitation).
- Benchmark Strategies Retrospectively: Replay historical project data to evaluate how different prioritization strategies would have performed, providing a low-cost test bed for selecting the best approach for your current project [37].
Q: Our lead compound shows promising in vitro activity but poor solubility, leading to low bioavailability in animal models. What optimization strategies can we employ?
- Problem: Poor aqueous solubility is a frequent hurdle that limits a drug's absorption and exposure in the body.
- Troubleshooting Steps:
- Modify Lipophilicity: Adjust the compound's partition coefficient (LogP) by introducing ionizable groups, hydrogen bond donors/acceptors, or reducing hydrophobic surface area. This is a primary medicinal chemistry approach [36].
- Salt and Cocrystal Screening: If the compound has ionizable groups, form pharmaceutically acceptable salts. For neutral compounds, explore cocrystals with coformers to improve solubility and dissolution rate.
- Employ Formulation Strategies: In parallel to chemical modification, collaborate with formulation scientists. Techniques like amorphization, nanoparticles, or the use of solubilizing agents (e.g., cyclodextrins) can rescue compounds with intrinsic solubility challenges [36].
- Apply the "Rule of Five" (Lipinski's Rules): Check if the compound violates multiple rules related to molecular weight, lipophilicity, and hydrogen bonding, which are predictive of solubility and permeability issues.
Clinical Trial Simulation
Q: Our clinical trial simulation for an adaptive design shows unacceptable operational characteristics under certain scenarios. How can we refine the design before submitting the protocol?
- Problem: This indicates that the initial design is not robust enough to handle plausible real-world uncertainties, such as variable treatment effects or patient enrollment rates [38].
- Troubleshooting Steps:
- Stress-Test with Expanded Scenarios: Develop a wider range of simulation scenarios, including challenging "edge cases" (e.g., smaller treatment effects, unexpected toxicity, or regional enrollment disparities). This helps identify the design's breaking points [38].
- Iterative Refinement and Comparison: Use simulation as an iterative design tool. Adjust key parameters (e.g., sample size, randomization ratios, interim analysis timing, futility thresholds) and compare the operating characteristics of the new design variants against the original [38].
- Leverage Specialized Software: Utilize advanced simulation platforms (e.g., FACTS) that are specifically designed to configure complex adaptive elements, run simulations rapidly, and compare multiple candidate designs within a unified framework [38].
- Engage Stakeholders Early: Walk clinicians, statisticians, and operational staff through example simulation runs. This builds mutual understanding and incorporates diverse feedback to create a more robust and widely-supported final design [38].
Q: How can we use optimization to determine the optimal sample size and interim analysis plan for a Phase II dose-finding study?
- Problem: The goal is to balance statistical power, type I error control, resource efficiency, and the probability of correctly selecting the most effective dose.
- Troubleshooting Steps:
- Define a Quantitative Objective Function: The optimization algorithm requires a clear goal. This could be maximizing the probability of correctly selecting a dose with a meaningful treatment effect, minimizing the expected sample size under the null hypothesis, or minimizing the cost while maintaining a target power.
- Simulate Key Scenarios: Model the trial's performance under a null scenario (all doses ineffective), a desired alternative (one or more doses effective), and other plausible dose-response shapes (e.g., linear, umbrella) [38].
- Optimize Design Parameters: Use the simulation engine to systematically evaluate different combinations of sample size per arm, number and timing of interim analyses, and dose-dropping rules. The output is the set of parameters that best satisfies the objective function while controlling for statistical errors [38].
- Incorporate Bayesian Methods: Consider Bayesian adaptive designs, which are naturally suited for this task. Techniques like response-adaptive randomization can automatically shift more patients to better-performing arms during the trial, optimizing resource allocation and potentially yielding a more ethical design [38].
Detailed Experimental Protocols
Protocol 1: Retrospective Benchmarking of Compound Prioritization Strategies
This methodology replays historical project data to evaluate the performance of different optimization algorithms for compound prioritization in lead optimization [37].
1. Objective To quantitatively compare the performance of various compound selection strategies (e.g., Active Learning, MCDA, medicinal chemistry heuristics) in a simulated DMTA cycle environment.
2. Materials and Data Requirements
- Datasets: Historical project data containing, for each synthesized compound: chemical structure (SMILES), assay results (e.g., IC50, solubility), ADMET endpoints, and a timestamp for each DMTA cycle [37].
- Software: A computational framework capable of handling chemical data and implementing selection strategies (e.g., Python with RDKit and scikit-learn).
3. Procedure
- Step 1: Data Preprocessing. Curate the historical dataset, ensuring data quality and aligning all data to consistent DMTA rounds.
- Step 2: Strategy Implementation. Define and code the selection algorithms to be benchmarked.
- Step 3: Simulation Loop. For each DMTA round in the historical data, simulate the selection process.
- Step 4: Performance Metrics Calculation. After the simulation, calculate key performance indicators (KPIs) for each strategy.
Table: Key Performance Indicators for Benchmarking
| Metric | Description | Interpretation |
|---|---|---|
| Cumulative Compound Quality | The sum of a weighted desirability score for all compounds selected by the strategy over time. | Measures the strategy's efficiency in selecting high-quality compounds. |
| Number of Rounds to Identify Lead | The number of DMTA cycles required to identify a compound meeting pre-defined lead criteria. | Measures the speed of the optimization process. |
| Chemical Space Exploration | The diversity of the selected compounds, measured by molecular fingerprints (e.g., Tanimoto similarity). | Assesses whether the strategy explores new areas or gets stuck exploiting a single region. |
4. Analysis Compare the KPIs across the different selection strategies. The optimal strategy is context-dependent but is generally the one that identifies the best compounds in the fewest rounds while maintaining a reasonable level of exploration.
Protocol 2: Optimization of Clinical Trial Design via Simulation
This protocol uses clinical trial simulation as an engine to optimize adaptive trial designs before a single patient is enrolled [38].
1. Objective To develop and stress-test a clinical trial design, optimizing its parameters (e.g., sample size, interim analysis rules) to ensure robust performance across a wide range of plausible future scenarios.
2. Materials and Software
- Software Platform: A specialized clinical trial simulation tool (e.g., FACTS, R/shiny applications) [38].
- Statistical Model: A model for generating synthetic patient data (e.g., a model for the primary endpoint, dropout rates, biomarker prevalence).
3. Procedure
- Step 1: Scenario Development. Collaboratively define a set of scenarios with stakeholders. These should include:
- Primary Alternative: The expected or desired treatment effect.
- Null Scenario: A scenario with no treatment effect to assess type I error.
- Challenging Scenarios: Smaller effect sizes, different accrual rates, or subgroup effects.
- Step 2: Design Candidate Specification. Define one or more candidate trial designs to simulate. For an adaptive dose-finding study, this includes the number of arms, initial randomization ratio, timing of interim analyses, and rules for dropping inferior arms.
- Step 3: Large-Scale Simulation. Run thousands of virtual trials for each candidate design and each scenario. For each virtual trial, the software will:
- Emulate patient enrollment, randomization, and endpoint generation.
- Apply the adaptive rules at interim looks (e.g., drop arms for futility).
- Record the final outcome (e.g., which dose was selected, whether the trial was successful).
- Step 4: Analysis of Operating Characteristics. Aggregate the results from all simulation runs to calculate the design's performance.
Table: Key Operating Characteristics for Clinical Trial Optimization
| Characteristic | Description | Target |
|---|---|---|
| Power | Probability of correctly identifying an effective treatment under the alternative scenario. | Maximize (e.g., >80-90%) |
| Type I Error | Probability of falsely claiming success under the null scenario. | Control (e.g., ≤5%) |
| Sample Size Distribution | The range and distribution of the number of patients required. | Understand and minimize where possible |
| Probability of Correct Selection | The likelihood of selecting the truly best dose. | Maximize |
4. Optimization and Refinement Compare the operating characteristics of different candidate designs. Iteratively adjust the design parameters (e.g., futility threshold, final sample size) and re-simulate until a design is found that meets the desired performance targets across the key scenarios.
Workflow and Pathway Diagrams
Lead Optimization DMTA Cycle
Clinical Trial Simulation for Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Computational Tools for Optimization in Drug Development
| Tool / Solution | Function in Optimization | Application Context |
|---|---|---|
| QSAR Models | Predicts biological activity and ADMET properties from chemical structure, enabling virtual screening of compounds before synthesis. | ADMET Prediction, Lead Optimization [3] |
| PBPK Models | Mechanistically simulates a drug's absorption, distribution, metabolism, and excretion in a virtual human body. Used to predict human PK and DDI risk. | ADMET Prediction, First-in-Human Dosing [3] |
| Active Learning Algorithms | AI/ML techniques that select the most informative compounds for the next testing cycle, optimizing the exploration of chemical space. | Lead Optimization (Compound Prioritization) [37] |
| Multi-Criteria Decision Analysis (MCDA) | Provides a framework to rank compounds based on a weighted score of multiple properties (e.g., potency, solubility, synthetic cost). | Lead Optimization (Compound Prioritization) [36] [37] |
| Clinical Trial Simulation Software (e.g., FACTS) | A platform for virtually running clinical trials under many scenarios to optimize adaptive design rules, sample size, and power before study start. | Clinical Trial Simulation [38] |
| Quantitative Systems Pharmacology (QSP) | Integrates disease biology and drug mechanisms to predict clinical efficacy and optimize trial design for specific patient populations. | Clinical Trial Simulation, Dose Optimization [3] |
Overcoming Implementation Hurdles: Strategies for Robust and Efficient Parameter Estimation
Troubleshooting Guides
1. Guide: Mitigating the Impact of Sparse Interior Data in PDE Parameter Identification
- Problem Statement: Parameter identification for complex physical systems governed by Partial Differential Equations (PDEs) fails or yields high errors when available measurement data is sparse in the interior domain [39].
- Diagnosis: Traditional Physics-Informed Neural Networks (PINNs) often experience a significant performance decline when interior data is sparse, as the physical constraints alone are insufficient for accurate parameter estimation [39].
- Solution: Implement a recurrent neural network architecture combined with an implicit numerical method [39].
- Step 1: Use a neural network (e.g., Gated Recurrent Unit - GRU) to produce an initial solution approximation over the entire spatio-temporal domain [39].
- Step 2: Employ an implicit numerical time-stepping scheme (like Adams-Moulton) based on the network's initial approximation. The unknown PDE parameters are initially assigned random values [39].
- Step 3: Construct a loss function that integrates two components [39]:
- The mean square error between the neural network's predictions and the solutions generated by the numerical iteration scheme.
- The mean square error between the network's predictions and the actual sparse interior measurement data.
- Step 4: Simultaneously identify the unknown PDE parameters (denoted as (\varvec{\tau})) and reconstruct the complete solution by minimizing this combined loss function [39].
2. Guide: Parameter Estimation for MIMO Systems with Outliers and Colored Noise
- Problem Statement: Parameter estimation for Multi-Input Multi-Output (MIMO) systems becomes inaccurate due to interference from outliers and colored (non-white) noise, which is common in real industrial processes [40].
- Diagnosis: Traditional identification methods like least squares, which focus on minimizing empirical risk, are prone to overfitting and perform poorly under such non-ideal noise conditions [40].
- Solution: Apply a Support Vector Regression (SVR) based algorithm, enhanced with optimization techniques for speed [40].
- Step 1: For a MIMO system described by a Transfer Function Matrix (TFM), first estimate the parameters of an equivalent difference equation model [40].
- Step 2: Use the (\epsilon)-SVR algorithm to perform the parameter estimation. SVR introduces an (\epsilon)-insensitive loss function that provides a tolerance margin for fitting, making it robust to outliers and noise [40].
- Step 3: To address the long computation time of SVR, integrate optimization methods like Random Search and Bayesian Optimization (RSBO-SVR) to rapidly find the optimal hyperparameters for the SVR model [40].
- Step 4: Derive the final parameters of the original TFM from the identified difference equation model [40].
Frequently Asked Questions
Q1: What strategies exist for signal-dependent noise parameter estimation from a single image? A1: A common approach is based on selecting "weakly textured" image blocks where noise is more apparent than actual image content. The key challenge is accurately identifying these blocks. One advanced method uses a clustering algorithm called Adaptively Relative Density Peak Clustering (ARDPC) [41].
- Methodology: The image is divided into small, overlapping blocks. Multiple features (e.g., based on gradients, histograms) are extracted from each block. The ARDPC algorithm then clusters these blocks based on their features, automatically identifying the cluster corresponding to weakly textured regions without needing an empirically set threshold. Finally, noise parameters are estimated by fitting a signal-dependent noise model using the pixel intensities and computed variances from the selected weak-texture blocks [41].
Q2: How can I estimate parameters in nonlinear ODEs from low-quality, noisy time-series data? A2: A framework using the Picard iteration has been proposed for this purpose. It is designed for data that is noisy, sparse, irregularly sampled, and where the system state or its derivative is not directly measured [42].
- Methodology: The approach reformulates the parameter estimation problem as a constrained optimization problem in an infinite-dimensional space using the Picard operator. It then leverages the contractive properties of this operator to create gradient-based algorithms that are provably convergent to a local optimum under certain conditions, demonstrating robustness across various models and datasets [42].
Q3: What is a systematic method for diagnosing and solving data-related problems in computational experiments? A3: Applying the scientific method provides a structured framework for problem-solving in IT and data analysis [43].
- Identify and Analyze the Problem: Translate the symptom into a focused, researchable question.
- Form a Hypothesis: Propose an educated, measurable proposition for a solution.
- Conduct Experiments: Design and run objective tests to prove or disprove the hypothesis.
- Analyze Data: Determine if the data confirms the hypothesis and identify any new issues.
- Conclude on the Results: Document findings and iterate if necessary [43].
Experimental Protocols & Data
Table 1: Performance of Denoising and Parameter Estimation Algorithms
| Algorithm / Method | Application Context | Key Performance Metric | Result | Source |
|---|---|---|---|---|
| ARDPC for Noise Estimation | Image denoising (Signal-dependent noise) | Accuracy in selecting weak-texture blocks | Improved accuracy over gradient/histogram-based methods | [41] |
| RSBO-SVR | MIMO System Identification (Colored noise & outliers) | Maximum Relative Error | ≤ 4% in simulation and tank experiment | [40] |
| RSBO-SVR | MIMO System Identification (Colored noise & outliers) | Runtime Reduction vs. standard SVR | Up to 99.38% reduction | [40] |
| GRU with Implicit Numerical Method | PDE Parameter Identification (Sparse interior data) | Reconstruction error in Burgers', Allen-Cahn equations | Accurate parameter identification and full solution recovery | [39] |
Table 2: Research Reagent Solutions: Key Computational Tools
| Item / Tool | Function in Research | Example Context / Use Case |
|---|---|---|
| Support Vector Regression (SVR) | A robust regression algorithm that minimizes a loss function with a tolerance margin ((\epsilon)), making it resistant to outliers and noise. | Estimating parameters of MIMO systems disturbed by colored noise and outliers [40]. |
| Physics-Informed Neural Networks (PINNs) | Neural networks that embed the residual of governing physical laws (e.g., PDEs) directly into the loss function to solve forward and inverse problems. | Solving PDE parameter identification problems; performance can decline with very sparse data [39]. |
| Gated Recurrent Unit (GRU) | A type of recurrent neural network (RNN) with gating mechanisms to better capture long-range dependencies in sequential data. | Approximating solutions for time-dependent PDEs and aiding in parameter estimation [39]. |
| Adaptively Relative Density Peak Clustering (ARDPC) | A clustering algorithm that identifies cluster centers in datasets with uneven density distribution without requiring empirically set parameters. | Automatically selecting weakly textured image blocks for single-image noise parameter estimation [41]. |
| Picard Iteration | An iterative method used to reformulate ODE problems into integral equations, facilitating the proof of existence and uniqueness of solutions. | A framework for gradient-based parameter estimation in nonlinear ODEs with low-quality data [42]. |
Workflow and System Diagrams
Workflow for PDE parameter identification with sparse data
Parameter estimation process for noisy MIMO systems
Mitigating Overfitting and Ensuring Generalization in Complex AI/ML Models
Troubleshooting Guide: Diagnosing and Resolving Overfitting
How do I know if my model is overfitting?
A model is likely overfitting when you observe a large performance gap: it has high accuracy (low error) on the training data but significantly lower accuracy (high error) on a separate validation or test dataset [44] [45] [46]. This indicates the model has memorized the training data instead of learning generalizable patterns. In drug discovery contexts, this might manifest as a model that performs perfectly on known molecular structures but fails to predict the activity of novel compounds [10].
Primary Indicators:
- Training accuracy is very high (e.g., >95%) while validation accuracy is substantially lower [46].
- The model's performance on a hold-out test set is poor, even after excellent training performance [45].
- The learned function, if visualized, would be overly complex and would pass through every data point in the training set, including outliers [46].
What is the difference between overfitting and underfitting?
The following table contrasts the key characteristics of overfitting and underfitting, which represent two ends of the model performance spectrum.
| Feature | Underfitting | Overfitting |
|---|---|---|
| Performance | Poor on both training and test data [44] [47] | Excellent on training data, poor on test data [44] [45] |
| Model Complexity | Too simple for the data [44] [46] | Too complex for the data [44] [46] |
| Bias/Variance | High bias, low variance [44] [45] | Low bias, high variance [44] [45] |
| Analogy | Only knows chapter titles; lacks depth [44] | Memorized the entire textbook, including typos [44] |
What are the most effective techniques to fix overfitting?
The table below summarizes established and advanced techniques for mitigating overfitting, along with their primary mechanisms and application contexts.
| Technique | Primary Mechanism | Common Application Context |
|---|---|---|
| Gather More Data [44] [47] | Provides a clearer signal of the true underlying pattern, making noise harder to memorize. | All models, when feasible. |
| Regularization (L1/L2) [44] [45] | Applies a penalty to the model's complexity, forcing weights to be small. | Linear models, neural networks. |
| Dropout [44] [48] | Randomly ignores neurons during training, preventing over-reliance on any single node. | Neural networks. |
| Early Stopping [44] [45] | Halts training when validation performance stops improving. | Iterative models (e.g., neural networks, boosting). |
| Ensemble Methods (Bagging) [48] [47] | Combines multiple models to average out their errors and reduce variance. | Decision trees (e.g., Random Forests), other base models. |
| Information-Corrected Estimation (ICE) [49] | Directly maximizes a corrected likelihood to reduce generalization error, an alternative to L2. | Model estimation within supervised learning. |
A Drug Discovery Case Study: The optSAE + HSAPSO Framework
In pharmaceutical research, overfitting is a critical concern that can lead to costly failures in later stages of drug development. A novel framework termed optSAE + HSAPSO has been proposed to address this, integrating a Stacked Autoencoder (SAE) for robust feature extraction with a Hierarchically Self-Adaptive Particle Swarm Optimization (HSAPSO) algorithm for adaptive parameter tuning [10].
Experimental Protocol and Workflow:
- Data Preprocessing: Curated datasets from DrugBank and Swiss-Prot are rigorously preprocessed to ensure input data quality [10].
- Feature Extraction: A Stacked Autoencoder (SAE) learns hierarchical and latent representations from the raw, high-dimensional pharmaceutical data (e.g., molecular descriptors, protein sequences) [10].
- Hyperparameter Optimization: The HSAPSO algorithm dynamically optimizes the hyperparameters of the SAE. It adaptively balances exploration and exploitation, leading to faster convergence and avoidance of suboptimal solutions compared to traditional methods [10].
- Classification & Validation: The optimized model performs classification tasks (e.g., target identification). Its performance is rigorously evaluated on validation and unseen test sets using metrics like accuracy, ROC analysis, and convergence behavior [10].
Quantitative Results: The following table summarizes the key performance metrics reported for the optSAE + HSAPSO framework in its study.
| Metric | Reported Performance |
|---|---|
| Classification Accuracy | 95.52% [10] |
| Computational Speed | 0.010 seconds per sample [10] |
| Stability (Variability) | ± 0.003 [10] |
Diagram 1: The optSAE + HSAPSO framework combines feature learning and adaptive optimization.
The Scientist's Toolkit: Key Research Reagents & Solutions
The following table lists essential computational "reagents" and their functions for building robust, generalizable models in drug discovery.
| Item | Function in the "Experiment" |
|---|---|
| Stacked Autoencoder (SAE) | A deep learning model that compresses input data (e.g., molecular structures) into a lower-dimensional, meaningful representation and then reconstructs it, effectively learning the most salient features [10]. |
| Particle Swarm Optimization (PSO) | An evolutionary optimization algorithm that searches for optimal parameters (e.g., hyperparameters) by simulating the social behavior of a bird flock, balancing global and local search [10]. |
| K-fold Cross-Validation | A resampling procedure used to evaluate a model by partitioning the data into 'k' subsets, repeatedly training on k-1 folds and validating on the held-out fold. This provides a robust estimate of generalization error [44] [45]. |
| Information-Corrected Estimation (ICE) | An objective function that aims to directly maximize a corrected likelihood as an estimator of KL divergence, proven to reduce generalization error compared to maximum likelihood estimation [49]. |
| Regularization (L1/L2) | A family of techniques that impose a penalty on the magnitude of model coefficients to prevent them from becoming too large, thereby simplifying the model and reducing overfitting [44] [47]. |
| Ensemble Methods (e.g., Random Forest) | Methods that combine the predictions of multiple base models (e.g., decision trees) to produce a single, more robust and accurate prediction, reducing variance and overfitting [48] [47]. |
Advanced Topic: Beyond Traditional Bias-Variance
Classical theory suggests that as model complexity increases, test error should eventually rise monotonically due to overfitting. However, modern over-parameterized models like deep neural networks challenge this view. The "double descent" risk curve has been observed, where test error descends a second time as model complexity grows past the point of exactly interpolating (fitting perfectly) the training data [45]. This underscores that traditional mitigation strategies like early stopping might sometimes prevent achieving the highest possible performance.
Furthermore, the concept of "epiplexity" has been proposed as a new measure that accounts for the structural information accessible to computationally bounded observers, offering a fresh framework to explain generalization in complex models [50].
Frequently Asked Questions (FAQs)
What is the simplest first step to try if I suspect overfitting?
The most direct initial step is to collect more high-quality, representative training data [44] [47]. A larger dataset provides a clearer signal of the true underlying pattern, making it harder for the model to memorize noise. In drug discovery, this means ensuring your training set encompasses a diverse and broad range of molecular structures and target classes [10].
Can a model be both overfit and underfit?
Not simultaneously for a given state, but a model can oscillate between these states during the training process. This is why continuously monitoring performance on a validation set is crucial [46]. You might start with an underfit model (high training error), which then learns and improves, but if training continues unchecked, it can become overfit (low training error, high validation error).
Why does dropout prevent overfitting?
Dropout is a regularization technique that, during training, randomly "drops out" (temporarily removes) a random subset of neurons in a layer [44] [48]. This prevents the network from becoming too dependent on any single neuron or co-adaptation of neurons, forcing it to learn more robust and distributed features that generalize better to new data [46].
Is some degree of overfitting always bad?
While significant overfitting is detrimental as it cripples a model's predictive power on new data, a small degree of overfitting might be acceptable in some applications. However, any overfitting generally indicates that the model is not learning the underlying pattern as well as it could, and thus its performance on real-world data is suboptimal and potentially unreliable [46].
How does the ICE estimator differ from L2 regularization?
While both aim to improve generalization, L2 regularization works by adding a penalty term based on the squared magnitude of the parameters to the loss function [44]. The Information-Corrected Estimation (ICE), in contrast, attempts to directly maximize a corrected likelihood function as an estimator of the KL divergence. It is theoretically proven to reduce generalization error and can be effective for a wider class of models where L2 regularization may fail [49].
Diagram 2: A diagnostic flowchart for identifying and addressing underfitting and overfitting.
This technical support center provides resources for researchers and scientists developing Explainable AI (XAI) for parameter estimation in critical fields like drug development. The following guides and FAQs address specific technical issues encountered when making complex AI models transparent and compliant with evolving regulations.
Troubleshooting Guides
Guide 1: Resolving Performance Drops After Enabling Explainability
Problem: After integrating Explainable AI (XAI) techniques into our parameter estimation model, the model's predictive performance (accuracy/F1-score) has significantly decreased.
Root Cause: The process of making a complex "black box" model interpretable can sometimes involve simplifying the model, using surrogate models, or adding constraints that reduce its raw predictive power. There is often a trade-off between absolute accuracy and explainability [51].
Solutions:
- Prioritize Simpler, More Interpretable Models: For high-stakes domains like drug development, start with models that are inherently more interpretable, such as decision trees. Research shows that the C4.5 decision tree algorithm, for instance, has outstanding performance on medical datasets and is highly interpretable [52].
- Use Post-Hoc Explanation Techniques: Instead of building explainability into the model itself, use techniques like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to explain predictions after the fact. These are particularly valuable for understanding complex model decisions in finance and compliance [53].
- Validate with Domain Experts: Ensure the explanations generated align with scientific domain knowledge. A performance metric drop is less critical if the model's reasoning becomes biologically or chemically plausible and can be validated by experts.
Guide 2: Addressing Regulatory "Right to Explanation" Requests
Problem: Regulators have requested a detailed explanation for a specific AI-driven decision (e.g., why a specific compound was flagged as toxic). The model used is a complex deep learning network, and providing a clear explanation is challenging.
Root Cause: Regulations, such as the EU AI Act, mandate transparency for high-risk AI systems. Opaque models can lead to non-compliance, with penalties reaching up to €35 million [53]. The "right to explanation" is a legal requirement in many jurisdictions [51].
Solutions:
- Implement a Layered Explanation Strategy:
- Layer 1: Provide a high-level, user-friendly summary of the main factors influencing the decision.
- Layer 2: Offer a more detailed technical explanation, such as a feature importance score (e.g., from SHAP analysis), suitable for internal reviewers and regulators [53].
- Maintain an Audit Trail: Keep detailed records of the model's development data, versioning, and hyperparameters. This demonstrates a commitment to transparency and provides context for its decisions [51].
- Conduct a Pre-emptive Algorithmic Audit: Proactively audit your AI systems for bias, fairness, and explainability to identify and remediate potential issues before they are flagged by regulators [53].
Guide 3: Mitigating Data Privacy Risks from Model Explanations
Problem: The security team warns that the detailed feature attributions provided by our XAI system could potentially be used to reverse-engineer sensitive training data or proprietary model parameters.
Root Cause: XAI techniques can inadvertently create vulnerabilities. Model inversion or membership inference attacks can exploit these explanations to extract private information, creating a conflict between transparency and privacy [51].
Solutions:
- Apply Differential Privacy (DP): Use DP mechanisms during model training. This adds carefully calibrated noise to the data or the optimization process, providing a mathematical guarantee of privacy and making it difficult to infer information about any individual data point from the model's outputs or explanations [51].
- Use Federated Learning (FL): Train the model across decentralized data sources (e.g., different research labs) without exchanging the raw data. This helps preserve privacy by keeping data localized, and XAI techniques can often be applied to the aggregated model [51].
- Sanitize Explanatory Outputs: Before sharing explanations, review and filter them to ensure they do not reveal overly specific information about the training data distribution or unique model weights.
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between an interpretable model and an explained "black box" model? A1: An interpretable model (e.g., a short decision tree or linear regression) is inherently transparent; its structure and parameters are directly understandable. An explained "black box" model (e.g., a deep neural network) remains complex, but we use post-hoc techniques like SHAP or LIME to generate approximate, often local, explanations for its specific predictions [53].
Q2: Our team uses advanced optimization algorithms for parameter estimation. Are there specific XAI techniques for these models? A2: Yes. Meta-heuristic optimization algorithms, like the Improved Mountain Gazelle Optimizer (i_MGO) used for photovoltaic parameter estimation, can benefit from XAI [19]. You can apply XAI to analyze which parameters most significantly influence the optimization outcome or to explain the behavior of a surrogate model that approximates your complex objective function, making the optimization process itself more transparent.
Q3: How can we balance the trade-off between model explainability and performance? A3: This is a core strategic decision. The table below summarizes the key trade-offs to guide your approach [53] [51].
Table 1: Balancing Explainability and Performance in AI Models
| Aspect | Highly Explainable Models | High-Performance "Black Box" Models |
|---|---|---|
| Typical Examples | Decision Trees (e.g., C4.5), Linear Models [52] | Deep Neural Networks, Complex Ensembles |
| Advantages | Easier to debug, validate, and gain regulatory approval; inherent transparency [52]. | Often higher accuracy on complex, high-dimensional data (e.g., molecular structures). |
| Disadvantages | May be too simplistic for complex phenomena, leading to lower accuracy. | Difficult to trust and validate; poses regulatory and ethical risks [53]. |
| Best Use Case | Critical processes where reasoning is as important as outcome (e.g., clinical trial analysis). | Tasks where prediction accuracy is paramount and the model's reasoning is secondary. |
Q4: What are the key regulatory requirements for XAI in drug development? A4: While specific regulations are evolving, the core principles from frameworks like the EU AI Act require that AI systems in high-risk areas, including healthcare, must be:
- Transparent and Explainable: You must be able to trace and communicate the logic behind AI decisions.
- Auditable: Your models and processes must allow for independent verification.
- Supervised by Humans: There must be meaningful human oversight and the ability to override AI decisions [53].
Experimental Protocol for XAI Implementation
This protocol provides a step-by-step methodology for integrating explainability into a parameter estimation model for a drug efficacy prediction task.
1. Define Explainability Requirements: * Stakeholder Interview: Consult with regulatory affairs, clinical scientists, and bioethicists. * Output: A document specifying the required level of explanation (e.g., global model behavior vs. individual prediction rationale) and the target audience (e.g., regulators, scientists).
2. Data Preprocessing and Feature Selection: * Method: Use SHAP or a similar technique on a preliminary model to identify the most important biochemical and physiological features driving the prediction. * Goal: Reduce dimensionality to improve both model performance and interpretability.
3. Model Selection and Training with Explainability in Mind: * Approach: Start with an inherently interpretable model like C4.5 [52]. If performance is insufficient, move to a more complex model (e.g., XGBoost or Neural Network) with plans for post-hoc explanation. * Hyperparameter Tuning: Optimize for performance and stability. Research indicates that for many datasets, default parameters can be sufficient, saving tuning time [52].
4. Generate and Validate Explanations: * Action: Apply selected XAI techniques (e.g., SHAP for feature importance, LIME for local explanations). * Validation: Have domain experts (e.g., pharmacologists) review a set of explanations to assess their scientific plausibility and consistency with established knowledge.
5. Documentation and Audit Trail Creation: * Deliverable: Create a model card and comprehensive documentation detailing the model's purpose, performance, limitations, and the XAI methods used. This is crucial for regulatory submissions [53] [51].
The workflow for this protocol is summarized in the diagram below:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Explainable AI and Parameter Estimation Research
| Tool / Technique | Function | Relevance to Parameter Estimation |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | A game-theoretic approach to explain the output of any machine learning model. It provides consistent feature importance values. | Quantifies the contribution of each input parameter (e.g., chemical descriptor) to the final estimated output (e.g., binding affinity). |
| LIME (Local Interpretable Model-agnostic Explanations) | Creates a local, interpretable surrogate model to approximate the predictions of a complex black box model for a specific instance. | Explains why a specific compound received a particular parameter estimate by highlighting local decision boundaries. |
| Decision Trees (C4.5/CART) | An inherently interpretable model that uses a tree-like structure of decisions based on feature thresholds. | Can be used directly as a transparent parameter estimation model or as a surrogate to explain a more complex model [52]. |
| Differential Privacy Tools | Software libraries (e.g., TensorFlow Privacy) that implement algorithms to train models with formal privacy guarantees. | Protects sensitive molecular or patient data during model training, balancing explainability with privacy mandates [51]. |
| Meta-heuristic Optimizers (e.g., MGO) | Algorithms inspired by natural processes to find near-optimal solutions for complex optimization problems. | Used for precise parameter estimation in complex models (e.g., pharmacokinetic models) where traditional methods fail [19]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: My parameter estimation is stuck in a local minimum. What strategies can help escape it? A1: Local minima are a common challenge in complex optimization landscapes. A highly effective strategy is to implement a hybrid approach that combines global and local search methods [54]. Begin with a global metaheuristic, such as a Scatter Search or a Genetic Algorithm, to broadly explore the parameter space and identify promising regions. Once these regions are found, switch to a gradient-based local optimization method (e.g., interior-point or Levenberg-Marquardt) to rapidly converge to a high-quality solution [55]. This combination leverages the robustness of global searches with the speed of local methods.
Q2: I have limited computational resources. Should I use a global or local optimization method? A2: For resource-constrained environments, a well-tuned multi-start of local optimizations is often a successful and efficient strategy [55]. This involves running a local search algorithm from many different starting points in the parameter space. The key is to use a sufficient number of starts to have a high probability of landing in the basin of attraction of the global optimum. The performance of this method has been significantly boosted by advances in efficient gradient calculation using adjoint-based sensitivities [55].
Q3: How can I reduce the computational cost of my high-dimensional biogeochemical (BGC) model? A3: Leveraging physics-based surrogate models is a powerful technique to control costs. For ocean BGC models, a one-dimensional (1D) vertical mixing model can be used as a computationally efficient surrogate for a full 3D simulation [54]. This approach can accurately recover seasonal dynamics and allows for simultaneous parameter estimation across multiple ocean locations and observational variables at a fraction of the computational cost.
Q4: What is the impact of the experimental operating profile on battery model parameter estimation? A4: The choice of operating profile profoundly affects the trade-off between estimation accuracy and computational time [56]. Using a diverse set of profiles (e.g., C/5, C/2, 1C, and Dynamic Stress Test - DST) generally minimizes model voltage output error. However, if time cost is the primary constraint, a simpler profile like a 1C constant current discharge can be used, though it may sacrifice some parameter accuracy [56].
Q5: How can I optimize combination drug therapies without testing all possible doses? A5: Exhaustively testing all drug and dose combinations is computationally infeasible. Search algorithms, such as modified sequential decoding algorithms from information theory, can identify optimal combinations of interventions by testing only a small fraction of the total possibility space [57]. In biological experiments, these algorithms have successfully identified optimal combinations of four drugs using only one-third of the tests required for a full factorial search [57].
Troubleshooting Common Experimental Issues
Issue 1: Poor Parameter Identifiability and Model Overfitting
- Problem: The optimization algorithm finds parameter sets that fit the data well, but the parameters have large uncertainties or are not unique. This often occurs when the model is too complex for the available data.
- Solution:
- Perform Sensitivity Analysis: Identify parameters to which your model outputs are most sensitive. Focus estimation efforts on these key parameters [56].
- Increase Data Diversity: Use experimental data from multiple operating conditions or profiles. For example, in battery modeling, combining constant-current and dynamic profiles provides richer information for constraining different parameters [56].
- Regularization: Introduce penalty terms to your objective function that discourage parameter values from becoming excessively large, which helps prevent overfitting.
Issue 2: Unacceptable Computational Time for a Single Model Evaluation
- Problem: The model simulation itself is so slow that running the thousands of evaluations required for optimization is impractical.
- Solution:
- Simplify the Model: Use a "fit-for-purpose" modeling philosophy [3] [58]. Replace complex mechanistic sub-models with simpler, semi-mechanistic or empirical representations that capture the essential dynamics without unnecessary detail.
- Employ Surrogate Models: Where possible, develop fast, approximate surrogate models (e.g., using machine learning) that can be used in place of the full model during the optimization process.
- Parallelize Evaluations: Many optimization algorithms, especially metaheuristics like Particle Swarm Optimization (PSO) and Genetic Algorithms (GA), are "embarrassingly parallel." Distributing model evaluations across multiple CPU cores or a computing cluster can drastically reduce wall-clock time.
Issue 3: Algorithm Fails to Converge to a Physically Plausible Solution
- Problem: The optimized parameters produce a good fit to the data but are biologically or physically unrealistic (e.g., negative rate constants).
- Solution:
- Implement Hard Constraints: Enforce strict lower and upper bounds on parameters based on prior knowledge (e.g., all kinetic rate constants must be positive) [55].
- Incorporate Prior Information: Use Bayesian inference methods to integrate prior knowledge about parameter distributions into the estimation process, which regularizes the solution towards physically realistic values.
- Re-evaluate Model Structure: The problem may indicate a structural flaw in the model itself. Use the implausible parameters as a diagnostic to revisit and refine the model's mechanistic assumptions.
Performance Comparison of Optimization Methods
The table below summarizes a systematic benchmarking study of optimization methods for parameter estimation in dynamic biological models, highlighting the trade-off between robustness and efficiency [55].
Table 1: Benchmarking Results for Parameter Estimation Methods
| Method Class | Specific Method | Computational Efficiency | Robustness (Success Rate) | Key Characteristics | Best For |
|---|---|---|---|---|---|
| Multi-start Local | Multi-start + Gradient-based (Adjoint) | High | Moderate to High | Fast convergence; performance depends on number of starts [55]. | Well-behaved problems with good initial guesses. |
| Metaheuristic (Global) | Scatter Search | Moderate | High | Effective global exploration; less prone to premature convergence [55]. | Highly non-convex problems with many local minima. |
| Hybrid | Scatter Search + Interior Point (Recommended) | High | Very High | Combines global search of metaheuristic with fast, refined convergence of local method [55]. | Challenging, medium- to large-scale kinetic models. |
| Metaheuristic (Global) | Genetic Algorithm (GA) | Low | Moderate | Good exploration; can be slow to converge [55]. | Problems where global search is critical and time is less limited. |
| Metaheuristic (Global) | Particle Swarm Optimization (PSO) | Moderate | Moderate | Efficient for many problems; can get stuck in local optima [58]. | Medium-scale optimization problems. |
Essential Experimental Protocols
Protocol 1: Hybrid Global-Local Parameter Estimation for Complex Models
This protocol is adapted from high-dimensional ocean biogeochemical model calibration and represents a state-of-the-art approach [54] [55].
- Problem Definition: Formulate the objective function (cost function) that quantifies the mismatch between model outputs and observational data.
- Global Exploration:
- Use a global metaheuristic algorithm (e.g., Scatter Search, PSO, or GA) to perform a broad search of the parameter space.
- Run the algorithm for a predefined number of iterations or until a set of promising, high-quality solutions is identified.
- Local Refinement:
- Select the best parameter sets from the global search phase.
- Use each of these sets as the initial guess for a gradient-based local optimization method (e.g., interior-point, Levenberg-Marquardt).
- The local method will quickly converge to the nearest local minimum from each starting point.
- Solution Selection: From all the locally refined solutions, select the parameter set that results in the lowest value of the objective function as the final, optimized parameters.
Protocol 2: Selecting Optimal Operating Profiles for Efficient Battery Parameter Estimation
This methodology uses systematic profile combination to balance accuracy and time cost [56].
- Generate Basic Profiles: Conduct experiments or simulations to generate voltage/current data under a suite of fundamental operating conditions. Common profiles include:
- Constant Current (CC) discharges at multiple C-rates (e.g., C/5, C/2, 1C).
- Pulse charge/discharge profiles.
- Dynamic Stress Test (DST) profiles.
- Create Profile Combinations: Systematically create different combinations of the basic profiles (e.g., C/5 alone; C/5 and C/2; C/5, C/2, and Pulse; all five profiles).
- Parameter Estimation & Validation: For each profile combination, run your chosen parameter estimation algorithm (e.g., PSO) to identify a parameter set. Then, validate each parameter set against a separate, held-out validation dataset.
- Multi-Criteria Analysis: Evaluate the results based on:
- Model Voltage Output Error (Root Mean Square Error vs. validation data).
- Parameter Estimation Error (if true parameters are known).
- Computational Time Cost for the estimation.
- Select Optimal Profile: Choose the profile combination that best meets your specific need (e.g., minimal error, minimal time, or the best compromise).
Workflow and Pathway Visualizations
Optimization Strategy Selection Workflow
The following diagram outlines a logical workflow for selecting an appropriate optimization strategy based on model characteristics and resource constraints.
Optimization Strategy Selection
Hybrid Global-Local Parameter Estimation Process
This diagram details the sequential process of the hybrid optimization method, which is recommended for robust and efficient parameter estimation.
Hybrid Optimization Process
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Key Computational Tools and Algorithms for Optimization Research
| Tool / Algorithm | Type | Primary Function | Application Context |
|---|---|---|---|
| Scatter Search | Global Metaheuristic | Explores parameter space for promising regions without using gradients [55]. | High-dimensional, non-convex problems; often used in hybrid methods. |
| Interior-Point Method | Local Gradient-Based | Efficiently converges to a local minimum from a good starting point [55]. | Local refinement in a hybrid strategy or for smooth, convex problems. |
| Particle Swarm Optimization (PSO) | Global Metaheuristic | Population-based search inspired by social behavior [56] [59]. | Parameter estimation in electrochemical battery models [56] and molecular optimization [59]. |
| Adjoint Sensitivity Analysis | Mathematical Method | Calculates gradients of objective function with respect to all parameters extremely efficiently [55]. | Enables fast gradient-based local optimization for complex dynamic models. |
| Sequential Decoding Algorithm | Search Algorithm | Efficiently searches vast combinatorial spaces by testing a smart subset of all possibilities [57]. | Optimizing combinations of drugs and doses without full factorial testing [57]. |
| Single Particle Model (SPM) | Physics-Based Surrogate | Simplified electrochemical model for rapid simulation [56]. | Reduces computational cost during parameter estimation for lithium-ion batteries. |
| 1D Vertical Mixing Model | Physics-Based Surrogate | Simplified physical model representing ocean mixing [54]. | Acts as a computationally efficient surrogate for 3D simulations in ocean BGC model calibration. |
Benchmarking Success: Validating and Comparing Optimization Algorithms for Regulatory Readiness
Core Concepts: Troubleshooting Guide
Q1: My model performs well on training data but fails on new data from a different hospital scanner. What is happening and how can I fix it?
A: This is a classic sign of poor generalizability, often caused by a domain shift between your training data and the new clinical environment [60] [61]. The model has likely learned features specific to your original scanner's imaging protocol rather than universally relevant patterns.
- Diagnosis: The model is overfitting to the source domain's data distribution.
- Solution: Implement Domain Adaptation techniques [60] [61]. Focus on learning features that are invariant across different scanners and acquisition protocols. Data Augmentation during training is also critical; simulate variations in contrast, noise, and resolution to make the model resilient to scanner heterogeneity [60] [61].
Q2: How can I proactively find my model's weaknesses before deployment in a high-stakes environment like drug solubility prediction?
A: You should perform a robustness validation focused on "weak robust samples" [62].
- Diagnosis: Standard validation on a clean test set fails to expose vulnerabilities to minor input perturbations.
- Solution: Isolate the most vulnerable samples from your training set—those where small perturbations cause misclassifications. Evaluate your model on these perturbed weak samples to identify the specific corruption or adversarial types (e.g., Gaussian noise, motion artifacts) that cause failure. Use these insights to guide targeted data augmentation [62].
Q3: For my cancer patient prediction model, performance has dropped over time. What could be the cause?
A: This indicates model drift, a common issue in dynamic real-world environments like healthcare [63]. The underlying data distribution has likely changed over time due to new medical practices, updated EHR coding, or shifts in patient populations.
- Diagnosis: Temporal dataset shift causing a disconnect between the model's training data and current reality.
- Solution: Implement a temporal validation framework [63]. Instead of a random train-test split, train your model on data from one time period (e.g., 2010-2018) and validate it on data from a subsequent period (e.g., 2019-2022). This simulates real-world deployment and helps assess model longevity. Regular model retraining on recent data may be necessary.
Q4: My classification model for a rare disease has 95% accuracy, but it's missing all positive cases. What metric should I use?
A: Accuracy is a misleading metric for imbalanced datasets [64] [65] [66]. Your model is likely just predicting the majority class.
- Diagnosis: Over-reliance on accuracy with a highly skewed class distribution.
- Solution: Use the F1 Score or PR AUC (Precision-Recall Area Under the Curve) [64]. The F1 score is the harmonic mean of precision and recall and provides a single measure of a model's effectiveness on the positive class. PR AUC is particularly robust for imbalanced problems as it focuses primarily on the positive class and does not use true negatives in its calculation [64].
Key Metrics for Model Validation
The table below summarizes essential quantitative metrics for evaluating model performance, robustness, and stability.
Table 1: Key Model Evaluation and Validation Metrics
| Metric | Formula / Definition | Use Case | Interpretation |
|---|---|---|---|
| F1 Score [64] [65] | ( F1 = 2 \times \frac{ \text{Precision} \times \text{Recall} }{ \text{Precision} + \text{Recall} } ) | Imbalanced classification; when both false positives and false negatives are costly. | Harmonic mean of precision & recall. Higher is better (max 1). |
| ROC AUC [64] [65] | Area Under the Receiver Operating Characteristic curve. | Balanced classification; evaluating overall ranking performance of a model. | Probability a random positive is ranked higher than a random negative. Higher is better (max 1). |
| PR AUC [64] | Area Under the Precision-Recall curve. | Imbalanced classification; focus on performance of the positive class. | Average precision across all recall thresholds. Higher is better (max 1). |
| R² Score [66] [67] | ( R^2 = 1 - \frac{SS{res}}{SS{tot}} ) | Regression tasks (e.g., predicting drug solubility or solvent density). | Proportion of variance in the target variable explained by the model. Closer to 1 is better. |
| Static Canonical Trace Divergence (SCTD) [68] | Divergence between static opcode distributions of generated code solutions. | Quantifying algorithmic structure diversity in LLM-generated code. | Lower values indicate higher structural stability among functionally correct solutions. |
| Dynamic Canonical Trace Divergence (DCTD) [68] | Divergence between runtime opcode traces of solutions across test cases. | Quantifying runtime behavioral variance in generated code. | Lower values indicate more consistent runtime performance. |
Experimental Protocols for Robustness & Generalization
Protocol 1: Temporal Validation for Clinical Models
This protocol, derived from a framework for validating models on cancer patient data, assesses model performance over time to ensure longevity [63].
- Data Splicing by Time: Split your dataset chronologically by patient index date (e.g., treatment start date). For example, use data from 2010-2018 for training and 2019-2022 for testing [63].
- Feature Engineering: Extract features from a fixed window (e.g., 180 days) prior to each patient's index date. Use the most recent value for each feature and one-hot encode categorical variables [63].
- Model Training with Cross-Validation: Train multiple models (e.g., LASSO, Random Forest, XGBoost) on the training period. Optimize hyperparameters using nested cross-validation within the training set [63].
- Temporal Performance Assessment: Evaluate the best model on the held-out future test set. Compare performance (using F1, AUC, etc.) against the internal validation score to quantify performance degradation [63].
Protocol 2: Identifying Weak Robust Samples for Targeted Augmentation
This protocol helps expose model vulnerabilities by finding easily perturbed samples in the training set [62].
- Per-Input Robustness Analysis: For each sample in your training set, generate multiple perturbed versions ("neighbors") using small variations (e.g., minor noise, contrast changes) [62].
- Identify Weak Samples: Rank training instances by their robustness score—the proportion of perturbed neighbors that are misclassified. The samples with the lowest scores are your "weak robust samples" [62].
- Perturbation Benchmarking: Systematically apply a battery of adversarial and common corruption perturbations to these weak samples. Identify the specific perturbation types that cause the highest error rates [62].
- Targeted Robustness Enhancement: Retrain the model using an augmented dataset that includes these non-robust perturbation types, specifically targeting the model's weaknesses [62].
Conceptual & Workflow Diagrams
Model Validation Workflow
Pillars of Model Robustness
The Scientist's Toolkit: Research Reagents & Solutions
Table 2: Essential Tools for Validation and Robustness Experiments
| Tool / Technique | Category | Function in Validation |
|---|---|---|
| Scikit-learn [66] | Software Library | Provides standard metrics, cross-validation splitters, and preprocessing tools for model validation. |
| Stratified K-Fold [66] | Validation Technique | Preserves class distribution across folds, essential for reliable validation on imbalanced datasets. |
| LASSO (L1 Regularization) [60] [61] | Regularization Technique | Prevents overfitting by promoting sparsity; useful for feature selection in high-dimensional data. |
| Random Forest / Extra Trees [67] | Ensemble Model | Improves robustness by combining multiple decision trees, reducing variance and overfitting. |
| Weak Robust Samples [62] | Diagnostic Concept | Serve as sensitive indicators of model vulnerability, enabling targeted performance enhancement. |
| Domain Adaptation [60] [61] | ML Strategy | Minimizes performance drop by aligning feature distributions across different domains (e.g., hospitals). |
| Whale Optimization Algorithm (WOA) [67] | Optimization Algorithm | Tunes model hyperparameters effectively, as demonstrated in drug solubility prediction tasks. |
Troubleshooting Guides
FAQ: How do I choose between a metaheuristic (PSO/GA) and Deep Learning for my parameter estimation problem?
Answer: The choice depends on your data characteristics, problem complexity, and computational constraints. The following table summarizes the key decision factors:
| Factor | Particle Swarm Optimization (PSO) | Genetic Algorithm (GA) | Deep Learning (DL) |
|---|---|---|---|
| Primary Strength | Global search in complex, non-convex spaces [69] [70] | Handling non-differentiable, discontinuous functions [71] | Learning complex, non-linear patterns from large datasets [72] [73] |
| Optimal Use Case | Kinetic parameter fitting for oligomerization equilibria [70] | Hyperparameter tuning for other algorithms [71] | Drug-target binding (DTB) and affinity (DTA) prediction [72] |
| Data Requirement | Low; effective with limited experimental data [70] | Low to Moderate [71] | Very High; requires large datasets for training [72] [73] |
| Key Advantage | Makes few assumptions about the problem; does not require the function to be differentiable [70] | Resistant to getting trapped in local optima compared to gradient-based methods [71] | Automates feature extraction and learns intricate relationships without manual curation [72] |
FAQ: My deep learning model has poor performance. What are the first steps to diagnose the issue?
Answer: Poor DL model performance is often due to implementation bugs, hyperparameter choices, or data issues [74]. Follow this structured debugging workflow:
- Start Simple: Begin with a simple architecture (e.g., a fully-connected network with one hidden layer), use sensible defaults like ReLU activation, and normalize your inputs [74].
- Overfit a Single Batch: A critical heuristic to catch bugs. Try to drive the training error on a single, small batch of data arbitrarily close to zero. Failure to do so indicates potential problems [74]:
- Error Explodes: Often a numerical instability issue or a learning rate that is too high.
- Error Oscillates: Lower the learning rate and inspect your data labels.
- Error Plateaus: Increase the learning rate, remove regularization, and inspect the loss function.
- Check for Common Bugs: The five most common bugs in deep learning are [74]:
- Incorrect tensor shapes.
- Incorrect input pre-processing (e.g., forgetting to normalize).
- Incorrect input to the loss function.
- Forgetting to set the model to train/evaluation mode correctly.
- Numerical instability (e.g.,
inforNaNoutputs).
FAQ: My PSO/GA is converging to a suboptimal solution. How can I improve it?
Answer: Premature convergence is a known challenge for metaheuristics. For PSO, several advanced strategies have been developed to address this [69]:
- Adaptive Learning Strategies: Use algorithms that dynamically adjust search strategies based on complexity, such as the Comprehensive Learning PSO (CLPSO) or adaptive learning strategy PSO [69].
- Multiple Swarms: Implement multi-swarm or multi-sample approaches, where several sub-swarms explore different regions of the parameter space simultaneously, preventing the entire population from getting stuck [69].
- Hybrid Algorithms: Combine PSO with a local search method. For instance, using linear gradient descent after PSO has found a promising region can refine the solution and increase robustness, as demonstrated in the analysis of HSD17β13 enzyme kinetics [70].
For Genetic Algorithms, the principle of maintaining population diversity is key. This can be achieved by carefully tuning crossover and mutation rates to prevent the premature dominance of suboptimal genetic traits [71].
Experimental Protocols & Performance Data
Quantitative Performance Metrics in Drug Discovery
The table below summarizes real-world performance metrics for different algorithms across various pharmaceutical applications, highlighting their quantitative impact.
| Application Area | Algorithm Class | Specific Model / Technique | Key Performance Metric & Result | Source / Validation |
|---|---|---|---|---|
| CEO Compensation Prediction | Deep Learning + PSO | DNN optimized with PSO | MSE: 0.0458, R²: 0.9853 (Superior performance) [75] | Comparative analysis of financial models [75] |
| CEO Compensation Prediction | Deep Learning + GA | DNN optimized with GA | Ranked second in predictive performance after PSO-optimized DNN [75] | Comparative analysis of financial models [75] |
| Small-Molecule Drug Discovery | Deep Learning | Generative AI (GANs, VAEs) | >75% hit validation rate in virtual screening [73] | Experimental validation [73] |
| Antibody Engineering | Deep Learning | AI-driven affinity maturation | Enhanced antibody binding affinity to the picomolar range [73] | In vitro validation [73] |
| Enzyme Kinetics (HSD17β13) | Particle Swarm Optimization | PSO with Linear Gradient Descent | Identified global minimum for complex oligomerization equilibrium model [70] | Validation via mass photometry data [70] |
| Drug-Target Binding (DTB) | Deep Learning | Graph-based & Attention-based models | Superior accuracy in predicting drug-target interactions and affinity [72] | Benchmarking on standard datasets [72] |
Detailed Protocol: Applying PSO to Protein Kinetics
This protocol is adapted from a study that used PSO to understand the mechanism of HSD17β13 enzyme inhibitors [70].
Objective: To determine the set of kinetic parameters that best explain experimental Fluorescent Thermal Shift Assay (FTSA) data for a protein-inhibitor system involving complex oligomerization.
Materials and Reagents:
- Protein of Interest: Purified HSD17β13 enzyme.
- Ligand/Inhibitor: The small-molecule inhibitor under investigation.
- Fluorescent Dye: A dye like SYPRO Orange that binds to hydrophobic protein regions exposed upon unfolding.
- Real-time PCR Instrument or Thermal Cycler: To perform the thermal shift assay and measure fluorescence.
Methodology:
- Experimental Data Collection:
- Perform FTSA by heating protein samples with and without increasing concentrations of the inhibitor while monitoring fluorescence.
- Record the melting curves (fluorescence vs. temperature) for each condition.
Model Formulation:
- Develop a kinetic scheme that defines the protein's oligomerization states (e.g., monomer, dimer, tetramer) and their equilibria, both with and without inhibitor binding.
Parameter Optimization with PSO:
- Initialization: Define a search space for each unknown parameter in the model. Place a "swarm" of particles at random locations within this multi-dimensional parameter space.
- Iteration:
- Each particle calculates the error (e.g., sum of squared residuals) between the melting curve predicted by its current parameter set and the actual experimental data.
- Each particle remembers its own best position (lowest error) and communicates with neighboring particles to know the swarm's best position.
- Particles update their velocities and positions based on a combination of their own memory and the swarm's collective knowledge.
- Termination: The process repeats until particles converge on the parameter set that minimizes the error across all melting curves, identifying the global optimum.
Validation:
- Validate the PSO-derived model and parameters using an orthogonal technique, such as mass photometry, to confirm the predicted shift in oligomerization equilibrium [70].
Workflow Diagram: PSO for Kinetic Parameter Estimation
The following diagram illustrates the iterative workflow of using PSO for parameter estimation in a biochemical context.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Algorithm-Assisted Research | Key Consideration |
|---|---|---|
| Purified Target Protein | The primary reagent for biophysical assays (e.g., FTSA) to study binding and stability. | Purity and correct folding are critical for generating reliable data for algorithm training/validation [70]. |
| Small-Molecule Compound Library | A collection of compounds for high-throughput screening to generate bioactivity data. | Diversity and quality of the library directly impact the performance of AI-driven virtual screening models [73]. |
| Fluorescent Dye (e.g., SYPRO Orange) | Binds to unfolded protein in FTSA, allowing measurement of thermal stability shifts upon ligand binding. | The source and batch consistency can affect the reproducibility of the melting curves used for parameter fitting [70]. |
| Benchmark Datasets (e.g., for DTB) | Standardized public datasets (e.g., BindingDB) used to train, test, and compare deep learning models for drug-target prediction. | Dataset size, quality, and the relevance of negative instances are crucial for model accuracy and generalizability [72]. |
| High-Performance Computing (HPC) Cluster | Provides the computational power needed for training large deep learning models or running extensive PSO/GA simulations. | Essential for managing the computational burden of complex models and achieving practical iteration times [72] [73]. |
This technical support center provides troubleshooting guides and FAQs to help researchers and drug development professionals navigate the regulatory landscape for AI-enhanced models, particularly in the context of using optimization algorithms for parameter estimation.
Frequently Asked Questions (FAQs)
1. What is the core framework the FDA uses to evaluate AI models for drug development?
The U.S. Food and Drug Administration (FDA) has proposed a risk-based credibility assessment framework for evaluating AI models used in the drug and biological product lifecycle [76] [77]. This framework is designed to establish trust in an AI model's output for a specific Context of Use (COU). The process consists of seven key steps [76] [78]:
- Define the question of interest.
- Define the COU for the AI model.
- Assess the AI model risk.
- Develop a plan to establish the credibility of the AI model output.
- Execute the plan.
- Document the results in a credibility assessment report.
- Determine the adequacy of the AI model for the COU.
2. My AI model is continuously learning and improving. How do I manage this with regulators?
Both the FDA and EMA emphasize lifecycle management for AI models [76] [79]. You are expected to have a plan to monitor and ensure the model's performance and fitness for use throughout its intended life cycle [76]. For the FDA, this plan should be part of your pharmaceutical quality system. Significant changes that impact performance are expected to be reported per regulatory requirements [76]. The EMA also highlights the need for performance monitoring and validation of AI systems used in the medicinal product lifecycle [79].
3. When should I engage with regulators about my AI model?
Early engagement is strongly encouraged by both the FDA and EMA [76] [80]. The FDA recommends that sponsors discuss their AI model development and use plans with the agency early on. This helps set expectations for credibility assessments, identify potential challenges, and facilitate a timely review [76]. The EMA similarly encourages qualification and early dialogue for novel AI methodologies [79].
4. Are there any real-world examples of AI models being accepted by regulators?
Yes. The European Medicines Agency (EMA) has issued its first qualification opinion on an AI methodology (AIM-NASH), accepting clinical trial evidence generated by an AI tool that assists pathologists in analyzing liver biopsy scans [79]. In the U.S., the UVA/Padova Type 1 Diabetes Simulator, a sophisticated in silico platform, has been accepted by the FDA to support regulatory decisions for continuous glucose monitoring devices [81].
5. What are the biggest challenges regulators have identified with AI models?
Regulators have pinpointed several key challenges that your model must address [80]:
- Data Variability: Risk of bias from variations in training data quality and representativeness.
- Transparency: Difficulty in interpreting the internal workings of complex models ("black box" problem).
- Uncertainty Quantification: Challenges in accurately explaining or quantifying the precision of model outputs.
- Model Drift: The potential for model performance to degrade over time or in new environments.
Troubleshooting Common Regulatory Challenges
| Problem Area | Symptom | Potential Root Cause | Recommended Solution |
|---|---|---|---|
| Model Risk Assessment | Regulators classify your model as "high risk," demanding extensive validation. | The model's output makes a final determination without human intervention on critical safety issues [76]. | Implement human-in-the-loop review for high-consequence decisions. Document how human oversight mitigates risk [76]. |
| Data & Transparency | Inability to explain model outputs or demonstrate training data representativeness. | Use of complex "black box" models without explainability methods; non-representative training data [80]. | Integrate Explainable AI (XAI) techniques. Perform rigorous bias testing and document data provenance and characteristics [80]. |
| Lifecycle Management | Model performance degrades after deployment; regulators question update process. | Lack of a robust monitoring and maintenance plan for data and concept drift [76]. | Develop a detailed lifecycle maintenance plan, including performance monitoring triggers and a pre-specified change control plan [76] [80]. |
| Regulatory Submission | Uncertainty about what documentation to submit and when. | The regulatory guidance is draft and principles-based, lacking specific submission templates [76] [78]. | Engage early with the FDA via existing pathways (e.g., pre-IND) to agree on "whether, when, and where" to submit the credibility assessment report [76]. |
| Intellectual Property | Concern that transparency requirements will force disclosure of trade secrets. | Need to disclose model architecture, data, or training procedures to establish credibility [81]. | Use a tiered data governance strategy: modularize model components, validate on public datasets, and strengthen patent protection for novel workflows [81]. |
Experimental Protocol for AI Model Credibility Assessment
This protocol outlines the core methodology based on the FDA's risk-based framework, essential for validating AI models used in parameter estimation for regulatory submissions.
1. Define Context of Use (COU) and Question of Interest
- Objective: Precisely specify the role of the AI model and the regulatory question it will help answer.
- Procedure: Formulate a specific question (e.g., "What is the predicted incidence of adverse event X in patient population Y?"). The COU must detail what is being modeled, the input data, the output, and how the output will inform the decision, including if it will be used alone or with other evidence [76].
2. Develop a Risk Assessment Plan
- Objective: Determine the level of scrutiny and validation required.
- Procedure: Evaluate risk based on two factors [76] [81]:
- Model Influence: How much does the AI output directly determine the decision? (Higher risk if it is the sole determinant).
- Decision Consequence: What is the impact of a wrong decision on patient safety or product quality?
- Documentation: Classify the model risk as low, medium, or high and justify the classification.
3. Design and Execute the Credibility Assessment Plan
- Objective: Generate evidence to build trust in the model for its COU.
- Procedure: Tailor activities to the model's risk and COU. This typically includes [76]:
- Model Description: Document the architecture, underlying algorithms, and assumptions.
- Data Governance: Describe data sources, preprocessing, and splitting into training, tuning, and test sets.
- Model Evaluation: Define and calculate performance metrics relevant to the COU. Perform sensitivity and uncertainty analysis.
4. Document and Report
- Objective: Create a comprehensive record for internal use and regulatory submission.
- Procedure: Compile a Credibility Assessment Report that includes the defined COU, risk assessment, executed plan, results, and any deviations. Discuss with the FDA early on whether, when, and where this report should be submitted [76].
Workflow Visualization
AI Model Regulatory Preparation Workflow
Research Reagent Solutions: Essential Components for AI Model Development
The following table details key "reagents" or components needed to build a robust AI model for a regulatory submission.
| Research Reagent / Component | Function in the "Experiment" | Regulatory Consideration |
|---|---|---|
| Context of Use (COU) Definition | Precisely scopes the model's purpose, inputs, outputs, and boundaries. | The foundational element for the entire credibility assessment framework. A vague COU will lead to validation challenges [76]. |
| Risk Assessment Matrix | A tool to evaluate model risk based on Influence and Consequence. | Determines the level of evidence and documentation required by regulators. Justifies the rigor of your validation plan [76] [81]. |
| Credibility Assessment Plan | The master protocol detailing how model trustworthiness will be established. | A required document that should be commensurate with model risk. Early agreement with regulators on this plan is advisable [76]. |
| Curated & Documented Datasets | High-quality, representative data split into training, validation, and test sets. | Data quality, provenance, and relevance are critical. Regulators will scrutinize data for potential biases that could affect model performance [76] [80]. |
| Explainable AI (XAI) Techniques | Tools and methods to interpret model outputs and increase transparency. | Addresses the "black box" challenge. Helps demonstrate that the model's operation is understood and its outputs are reliable [80]. |
| Lifecycle Maintenance Plan | A proactive plan for monitoring performance and managing model updates. | Expected by regulators to ensure the model remains fit-for-purpose over time, especially for adaptive models [76] [79]. |
FAQ: Troubleshooting Algorithm Performance and Implementation
Q1: Our AI-designed drug candidates show excellent predicted bioactivity in silico, but consistently fail in early biological assays. What could be the cause?
This is a classic sign of overfitting or a data quality issue. The algorithm may have learned noise or specific patterns from your training data that do not generalize to real-world conditions.
- Root Cause Analysis: The problem likely originates in the training data or model validation process.
- Solution:
- Audit Your Training Data: Ensure your data is high-quality, curated, and as complete as possible. The predictive power of any Machine Learning (ML) approach is dependent on the availability of high volumes of high-quality data [17].
- Implement Robust Validation: Use techniques like hold-back validation sets or resampling methods (e.g., 5-fold cross-validation) to test the model's performance on data it has not seen during training. Regularization methods can also be applied to force the model to generalize and not overfit [17].
- Review Model Interpretability: If using a complex "black-box" model, employ explainability metrics to understand the rationale behind its predictions. The inability to interpret AI decision-making is a known challenge in the field [82].
Q2: We are experiencing significant delays in our drug discovery projects because tuning our model's hyperparameters is extremely time-consuming. How can we optimize this process?
Hyperparameter optimization is a common bottleneck. Research indicates that for many datasets, extensive tuning may be unnecessary.
- Root Cause Analysis: Applying a trial-and-error method for parameter selection without prior knowledge of the algorithm's behavior on different data types.
- Solution: Leverage empirical knowledge from algorithm applicability research. For instance, a study on the C4.5 decision tree algorithm, which performs well on medical datasets, built a knowledge base to recommend hyperparameter values based on dataset characteristics. This approach eliminated unnecessary tuning for over 65% of datasets and achieved an accuracy of over 80% for the hyperparameter optimization value judgment model [52]. Establish a similar internal knowledge base for your most frequently used algorithms.
Q3: Our AI tool, used for predicting clinical trial success, is generating predictions that our stakeholders find difficult to trust. How can we improve confidence in the model's outputs?
The issue often revolves around the lack of interpretability and transparent documentation.
- Root Cause Analysis: A "black box" model where the decision-making process is not clear, leading to justified skepticism.
- Solution:
- Prioritize Explainability: Where possible, use interpretable models or ensure that complex models are accompanied by explainability metrics that clarify how a prediction was derived [83].
- Comprehensive Documentation: Maintain traceable documentation of the entire AI lifecycle. Regulatory guidance, such as the EMA's Reflection Paper, mandates detailed records of data acquisition, transformation, model architecture, and performance [83]. This documentation is critical for both internal trust and regulatory compliance.
- Provide Context with Benchmarks: Compare your model's performance against industry benchmarks. For example, you could state that your model achieves a predictive AUC of 0.81 for phase 3 to approval, which aligns with or exceeds the state-of-the-art [84].
Q4: We want to use AI to predict the probability of our drug's regulatory approval, but our dataset has many missing values. Should we discard the incomplete data points?
Discarding data (complete-case analysis) is typically not the best approach as it can introduce bias and waste valuable information.
- Root Cause Analysis: Incomplete data records are a common challenge in drug development datasets.
- Solution: Implement statistical imputation methods. Research on predicting drug approvals has successfully used imputation to fully exploit datasets with over 140 features. This approach has been shown to outperform complete-case analysis, which typically yields biased inferences and reduces the effective sample size [84].
Quantitative Performance Benchmarks in Real-World Case Studies
The following table summarizes key performance metrics from documented AI-driven drug development programs, providing concrete benchmarks for the industry.
Table 1: Algorithm Performance in Real-World Drug Development Case Studies
| Company / Platform | Therapeutic Area | Algorithm Application | Key Performance Metric | Reported Outcome |
|---|---|---|---|---|
| Insilico Medicine [82] [85] | Idiopathic Pulmonary Fibrosis | Generative AI for target & drug candidate identification | Discovery & Preclinical Timeline | ~18 months (vs. ~5 years traditional) [85] |
| Exscientia [85] | Oncology (CDK7 inhibitor) | AI-driven lead optimization | Compounds Synthesized | 136 compounds to candidate (vs. thousands traditionally) [85] |
| Exscientia [85] | General Drug Design | AI-powered design cycles | Design Cycle Efficiency | ~70% faster, requiring 10x fewer synthesized compounds [85] |
| Industry-wide Analysis [82] | Multiple | AI-discovered drugs in clinical trials | Phase 1 Trial Success Rate | 80-90% (vs. 40-65% for conventional drugs) |
| Machine Learning Model [84] | Multiple (Pipeline Analysis) | Predicting drug approval from Phase 3 | Predictive Accuracy (AUC) | 0.81 AUC for Phase 3 to approval [84] |
| Machine Learning Model [84] | Multiple (Pipeline Analysis) | Predicting drug approval from Phase 2 | Predictive Accuracy (AUC) | 0.78 AUC for Phase 2 to approval [84] |
Experimental Protocol: Predictive Modeling for Drug Approval
This protocol outlines the methodology for building a machine learning model to predict the probability of regulatory drug approval, based on the research by [84].
1. Objective: To construct a classifier that can predict the eventual approval of a drug-indication pair based on features known after the conclusion of its Phase 2 (or Phase 3) clinical trials.
2. Data Acquisition and Preprocessing:
- Data Sources: Utilize comprehensive commercial pharmaceutical pipeline databases (e.g., Pharmaprojects for drug information, Trialtrove for clinical trial information) [84].
- Feature Engineering: Extract a wide range of potential predictive features (e.g., >140 features), including:
- Trial Outcomes: Objective response rates, trial status.
- Trial Logistics: Accrual rates, trial duration.
- Drug Characteristics: Prior approval for another indication, drug compound attributes.
- Sponsor Information: Sponsor's historical track record [84].
- Data Cleaning and Imputation:
- Apply statistical imputation methods to handle missing data. Do not discard incomplete cases, as this can introduce bias and reduce dataset size [84].
- Define "success" (e.g., registration and launch) and "failure" (e.g., suspension, termination) outcomes clearly.
3. Model Training and Validation:
- Algorithm Selection: Employ appropriate machine learning techniques (e.g., tree-based algorithms, regression models).
- Validation Framework: Use a robust cross-validation scheme for training and a held-out testing set for final performance evaluation [84].
- Performance Metric: Use the Area Under the ROC Curve (AUC) as the primary metric, which estimates the probability that the classifier will rank a positive outcome higher than a negative one [84].
The workflow for this experimental protocol is summarized in the following diagram:
The Scientist's Toolkit: Essential Research Reagents & Solutions
This table details key computational and data resources essential for conducting AI-driven drug development research.
Table 2: Key Research Reagent Solutions for AI-Driven Drug Development
| Item / Solution | Function / Application | Specific Example / Note |
|---|---|---|
| Pharmaprojects Database | Provides detailed drug information for feature engineering in predictive models. | Used to extract 31 drug compound attributes [84]. |
| Trialtrove Database | Provides comprehensive clinical trial characteristics for predictive modeling. | Used to extract 113 clinical trial features [84]. |
| TensorFlow / PyTorch | Open-source programmatic frameworks for building and training machine learning models. | Commonly used ML frameworks for high-performance computation [17]. |
| Algorithm Applicability Knowledge Base | Provides recommended hyperparameter values for specific algorithms based on dataset characteristics. | Can reduce unnecessary tuning time; e.g., successful implementation for C4.5 algorithm [52]. |
| Statistical Imputation Software | Addresses missing data in sparse real-world datasets, allowing for full data utilization. | Critical for avoiding biased inferences from complete-case analysis [84]. |
| Cloud & Robotics Infrastructure | Enables closed-loop, automated design-make-test-analyze cycles for generative AI. | E.g., Exscientia's integration of AI "DesignStudio" with robotic "AutomationStudio" on cloud infrastructure [85]. |
Workflow Diagram: AI-Accelerated Drug Discovery from Target to Candidate
The following diagram illustrates the integrated workflow of a modern, AI-driven drug discovery platform, highlighting how algorithms optimize each stage.
Conclusion
The strategic application of optimization algorithms for parameter estimation represents a transformative force in modern drug development, enabling more predictive modeling, reduced development timelines, and increased probability of success. The integration of AI and ML with established mechanistic models creates powerful hybrid approaches that balance predictive power with scientific interpretability—a crucial combination for regulatory acceptance. As the field evolves, future directions will focus on enhanced explainable AI, automated clinical trial simulation, and the delivery of truly personalized medicine through patient-specific predictive modeling. Researchers who master these optimization techniques and navigate their implementation challenges will be best positioned to accelerate the development of innovative therapies for patients in need.
References
- 1. New robust two-parameter estimator for overcoming ... [https://www.nature.com/articles/s41598-025-12646-8]
- 2. Redefining Parameter Estimation and Covariate Selection ... [https://pubmed.ncbi.nlm.nih.gov/41186137/]
- 3. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 4. Practical Perspectives on Enhancing Predictive Modeling ... [https://link.springer.com/article/10.1007/s40495-025-00426-x]
- 5. Good Practices in Model‐Informed Drug Discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4809625/]
- 6. Regulatory considerations for successful implementation of ... [https://www.nature.com/articles/s41746-025-01513-5]
- 7. "Parameter estimation and optimization for biological ... [https://repository.lsu.edu/gradschool_theses/5249/]
- 8. Back-propagation algorithm converging too quickly to poor ... [https://stackoverflow.com/questions/26542547/back-propagation-algorithm-converging-too-quickly-to-poor-results]
- 9. Vanishing and Exploding Gradients Problems in Deep ... [https://www.geeksforgeeks.org/deep-learning/vanishing-and-exploding-gradients-problems-in-deep-learning/]
- 10. Automated drug design for druggable target identification ... [https://www.nature.com/articles/s41598-025-18091-x]
- 11. Gradient Genetic Algorithm For Drug Molecular Design [https://openreview.net/forum?id=kFKcktAeEG]
- 12. Adaptive Parameter Tuning of Evolutionary Computation ... [https://link.springer.com/article/10.1007/s12561-025-09500-w]
- 13. Prioritize Algorithm Errors: A Step-by-Step Troubleshooting ... [https://www.linkedin.com/advice/1/youre-faced-multiple-algorithm-errors-how-do-you-decide-tu66f]
- 14. A two stage differential evolution algorithm for parameter ... [https://www.nature.com/articles/s41598-025-89304-6]
- 15. The Do's and Don'ts of choosing an Optimization Problem ... [https://sites.gatech.edu/omscs7641/2024/02/19/navigating-the-optimization-landscape-the-dos-and-donts-of-choosing-an-optimization-problem/]
- 16. Estimating the Cost of Industry Investment in Drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8855407/]
- 17. Applications of machine learning in drug discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6552674/]
- 18. Troubleshoot Online Parameter Estimation - MATLAB & ... [https://www.mathworks.com/help/ident/ug/troubleshoot-online-parameter-estimation.html]
- 19. Parameter estimation of photovoltaic models based on ... [https://www.frontiersin.org/journals/energy-research/articles/10.3389/fenrg.2025.1464011/full]
- 20. Enhanced artificial satellite search algorithm with memory ... [https://www.nature.com/articles/s41598-025-24760-8]
- 21. 9 Frequently Misunderstood Concepts in PK/PD Modeling [https://www.certara.com/knowledge-base/9-frequently-misunderstood-concepts-in-pkpd-modeling/]
- 22. Machine Learning for PK/PD Modeling in Drug Development [https://www.certara.com/blog/machine-learning-for-pk-pd-modeling-in-drug-development/]
- 23. Machine Learning and Artificial Intelligence in PK‐PD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11146679/]
- 24. Optimization Algorithms in Machine Learning [https://medium.com/@koushikkushal95/optimization-algorithms-in-machine-learning-a-comprehensive-guide-to-understand-the-concept-and-3db1df7a2f59]
- 25. Overcoming PK/PD Modeling Challenges [https://www.pharmtech.com/view/overcoming-pk-pd-modeling-challenges]
- 26. Artificial Intelligence for Drug Development [https://www.fda.gov/about-fda/center-drug-evaluation-and-research-cder/artificial-intelligence-drug-development]
- 27. Frequently Asked Questions [https://www.pharmacy.umaryland.edu/academics/ai-drug-development/faq/]
- 28. Artificial-intelligence-driven Innovations in Mechanistic ... [https://www.sciencedirect.com/science/article/abs/pii/S0022283625002475]
- 29. The dawn of a new era: can machine learning and large ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170689/]
- 30. Scale-up of complex molecular reaction system by hybrid ... [https://www.nature.com/articles/s41467-025-63982-2]
- 31. Understanding Mechanistic Interpretability in AI Models [https://intuitionlabs.ai/articles/mechanistic-interpretability-ai-llms]
- 32. Mechanistic Interpretability | Decode Neural Networks | CSA [https://cloudsecurityalliance.org/blog/2024/09/05/mechanistic-interpretability-101]
- 33. Progress of AI-Driven Drug–Target Interaction Prediction and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563295/]
- 34. A New Hyperparameter Tuning Framework for Regression ... [https://www.mdpi.com/2227-7390/12/24/3892]
- 35. A Comparative Analysis of Hyper-Parameter Optimization ... [https://www.mdpi.com/2076-3417/15/6/3393]
- 36. Lead Optimization in Drug Discovery [https://chem-space.com/news/chemspace-lead-otimization]
- 37. the Future of Lead Optimization: Benchmarking Compound ... [https://chemrxiv.org/engage/chemrxiv/article-details/686b04ffc1cb1ecda0741680]
- 38. Clinical Trial Simulation and the Art of Adaptive Design ... [https://www.berryconsultants.com/resource/clinical-trial-simulation-and-the-art-of-adaptive-design-optimization]
- 39. Parameter identification for PDEs using sparse interior data ... [https://www.nature.com/articles/s41598-025-02410-3]
- 40. Parameter Estimation of Noise-Disturbed Multivariate ... [https://www.mdpi.com/2227-9717/13/3/773]
- 41. Single-image signal-dependent noise parameter ... [https://www.sciencedirect.com/science/article/abs/pii/S0925231225021071]
- 42. Picard Iteration for Parameter Estimation in Nonlinear ... [https://arxiv.org/abs/2412.20216]
- 43. IT Problem-Solving: Part 1. The Scientific Method - ACA Group [https://acagroup.be/en/blog/it-problem-solving-part-1-the-scientific-method/]
- 44. Underfitting vs. Overfitting in Machine Learning [https://www.ayadata.ai/a-guide-to-overfitting-and-underfitting-in-machine-learning/]
- 45. What is Overfitting? | IBM [https://www.ibm.com/think/topics/overfitting]
- 46. How to Fix Overfitting and Underfitting | by Tahir | Oct, 2025 [https://medium.com/@tahirbalarabe2/how-to-fix-overfitting-and-underfitting-4cf8f383ea96]
- 47. Overfitting in Machine Learning Explained [https://aws.amazon.com/what-is/overfitting/]
- 48. How to Mitigate Overfitting by Creating Ensembles [https://www.geeksforgeeks.org/machine-learning/how-to-mitigate-overfitting-by-creating-ensembles/]
- 49. A Generalization Error Reducing Parameter Estimation Method [https://pmc.ncbi.nlm.nih.gov/articles/PMC8621511/]
- 50. Quantifying, Understanding, and Improving Generalization ... [https://kilthub.cmu.edu/articles/thesis/Quantifying_Understanding_and_Improving_Generalization_in_Deep_Learning/30004975]
- 51. Balancing explainability and privacy in AI systems [https://www.sciencedirect.com/science/article/abs/pii/S0007681325001715]
- 52. Research on parameter selection and optimization of C4.5 ... [https://www.nature.com/articles/s41598-025-11901-2]
- 53. Explainable AI (XAI) in 2025: How to Trust AI ... - Blog de Bismart [https://blog.bismart.com/en/explainable-ai-business-trust]
- 54. Computationally efficient parameter estimation for high ... - GMD [https://gmd.copernicus.org/articles/17/621/2024/]
- 55. Benchmarking optimization methods for parameter estimation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6394396/]
- 56. Optimizing Parameter Estimation for Electrochemical ... [https://arxiv.org/html/2503.00604v2]
- 57. Search Algorithms as a Framework for the Optimization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2590660/]
- 58. How to mathematically optimize drug regimens using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5847021/]
- 59. Molecule discovery and optimization via evolutionary ... [https://www.nature.com/articles/s41598-024-75515-w]
- 60. Strategies to Improve the Robustness and Generalizability ... [https://www.mdpi.com/2673-7426/5/2/20]
- 61. Strategies to Improve the Robustness and Generalizability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12014193/]
- 62. A Validation Strategy for Deep Learning Models [https://arxiv.org/html/2509.19197v1]
- 63. Diagnostic framework to validate clinical machine learning ... [https://www.nature.com/articles/s43856-025-00965-w]
- 64. F1 Score vs ROC AUC vs Accuracy vs PR AUC [https://neptune.ai/blog/f1-score-accuracy-roc-auc-pr-auc]
- 65. 12 Important Model Evaluation Metrics for Machine ... [https://www.analyticsvidhya.com/blog/2019/08/11-important-model-evaluation-error-metrics/]
- 66. AI Model Validation: Ensuring Accuracy & Reliability in AI [https://www.testriq.com/blog/post/model-validation-for-ai-applications]
- 67. Machine learning estimation and optimization for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521650/]
- 68. Dynamic Stability of LLM-Generated Code [https://arxiv.org/html/2511.07463v1]
- 69. Cumulative Major Advances in Particle Swarm ... [https://link.springer.com/article/10.1007/s11831-024-10185-5]
- 70. Application of particle swarm optimization to understand ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10201303/]
- 71. A Complete Guide to Genetic Algorithm — Advantages ... [https://medium.com/@byanalytixlabs/a-complete-guide-to-genetic-algorithm-advantages-limitations-more-738e87427dbb]
- 72. A survey on deep learning for drug-target binding prediction [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451107/]
- 73. Applications of Artificial Intelligence in Biotech Drug Discovery ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308071/]
- 74. Lecture 7: Troubleshooting Deep Neural Networks [https://fullstackdeeplearning.com/spring2021/lecture-7/]
- 75. Genetic Algorithm and Particle Swarm Optimization [https://www.bmfopen.com/index.php/bmfopen/article/view/177]
- 76. Key takeaways from FDA ’s draft guidance on use of AI in drug and... [https://www.dlapiper.com/en-us/insights/publications/2025/01/fda-releases-draft-guidance-on-use-of-ai]
- 77. Considerations for the Use of Artificial Intelligence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-use-artificial-intelligence-support-regulatory-decision-making-drug-and-biological]
- 78. Publishes Its First Draft FDA On Use of Artificial Intelligence... Guidance [https://www.goodwinlaw.com/en/insights/publications/2025/01/alerts-lifesciences-aiml-fda-publishes-its-first-draft-guidance]
- 79. Artificial intelligence | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/about-us/how-we-work/data-regulation-big-data-other-sources/artificial-intelligence]
- 80. Regulating the Use of AI in Drug Development: Legal ... [https://www.fdli.org/2025/07/regulating-the-use-of-ai-in-drug-development-legal-challenges-and-compliance-strategies/]
- 81. Navigating FDA ’s Proposed Guidance on AI and Non-Animal Models ... [https://www.jdsupra.com/legalnews/navigating-fda-s-proposed-guidance-on-1756579/]
- 82. AI's Role in Drug Discovery: Top Uses, Real-world Cases ... [https://expertnetworkcalls.com/69/ai-role-in-drug-discovery-top-uses-real-world-cases-challenges]
- 83. The future of AI regulation in drug development: a comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598624/]
- 84. Machine Learning With Statistical Imputation for Predicting ... [https://hdsr.mitpress.mit.edu/pub/ct67j043]
- 85. Leading AI-Driven Drug Discovery Platforms [https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118]